Monday Poster Session
Category: Stomach and Spleen
P4279 - Multifactorial Shock in Patient With Hiatal Hernia Causing Cardiac Compression
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GA
Graham Akeson, MS, MD
University Hospitals
Chardon, OH
Presenting Author(s)
Mohammed Mazumder, MD1, Graham Akeson, MS, MD2, Gregory Stefano, MD2, Charles Peng, MD2
1University Hospitals, Solon, OH; 2University Hospitals, Chardon, OH
Introduction: Cardiac tamponade secondary to a large hiatal hernia is a rare complication that is normally treated by surgical repair. We describe a case of a patient with a known stable paresophageal hernia presenting with hypotension. Diagnostic evaluation narrowed the differential to sepsis secondary to community acquired pneumonia (CAP), cardiomyopathy, pulmonary emboli (PE), or cardiac tamponade caused by compression from large paraesophageal hernia.
Case Description/
Methods: An 83 year old woman with a history of Parkinson’s, provoked deep vein thrombosis, remote history of breast cancer, and paraesophageal hernia, presented to the emergency department for weakness and diarrhea. Initial vital signs showed a heart rate of 91, blood pressure 96/48, and oxygen saturation of 50%. Computed tomography angiography of the chest showed multiple small PE with diffuse hazy densities concerning for CAP along with an intrathoracic stomach with organoaxial malrotation and gastric outlet obstruction. There was marked cardiac compression. It was not thought that the patient’s hemodynamic status was caused exclusively by the PE. She was started on vancomycin, cefepime, azithromycin, and a heparin infusion and admitted to the intensive care unit.
In the ICU, surgery recommended a nasogastric tube (NGT) for decompression. After five unsuccessful attempts to place the NGT, the patient refused further tries. Endoscopically guided decompression was also not immediately available. Emergent decompression was not recommended by surgery as the patient’s blood pressure modestly improved. It was believed that her hiatal hernia had decreased in size on its own as patient was still having bowel movements and passing gas. The patient was then started on metoclopromide 5mg three times daily. An echocardiogram showed normal left ventricular systolic function with the hernia compressing the left ventricle during systole. The patient was treated for pneumonia and PE, then eventually discharged on oral anticoagulation, oral antibiotics, and follow up with surgery.
Discussion: The justification to pursue aggressive therapy was outweighed by the risks inherent in such approaches. The presence of PE, therapeutic anticoagulation and hemodynamic instability meant that any surgical intervention would have been deemed high-risk for complications. Given the elevated procedural risk, conservative management with metoclopromide and dietary changes were utilized to address the underlying physiology without exposing the patient to excessive risk.
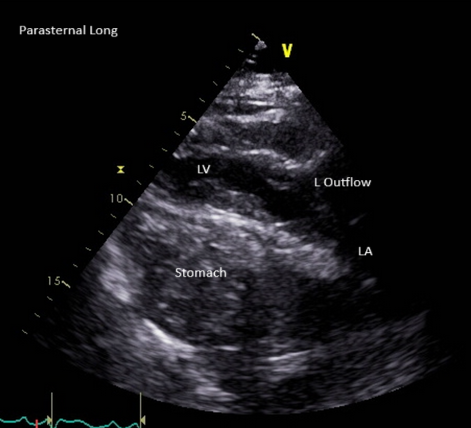
Figure: Transthoracic echocardiogram - parasternal long axis
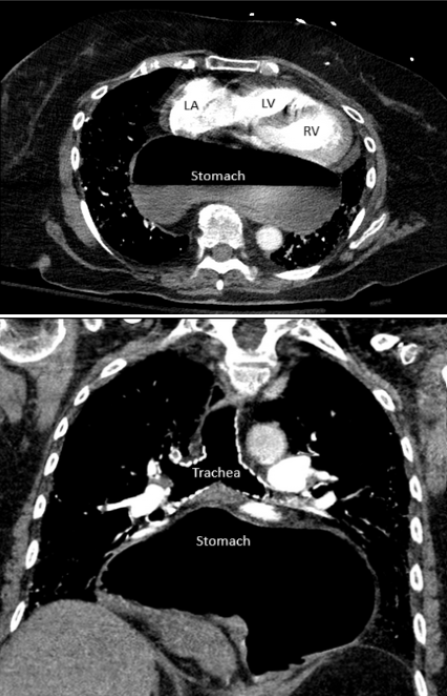
Figure: CT angiography chest
Disclosures:
Mohammed Mazumder indicated no relevant financial relationships.
Graham Akeson indicated no relevant financial relationships.
Gregory Stefano indicated no relevant financial relationships.
Charles Peng indicated no relevant financial relationships.
Mohammed Mazumder, MD1, Graham Akeson, MS, MD2, Gregory Stefano, MD2, Charles Peng, MD2. P4279 - Multifactorial Shock in Patient With Hiatal Hernia Causing Cardiac Compression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals, Solon, OH; 2University Hospitals, Chardon, OH
Introduction: Cardiac tamponade secondary to a large hiatal hernia is a rare complication that is normally treated by surgical repair. We describe a case of a patient with a known stable paresophageal hernia presenting with hypotension. Diagnostic evaluation narrowed the differential to sepsis secondary to community acquired pneumonia (CAP), cardiomyopathy, pulmonary emboli (PE), or cardiac tamponade caused by compression from large paraesophageal hernia.
Case Description/
Methods: An 83 year old woman with a history of Parkinson’s, provoked deep vein thrombosis, remote history of breast cancer, and paraesophageal hernia, presented to the emergency department for weakness and diarrhea. Initial vital signs showed a heart rate of 91, blood pressure 96/48, and oxygen saturation of 50%. Computed tomography angiography of the chest showed multiple small PE with diffuse hazy densities concerning for CAP along with an intrathoracic stomach with organoaxial malrotation and gastric outlet obstruction. There was marked cardiac compression. It was not thought that the patient’s hemodynamic status was caused exclusively by the PE. She was started on vancomycin, cefepime, azithromycin, and a heparin infusion and admitted to the intensive care unit.
In the ICU, surgery recommended a nasogastric tube (NGT) for decompression. After five unsuccessful attempts to place the NGT, the patient refused further tries. Endoscopically guided decompression was also not immediately available. Emergent decompression was not recommended by surgery as the patient’s blood pressure modestly improved. It was believed that her hiatal hernia had decreased in size on its own as patient was still having bowel movements and passing gas. The patient was then started on metoclopromide 5mg three times daily. An echocardiogram showed normal left ventricular systolic function with the hernia compressing the left ventricle during systole. The patient was treated for pneumonia and PE, then eventually discharged on oral anticoagulation, oral antibiotics, and follow up with surgery.
Discussion: The justification to pursue aggressive therapy was outweighed by the risks inherent in such approaches. The presence of PE, therapeutic anticoagulation and hemodynamic instability meant that any surgical intervention would have been deemed high-risk for complications. Given the elevated procedural risk, conservative management with metoclopromide and dietary changes were utilized to address the underlying physiology without exposing the patient to excessive risk.
Figure: Transthoracic echocardiogram - parasternal long axis
Figure: CT angiography chest
Disclosures:
Mohammed Mazumder indicated no relevant financial relationships.
Graham Akeson indicated no relevant financial relationships.
Gregory Stefano indicated no relevant financial relationships.
Charles Peng indicated no relevant financial relationships.
Mohammed Mazumder, MD1, Graham Akeson, MS, MD2, Gregory Stefano, MD2, Charles Peng, MD2. P4279 - Multifactorial Shock in Patient With Hiatal Hernia Causing Cardiac Compression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

