Monday Poster Session
Category: Stomach and Spleen
P4235 - Inability to Regulate Thyroid Hormones as a Unique Presentation of Autoimmune Gastritis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SH
Shaina Hasan, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Shaina Hasan, MD, Amy Doran, MD, Rebecca Haug, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Autoimmune gastritis (AIG) is a relatively rare disease with limited treatment options, and it is often underdiagnosed. There is a strong association between autoimmune thyroid disease and AIG. We present a case of a patient with hypothyroidism who had gradually increasing levothyroxine requirements despite appropriate therapy, eventually found to have AIG.
Case Description/
Methods: A 58-year-old woman with hypothyroidism and pernicious anemia was initially evaluated for persistent iron deficiency anemia. Evaluation included EGD, colonoscopy, and VCE, which demonstrated erosive gastropathy, with gastric biopsy noting chronic gastritis and a reactive gastropathy pattern. Despite therapy, she remained dependent on IV iron infusions, folic acid supplementation, and B12 injections.
She follows with Endocrinology, who initially diagnosed her hypothyroidism twenty years prior and started on her on levothyroxine. She had persistently elevated TSH and low free T4 with only slight improvement in these levels after escalating to high doses of levothyroxine. A subsequent levothyroxine absorption test demonstrated reduced absorption.
Further workup noted persistent iron deficiency, folate deficiency, vitamin D deficiency, and low IgG levels. She tested positive for parietal cell antibody (PCA) and intrinsic factor antibody (IFA), suggestive of autoimmune gastritis. Evaluation of the small bowel with CT enterography was unremarkable, and follow up EGD demonstrated gastric ulcers and atrophy with erosive and reactive gastropathy on pathology. She remains on an oral proton pump inhibitor with referral to hematology for ongoing management of her iron deficiency and pernicious anemia.
Discussion: AIG remains underdiagnosed due to its asymptomatic nature, with more overt symptoms in later stages of disease. It is not until micronutrient and hematological deficiencies manifest that it is considered on the differential.
Our patient’s history of longstanding hypothyroidism with gradually increasing levothyroxine requirements despite appropriate adherence may have been her first manifestation of AIG, as it started several years prior to her initial presentation of persistent iron deficiency anemia. She received her diagnosis of AIG nearly four years later.
Patients with autoimmune thyroid disease and evidence of malabsorption with persistent anemia or vitamin B12 deficiency should be evaluated for AIG, which could help mitigate the diagnostic delay that often occurs in this patient population.
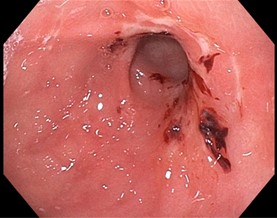
Figure: Gastric ulcers in the antrum
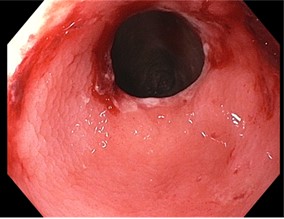
Figure: Gastric atrophy in the pre-pylorus with oozing on contact
Disclosures:
Shaina Hasan indicated no relevant financial relationships.
Amy Doran indicated no relevant financial relationships.
Rebecca Haug indicated no relevant financial relationships.
Shaina Hasan, MD, Amy Doran, MD, Rebecca Haug, MD. P4235 - Inability to Regulate Thyroid Hormones as a Unique Presentation of Autoimmune Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Autoimmune gastritis (AIG) is a relatively rare disease with limited treatment options, and it is often underdiagnosed. There is a strong association between autoimmune thyroid disease and AIG. We present a case of a patient with hypothyroidism who had gradually increasing levothyroxine requirements despite appropriate therapy, eventually found to have AIG.
Case Description/
Methods: A 58-year-old woman with hypothyroidism and pernicious anemia was initially evaluated for persistent iron deficiency anemia. Evaluation included EGD, colonoscopy, and VCE, which demonstrated erosive gastropathy, with gastric biopsy noting chronic gastritis and a reactive gastropathy pattern. Despite therapy, she remained dependent on IV iron infusions, folic acid supplementation, and B12 injections.
She follows with Endocrinology, who initially diagnosed her hypothyroidism twenty years prior and started on her on levothyroxine. She had persistently elevated TSH and low free T4 with only slight improvement in these levels after escalating to high doses of levothyroxine. A subsequent levothyroxine absorption test demonstrated reduced absorption.
Further workup noted persistent iron deficiency, folate deficiency, vitamin D deficiency, and low IgG levels. She tested positive for parietal cell antibody (PCA) and intrinsic factor antibody (IFA), suggestive of autoimmune gastritis. Evaluation of the small bowel with CT enterography was unremarkable, and follow up EGD demonstrated gastric ulcers and atrophy with erosive and reactive gastropathy on pathology. She remains on an oral proton pump inhibitor with referral to hematology for ongoing management of her iron deficiency and pernicious anemia.
Discussion: AIG remains underdiagnosed due to its asymptomatic nature, with more overt symptoms in later stages of disease. It is not until micronutrient and hematological deficiencies manifest that it is considered on the differential.
Our patient’s history of longstanding hypothyroidism with gradually increasing levothyroxine requirements despite appropriate adherence may have been her first manifestation of AIG, as it started several years prior to her initial presentation of persistent iron deficiency anemia. She received her diagnosis of AIG nearly four years later.
Patients with autoimmune thyroid disease and evidence of malabsorption with persistent anemia or vitamin B12 deficiency should be evaluated for AIG, which could help mitigate the diagnostic delay that often occurs in this patient population.
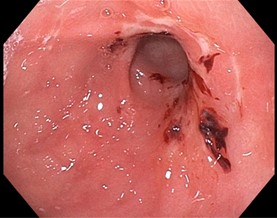
Figure: Gastric ulcers in the antrum
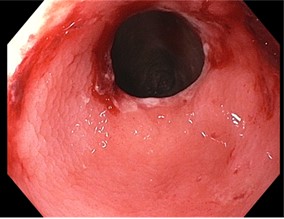
Figure: Gastric atrophy in the pre-pylorus with oozing on contact
Disclosures:
Shaina Hasan indicated no relevant financial relationships.
Amy Doran indicated no relevant financial relationships.
Rebecca Haug indicated no relevant financial relationships.
Shaina Hasan, MD, Amy Doran, MD, Rebecca Haug, MD. P4235 - Inability to Regulate Thyroid Hormones as a Unique Presentation of Autoimmune Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

