Monday Poster Session
Category: Stomach and Spleen
P4232 - Entangling Webs of Immunotherapy: A Case of Immune Checkpoint Inhibitor-Induced Gastritis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MC
Mark Cromer, MD
Prisma Health Greenville Memorial Hospital
Greenville, SC
Presenting Author(s)
Mark Cromer, MD, Jay Alden, DO, Weston Bettner, MD, Graziella Rangel Paniz, MD
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Immune checkpoint inhibitors (ICIs) enable immune cell proliferation to augment tumor destruction. Consequentially, inflammatory immune-related adverse events (irAEs) may develop; these are estimated to occur in 36% of palliative cases of advanced non-small cell lung cancer (NSCLC), with 9% reaching grade 3-5 severity. Gastrointestinal (GI) irAEs are the second most common type. We present a case of ICI-induced gastritis, an uncommon manifestation of GI-irAEs.
Case Description/
Methods: A 45-year-old male former smoker with poorly differentiated metastatic NSCLC, post-chemoradiation and pembrolizumab, presented with hematemesis without antecedent vomiting or melena. His last dose of immunotherapy was 3 months prior and caused grade 3 enterocolitis (nausea, vomiting, diarrhea, and right-sided colon inflammation on imaging); this resolved with immunotherapy cessation and a corticosteroid taper, completed 1 month prior. Otherwise, he reported intermittent NSAID use and no alcohol consumption.
Objectively, the patient was hemodynamically stable with a benign abdominal exam and labs reflecting normal hemoglobin, platelets, prothrombin time, lipase, and liver biochemical testing. No interval imaging was obtained. Upper endoscopy revealed diffuse severe gastric antral/body erythema, friability with spontaneous oozing blood, and mucosal sloughing with a spiderweb-like appearance. Hemostatic spray was attempted, but diffuse mucosal oozing persisted. Gastric biopsies revealed severe acute and chronic gastritis, focal intestinal metaplasia, negative Helicobacter pylori (HP) staining, and no dysplasia or malignancy – confirming the diagnosis of ICI-induced gastritis. Proton pump inhibitor and weight-based steroid therapy was started, the patient’s symptoms resolved, and he was discharged with close follow up.
Discussion: Gastritis accounts for only 5% of GI-irAEs, with colitis and hepatitis being the most common; 45-70% of gastritis cases have concomitant enterocolitis. Endoscopically, common mucosal findings are erythema (88%), friability (48%), and erosions (36%). The hallmark spiderweb-like appearance caused by mucosal sloughing (highlighted in our case) is a distinguishing feature that can expedite diagnosis and treatment. Prompt recognition of ICI-induced gastritis and early endoscopic assessment is essential to exclude other diagnoses (e.g. chemical gastritis, peptic ulcer disease, HP infection, malignancy, etc.), identify focal treatable lesions, and guide future anti-tumor therapeutic course.
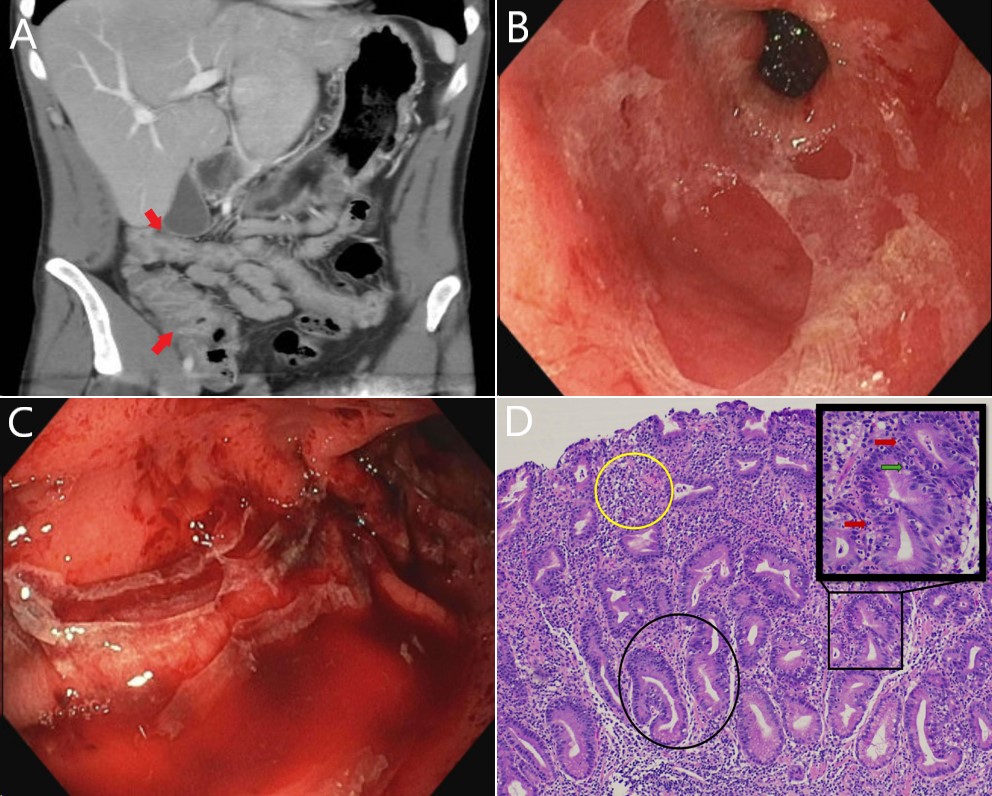
Figure: Figure 1: Case images
