Monday Poster Session
Category: Stomach and Spleen
P4270 - Radioembolization Gone Rogue: 90Y Microspheres Causing Rapid Gastric Ulceration Requiring Gastrectomy and Gastrojejunostomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Amir Harb, DO1, Tareq Alsaleh, MD1, Raja Muhammad Hamza Mushtaq, MD2, Aimen Farooq, MD3, Mohammad Asfari, MD3
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Ayub Medical College, Abbottabad, Northern Areas, Pakistan; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Transcatheter arterial radioembolization (TARE) with β-emitting yttrium-90 (90Y) microspheres has utility in unresectable primary liver tumors or hepatic metastases. We present a case of a 62-year-old woman with hepatic metastases undergoing this procedure who developed a large gastric ulcer due to non-target radioembolization through aberrant arterial communication.
Case Description/
Methods: A 62-year-old woman presented to the emergency room with abdominal pain, nausea, and vomiting for the past two days. She has a history of small bowel carcinoid tumor with liver metastasis, for which she underwent TARE with 90Y glass microspheres via the left hepatic artery two days ago. Physical examination revealed generalized abdominal tenderness but was negative for peritoneal signs.
Single-photon emission computed tomography scan (SPECT) of the abdomen obtained during TARE showed radioactivity in the left hepatic lobe and dispersal of 90% of the microspheres to the antrum through a diminutive gastric artery branch coming off the left hepatic artery (Figure 1A). Initial supportive measures, including enteric nutrition, did not result in improvement. Upper endoscopy revealed a large gastric ulcer on the lesser curvature of the stomach (Figure 1B). Biopsies were negative for malignancy and common microorganisms. The patient ultimately underwent partial gastrectomy with gastrojejunostomy. Pathology evaluation showed ulcerations, inflammatory changes, but no evidence of malignancy (Figure 2). On outpatient follow-up, she reported resolution of symptoms.
