Monday Poster Session
Category: Stomach and Spleen
P4226 - Gastro-Duodenal Strongyloidiasis as a Cause of Upper Gastrointestinal Bleeding in an Immunocompetent Patient With Poorly Controlled Diabetes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Jodie A. Barkin, MD, FACG
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Danielle Hahn, BA, Helen Bermudez, MD, Fabian Emura, MD, PhD, FACG, Domenika A. Ortiz Requena, MD, Jodie A. Barkin, MD, FACG
University of Miami Miller School of Medicine, Miami, FL
Introduction: Strongyloidiasis is a parasitic infection caused by the nematode Strongyloides stercoralis, rarely found in the United States. In immunocompetent individuals, infection can persist undetected for years. Clinical presentations vary from asymptomatic carriage to disseminated disease, often triggered by immunosuppression or physiological stressors. Severe gastrointestinal (GI) involvement is well-documented in immunocompromised hosts, but such presentations are rare in patients without obvious immunodeficiency. This case describes an immunocompetent man found to have severe GI manifestations of Strongyloidiasis.
Case Description/
Methods: A 47-year-old man with alcohol use disorder, poorly controlled type 2 diabetes mellitus (Hgb A1C 8.3%, point of care blood glucose 1169) presented with altered mental status, diabetic ketoacidosis (DKA) and bacteremia secondary to E.coli and E.faecalis. Complete blood count was consistent with neutrophilic left shift with absent eosinophilia. After treatment initiated for DKA and bacteremia, the GI service was consulted for evaluation of anemia with hematemesis and coffee-ground material from his nasogastric tube. GI bleeding and hemodilution from DKA management were considered contributory to his anemia. The patient reported months of postprandial vomiting and poor appetite prior to presentation. On upper endoscopy, LA Grade D esophagitis was noted, with numerous 5-10 mm ulcers in the stomach and duodenum without active bleeding but with old bleeding stigmata along with friable mucosa (Figure 1). Histopathology revealed ulcerated oxyntic mucosa with acute gastritis and numerous S. stercoralis larvae in the stomach and a diffuse inflammatory process with neutrophilic cryptitis and numerous larvae in the duodenum (Figure 2). Patient received a 2-week course of oral ivermectin, with no further bleeding. Immunodeficiency workup was negative.
Discussion: This case highlights a rarely reported GI manifestation of Strongyloidiasis in an immunocompetent individual. A literature review performed yielded overall few reported cases in immunocompetent patients, but uncontrolled diabetes was noted as a risk factor for Strongyloidiasis hyperinfection and symptomatic disease. Absence of eosinophilia is common in the hyperinfection phase of Strongyloidiasis. Strongyloidiasis should be ruled out in immunocompromised patients presenting with gastrointestinal bleeding and endoscopic findings of multiple gastric ulcers with friable mucosa.
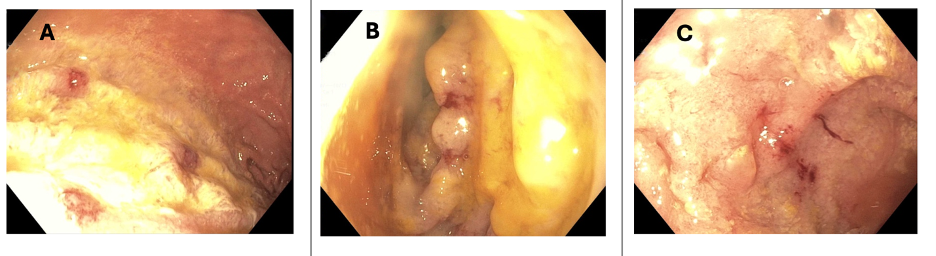
Figure: Figure 1: Endoscopic images (1A: Body of stomach, 1B: Duodenal Bulb, 1C: Second portion of duodenum) showing friable mucosa and diffuse ulceration secondary to Strongyloides stercoralis.