A) Coronal view of computed tomography scan during initial episode of immune-checkpoint inhibitor (ICI)-induced enterocolitis 3 months prior which showed diffuse colonic wall edema and peri-colonic stranding involving the right and transverse colon (red arrows) consistent with colitis.
B) and C) Endoscopy images during hospitalization showing diffuse gastric antral (B) and body (C) erythema, friability with spontaneous oozing, and mucosal sloughing with characteristic spiderweb-like appearance.
D) Histology slide showing both acute inflammation (lymphocytes, plasma cells, neutrophils, and eosinophils invading the lamina propria [yellow circle]; neutrophilic and lymphocytic crypt injury [red and green arrows, respectively]) and chronic inflammation (branched and irregularly shaped crypts [black circle]) consistent with ICI-induced gastritis.
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Jay Alden indicated no relevant financial relationships.
Weston Bettner indicated no relevant financial relationships.
Graziella Rangel Paniz indicated no relevant financial relationships.
Mark Cromer, MD, Jay Alden, DO, Weston Bettner, MD, Graziella Rangel Paniz, MD. P4232 - Entangling Webs of Immunotherapy: A Case of Immune Checkpoint Inhibitor-Induced Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Immune checkpoint inhibitors (ICIs) enable immune cell proliferation to augment tumor destruction. Consequentially, inflammatory immune-related adverse events (irAEs) may develop; these are estimated to occur in 36% of palliative cases of advanced non-small cell lung cancer (NSCLC), with 9% reaching grade 3-5 severity. Gastrointestinal (GI) irAEs are the second most common type. We present a case of ICI-induced gastritis, an uncommon manifestation of GI-irAEs.
Case Description/
Methods: A 45-year-old male former smoker with poorly differentiated metastatic NSCLC, post-chemoradiation and pembrolizumab, presented with hematemesis without antecedent vomiting or melena. His last dose of immunotherapy was 3 months prior and caused grade 3 enterocolitis (nausea, vomiting, diarrhea, and right-sided colon inflammation on imaging); this resolved with immunotherapy cessation and a corticosteroid taper, completed 1 month prior. Otherwise, he reported intermittent NSAID use and no alcohol consumption.
Objectively, the patient was hemodynamically stable with a benign abdominal exam and labs reflecting normal hemoglobin, platelets, prothrombin time, lipase, and liver biochemical testing. No interval imaging was obtained. Upper endoscopy revealed diffuse severe gastric antral/body erythema, friability with spontaneous oozing blood, and mucosal sloughing with a spiderweb-like appearance. Hemostatic spray was attempted, but diffuse mucosal oozing persisted. Gastric biopsies revealed severe acute and chronic gastritis, focal intestinal metaplasia, negative Helicobacter pylori (HP) staining, and no dysplasia or malignancy – confirming the diagnosis of ICI-induced gastritis. Proton pump inhibitor and weight-based steroid therapy was started, the patient’s symptoms resolved, and he was discharged with close follow up.