Discussion: Patients undergoing TARE with 90Y microspheres are prone to developing ulceration. The incidence is low, ranging from 1.5-3.75%. It is believed to occur due to direct radiation damage from microspheres diverted from the intended therapeutic site through variant anatomy of the common hepatic artery, collateral circulation, or reflux of microspheres. The diminutive gastric artery branch was likely the cause in our case.
No guidelines regarding management of 90Y radiation-induced stomach ulceration currently exist. Supportive care and enteric nutrition have been successful in previous cases but not with our patient.
The unusual symptom onset on the same day of the TARE treatment portends to including ulceration earlier in the differential diagnosis in these contexts. Our case also underscores the importance of multidisciplinary care and the low threshold for endoscopy in patients who have undergone recent TARE.
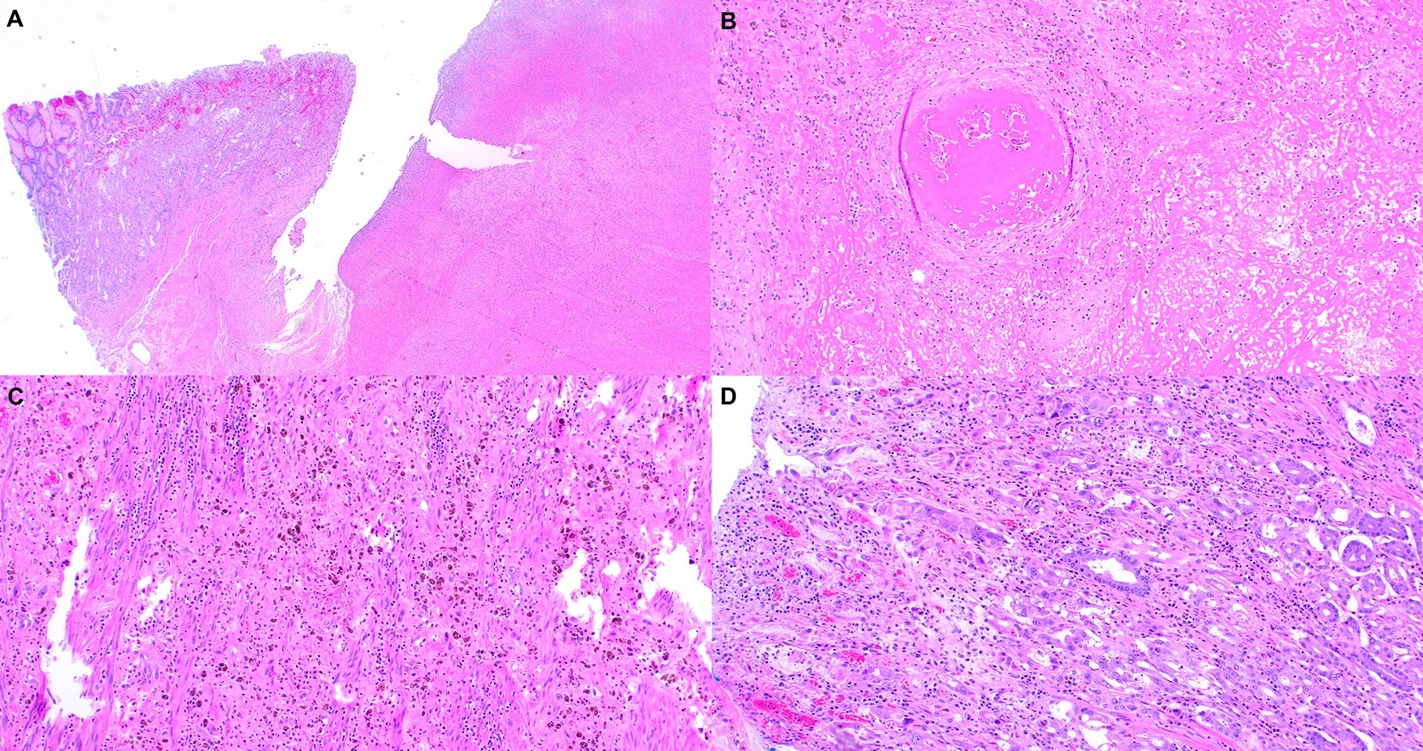
Figure: Figure 1A. SPECT imaging of the abdomen demonstrating radioactivity within the antrum of the stomach (white arrows) and little to no radioactivity in the left lobe of the liver. Figure 1B. Large, friable, necrotic gastric ulcer covering the distal lesser curvature from incisura to the pylorus. Hemostatic spray was applied due to oozing after contact and sampling.
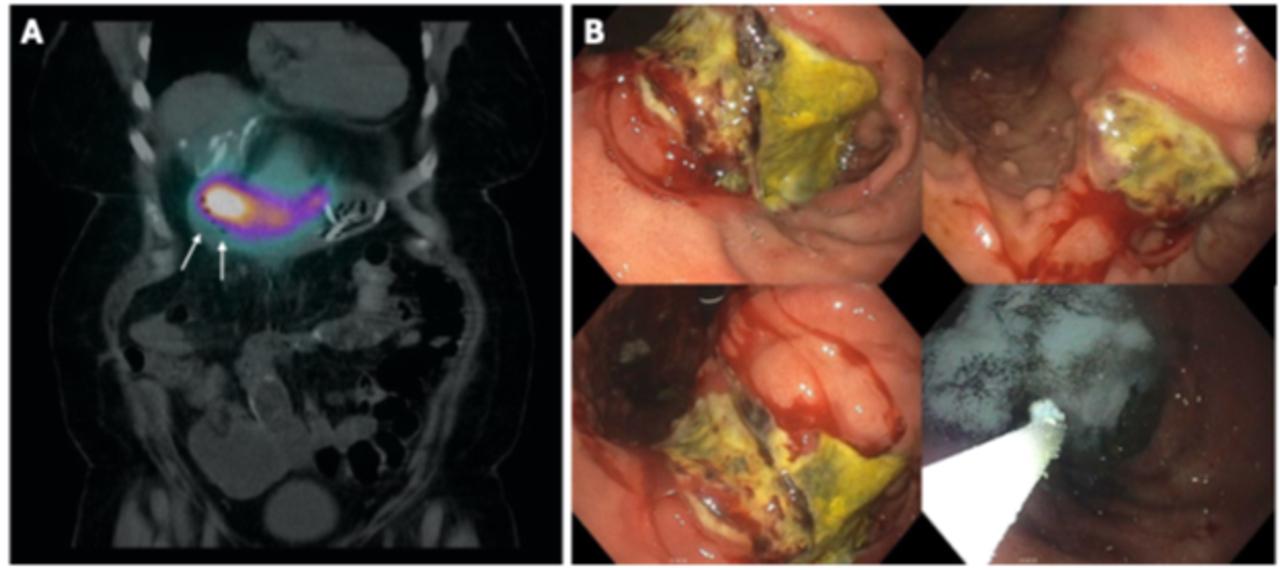
Figure: Figure 2A. Mucosal and transmural necrosis and ulceration. Figure 2B. Vascular thrombosis. Figure 2C. Reactive atypia, fibrinoid necrosis, and hemosiderin-laden histiocytes. Figure 2D. Reactive/radiation atypia.