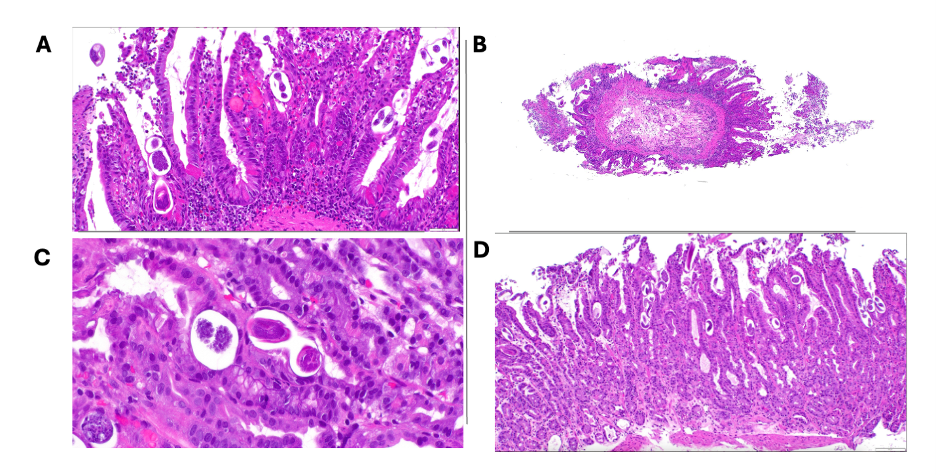
Figure: Figure 2: Histopathology slides demonstrating Strongyloides stercoralis
Figures 2A, 2B: Gastric mucosa containing numerous cross sections of Strongyloides larvae (Filariform larvae); Figures 2C, 2D: Duodenal mucosa with ulcer, reactive changes, and numerous Strongyloides larvae).
Disclosures:
Danielle Hahn indicated no relevant financial relationships.
Helen Bermudez indicated no relevant financial relationships.
Fabian Emura indicated no relevant financial relationships.
Domenika Ortiz Requena indicated no relevant financial relationships.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Danielle Hahn, BA, Helen Bermudez, MD, Fabian Emura, MD, PhD, FACG, Domenika A. Ortiz Requena, MD, Jodie A. Barkin, MD, FACG. P4226 - Gastro-Duodenal Strongyloidiasis as a Cause of Upper Gastrointestinal Bleeding in an Immunocompetent Patient With Poorly Controlled Diabetes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Miami Miller School of Medicine, Miami, FL
Introduction: Strongyloidiasis is a parasitic infection caused by the nematode Strongyloides stercoralis, rarely found in the United States. In immunocompetent individuals, infection can persist undetected for years. Clinical presentations vary from asymptomatic carriage to disseminated disease, often triggered by immunosuppression or physiological stressors. Severe gastrointestinal (GI) involvement is well-documented in immunocompromised hosts, but such presentations are rare in patients without obvious immunodeficiency. This case describes an immunocompetent man found to have severe GI manifestations of Strongyloidiasis.
Case Description/
Methods: A 47-year-old man with alcohol use disorder, poorly controlled type 2 diabetes mellitus (Hgb A1C 8.3%, point of care blood glucose 1169) presented with altered mental status, diabetic ketoacidosis (DKA) and bacteremia secondary to E.coli and E.faecalis. Complete blood count was consistent with neutrophilic left shift with absent eosinophilia. After treatment initiated for DKA and bacteremia, the GI service was consulted for evaluation of anemia with hematemesis and coffee-ground material from his nasogastric tube. GI bleeding and hemodilution from DKA management were considered contributory to his anemia. The patient reported months of postprandial vomiting and poor appetite prior to presentation. On upper endoscopy, LA Grade D esophagitis was noted, with numerous 5-10 mm ulcers in the stomach and duodenum without active bleeding but with old bleeding stigmata along with friable mucosa (Figure 1). Histopathology revealed ulcerated oxyntic mucosa with acute gastritis and numerous S. stercoralis larvae in the stomach and a diffuse inflammatory process with neutrophilic cryptitis and numerous larvae in the duodenum (Figure 2). Patient received a 2-week course of oral ivermectin, with no further bleeding. Immunodeficiency workup was negative.