Discussion: Gastritis accounts for only 5% of GI-irAEs, with colitis and hepatitis being the most common; 45-70% of gastritis cases have concomitant enterocolitis. Endoscopically, common mucosal findings are erythema (88%), friability (48%), and erosions (36%). The hallmark spiderweb-like appearance caused by mucosal sloughing (highlighted in our case) is a distinguishing feature that can expedite diagnosis and treatment. Prompt recognition of ICI-induced gastritis and early endoscopic assessment is essential to exclude other diagnoses (e.g. chemical gastritis, peptic ulcer disease, HP infection, malignancy, etc.), identify focal treatable lesions, and guide future anti-tumor therapeutic course.
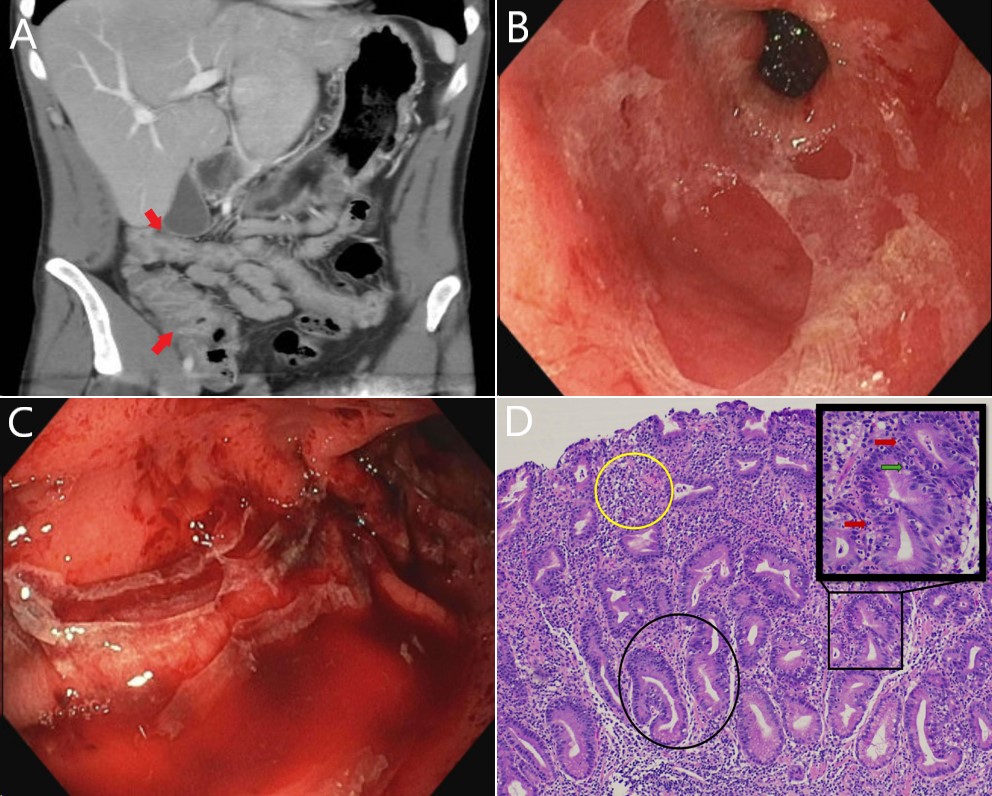
Figure: Figure 1: Case images
A) Coronal view of computed tomography scan during initial episode of immune-checkpoint inhibitor (ICI)-induced enterocolitis 3 months prior which showed diffuse colonic wall edema and peri-colonic stranding involving the right and transverse colon (red arrows) consistent with colitis.
B) and C) Endoscopy images during hospitalization showing diffuse gastric antral (B) and body (C) erythema, friability with spontaneous oozing, and mucosal sloughing with characteristic spiderweb-like appearance.
D) Histology slide showing both acute inflammation (lymphocytes, plasma cells, neutrophils, and eosinophils invading the lamina propria [yellow circle]; neutrophilic and lymphocytic crypt injury [red and green arrows, respectively]) and chronic inflammation (branched and irregularly shaped crypts [black circle]) consistent with ICI-induced gastritis.
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Jay Alden indicated no relevant financial relationships.
Weston Bettner indicated no relevant financial relationships.
Graziella Rangel Paniz indicated no relevant financial relationships.
Mark Cromer, MD, Jay Alden, DO, Weston Bettner, MD, Graziella Rangel Paniz, MD. P4232 - Entangling Webs of Immunotherapy: A Case of Immune Checkpoint Inhibitor-Induced Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