Disclosures:
Amir Harb indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Raja Muhammad Hamza Mushtaq indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Amir Harb, DO1, Tareq Alsaleh, MD1, Raja Muhammad Hamza Mushtaq, MD2, Aimen Farooq, MD3, Mohammad Asfari, MD3. P4270 - Radioembolization Gone Rogue: 90Y Microspheres Causing Rapid Gastric Ulceration Requiring Gastrectomy and Gastrojejunostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Ayub Medical College, Abbottabad, Northern Areas, Pakistan; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Transcatheter arterial radioembolization (TARE) with β-emitting yttrium-90 (90Y) microspheres has utility in unresectable primary liver tumors or hepatic metastases. We present a case of a 62-year-old woman with hepatic metastases undergoing this procedure who developed a large gastric ulcer due to non-target radioembolization through aberrant arterial communication.
Case Description/
Methods: A 62-year-old woman presented to the emergency room with abdominal pain, nausea, and vomiting for the past two days. She has a history of small bowel carcinoid tumor with liver metastasis, for which she underwent TARE with 90Y glass microspheres via the left hepatic artery two days ago. Physical examination revealed generalized abdominal tenderness but was negative for peritoneal signs.
Single-photon emission computed tomography scan (SPECT) of the abdomen obtained during TARE showed radioactivity in the left hepatic lobe and dispersal of 90% of the microspheres to the antrum through a diminutive gastric artery branch coming off the left hepatic artery (Figure 1A). Initial supportive measures, including enteric nutrition, did not result in improvement. Upper endoscopy revealed a large gastric ulcer on the lesser curvature of the stomach (Figure 1B). Biopsies were negative for malignancy and common microorganisms. The patient ultimately underwent partial gastrectomy with gastrojejunostomy. Pathology evaluation showed ulcerations, inflammatory changes, but no evidence of malignancy (Figure 2). On outpatient follow-up, she reported resolution of symptoms.