Discussion: This case highlights a rarely reported GI manifestation of Strongyloidiasis in an immunocompetent individual. A literature review performed yielded overall few reported cases in immunocompetent patients, but uncontrolled diabetes was noted as a risk factor for Strongyloidiasis hyperinfection and symptomatic disease. Absence of eosinophilia is common in the hyperinfection phase of Strongyloidiasis. Strongyloidiasis should be ruled out in immunocompromised patients presenting with gastrointestinal bleeding and endoscopic findings of multiple gastric ulcers with friable mucosa.
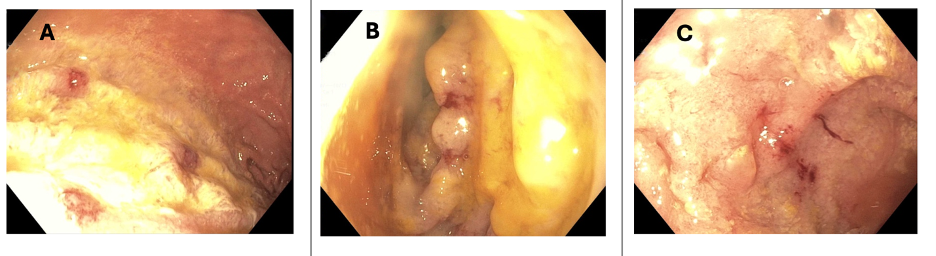
Figure: Figure 1: Endoscopic images (1A: Body of stomach, 1B: Duodenal Bulb, 1C: Second portion of duodenum) showing friable mucosa and diffuse ulceration secondary to Strongyloides stercoralis.
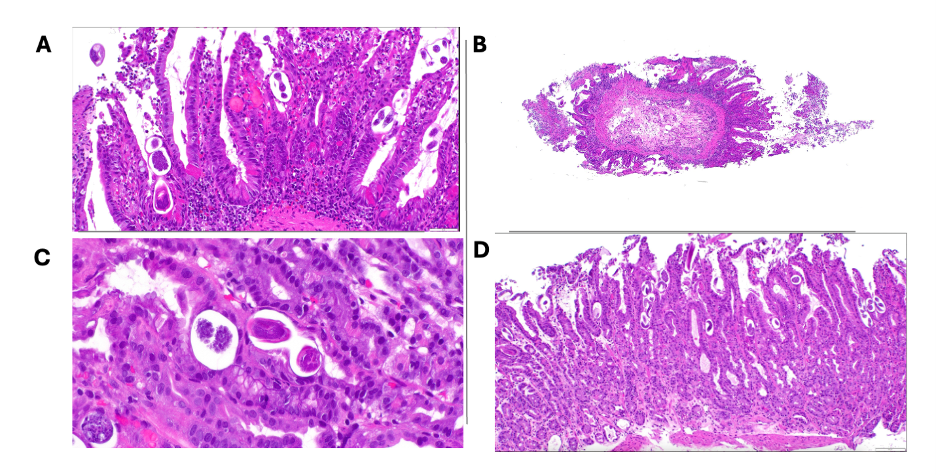
Figure: Figure 2: Histopathology slides demonstrating Strongyloides stercoralis
Figures 2A, 2B: Gastric mucosa containing numerous cross sections of Strongyloides larvae (Filariform larvae); Figures 2C, 2D: Duodenal mucosa with ulcer, reactive changes, and numerous Strongyloides larvae).
Disclosures:
Danielle Hahn indicated no relevant financial relationships.
Helen Bermudez indicated no relevant financial relationships.
Fabian Emura indicated no relevant financial relationships.
Domenika Ortiz Requena indicated no relevant financial relationships.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Danielle Hahn, BA, Helen Bermudez, MD, Fabian Emura, MD, PhD, FACG, Domenika A. Ortiz Requena, MD, Jodie A. Barkin, MD, FACG. P4226 - Gastro-Duodenal Strongyloidiasis as a Cause of Upper Gastrointestinal Bleeding in an Immunocompetent Patient With Poorly Controlled Diabetes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