Discussion: Patients undergoing TARE with 90Y microspheres are prone to developing ulceration. The incidence is low, ranging from 1.5-3.75%. It is believed to occur due to direct radiation damage from microspheres diverted from the intended therapeutic site through variant anatomy of the common hepatic artery, collateral circulation, or reflux of microspheres. The diminutive gastric artery branch was likely the cause in our case.
No guidelines regarding management of 90Y radiation-induced stomach ulceration currently exist. Supportive care and enteric nutrition have been successful in previous cases but not with our patient.
The unusual symptom onset on the same day of the TARE treatment portends to including ulceration earlier in the differential diagnosis in these contexts. Our case also underscores the importance of multidisciplinary care and the low threshold for endoscopy in patients who have undergone recent TARE.
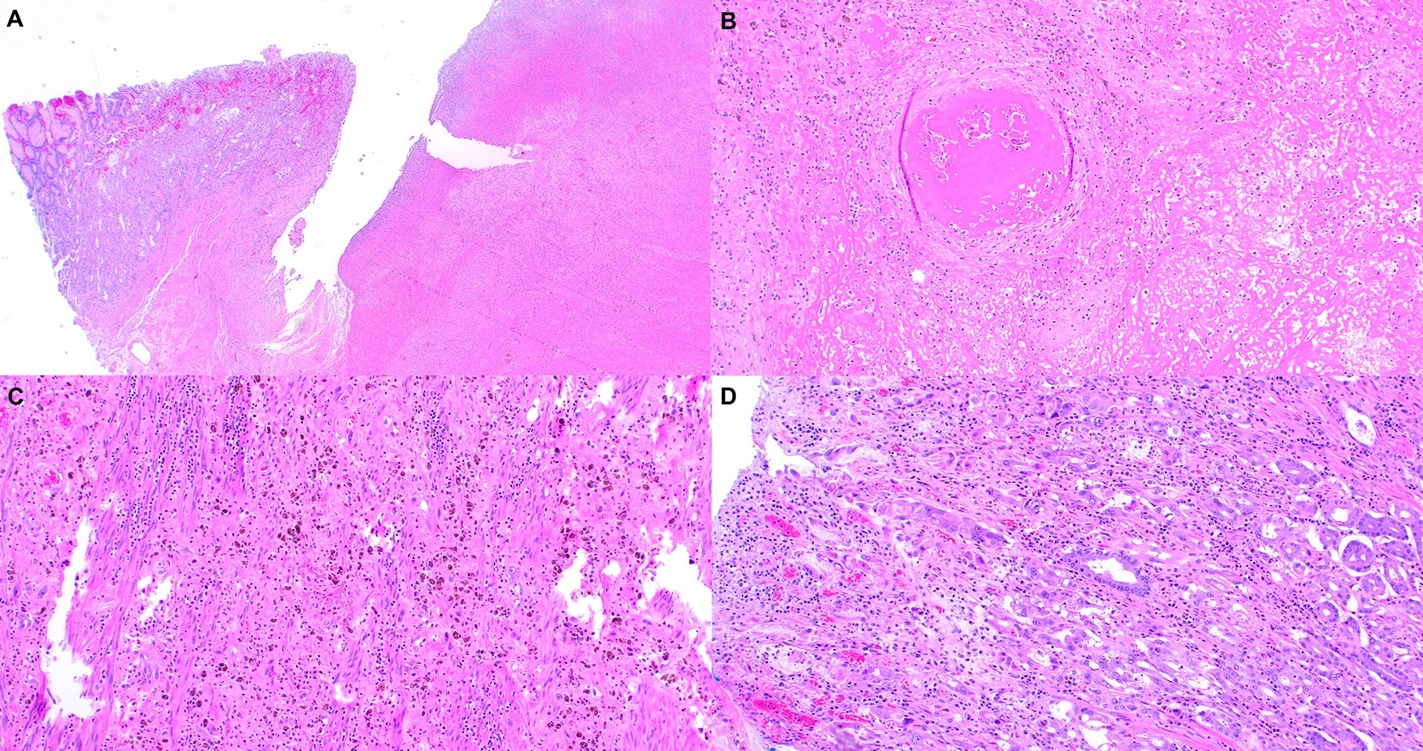
Figure: Figure 1A. SPECT imaging of the abdomen demonstrating radioactivity within the antrum of the stomach (white arrows) and little to no radioactivity in the left lobe of the liver. Figure 1B. Large, friable, necrotic gastric ulcer covering the distal lesser curvature from incisura to the pylorus. Hemostatic spray was applied due to oozing after contact and sampling.
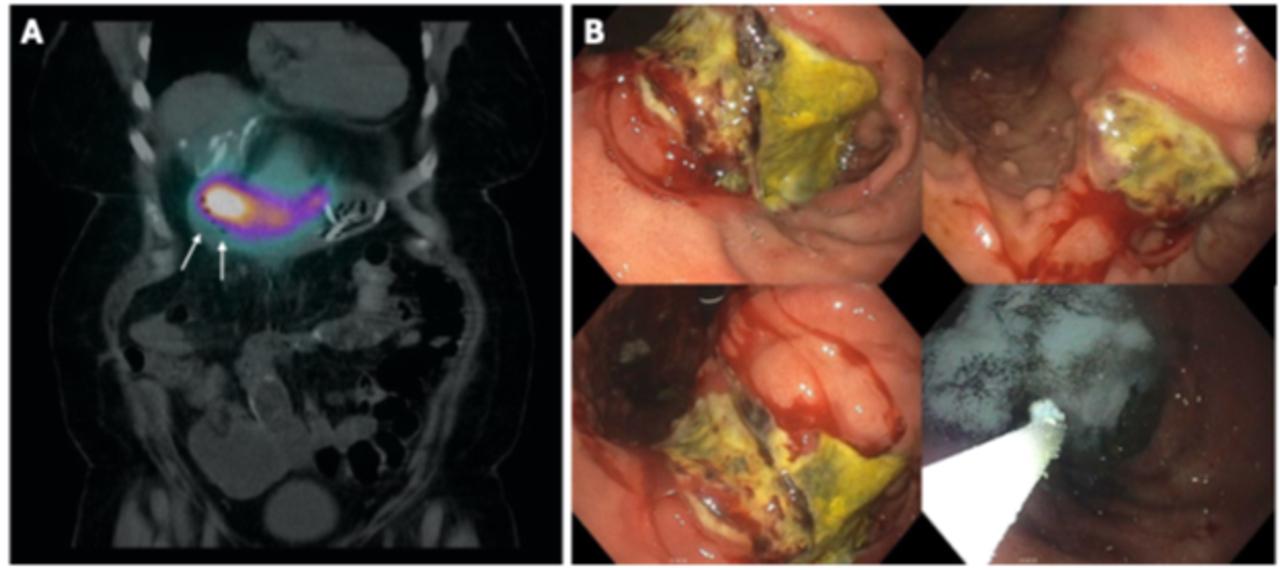
Figure: Figure 2A. Mucosal and transmural necrosis and ulceration. Figure 2B. Vascular thrombosis. Figure 2C. Reactive atypia, fibrinoid necrosis, and hemosiderin-laden histiocytes. Figure 2D. Reactive/radiation atypia.
Disclosures:
Amir Harb indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Raja Muhammad Hamza Mushtaq indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Amir Harb, DO1, Tareq Alsaleh, MD1, Raja Muhammad Hamza Mushtaq, MD2, Aimen Farooq, MD3, Mohammad Asfari, MD3. P4270 - Radioembolization Gone Rogue: 90Y Microspheres Causing Rapid Gastric Ulceration Requiring Gastrectomy and Gastrojejunostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
