Monday Poster Session
Category: Stomach and Spleen
P4255 - Synergistic Gastrointestinal Toxicity of Immune Checkpoint Inhibitors and Corticosteroids Leading to Gastric Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nathanial Bartosek, MD
Corewell Health East William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nathanial Bartosek, MD1, Melina Brown, DO2, Ahmed Aref, MBBCh3, Fady Banno, MD3, Naveen Reddy, MD4
1Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 2William Beaumont Hospital, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI; 4Corewell Health, Royal Oak, MI
Introduction: Immune checkpoint inhibitors (ICIs) are widely used in cancer treatment regimens but are associated with a variety of adverse events, including gastrointestinal (GI)+ complications. Although rare, GI bleeding and gastric perforation are serious complications linked to ICIs and prolonged corticosteroid use, which are often prescribed to mediate side effects of ICIs. Steroid treatment can impair mucosal defenses and delay healing, increasing risk of ulceration and perforation. This case highlights the relationship between ICIs and steroids, demonstrating the risk of severe upper GI complications and need for vigilant monitoring and early recognition in high-risk patients.
Case Description/
Methods: This is a 72-year-old female with a history of malignant mesothelioma and chronic lymphocytic leukemia who presented from a skilled nursing facility with altered mental status and hematemesis. Due to hemodynamic instability, she was intubated and started on vasopressors for hemorrhagic shock. CT abdomen/pelvis showed a left upper quadrant hematoma or mass. Her hemoglobin was 6.5 g/dL (normal: 12.1-15 g/dL), requiring blood transfusion. Emergent EGD revealed a large gastric perforation (figure 1), multiple gastric ulcers (Forrest IIB), duodenitis, and abnormal esophageal mucosa. Hemostasis was achieved endoscopically with clipping and argon plasma coagulation. Further history revealed she had been on 20 mg prednisone daily for 3 months due to immunotherapy-induced diarrhea from treatment for peritoneal mesothelioma. She was nonadherent to pantoprazole. Despite management, bleeding persisted, and the patient expired on day 7 with comfort measures.
Discussion: This case highlights the severe risk of gastrointestinal complications in patients on combined immunotherapy and prolonged corticosteroids. Immune checkpoint inhibitors can cause GI inflammation, which may be worsened by steroids impairing mucosal healing. In this patient, the rapid progression from a normal EGD three months prior to gastric ulceration and perforation exemplifies how quickly injury can occur. Nonadherence to proton pump inhibitors likely contributed to ulcer formation. Despite aggressive resuscitation and endoscopic therapy, the patient’s condition deteriorated, reflecting the high morbidity and mortality risk. This case emphasizes the importance of vigilant monitoring, adherence to gastroprotective measures, and early endoscopic evaluation in high-risk patients to prevent and manage GI complications.
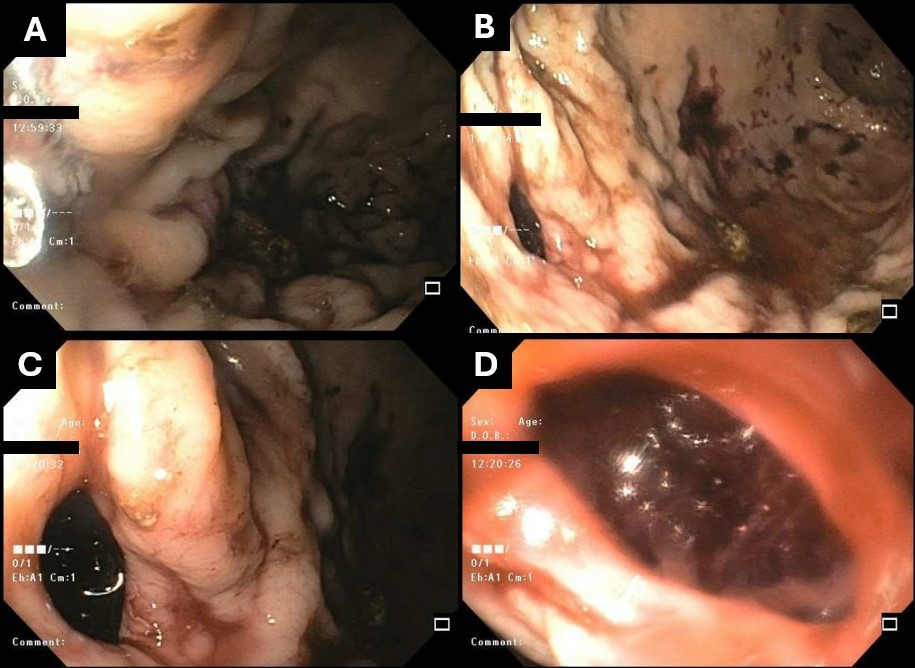
Figure: Figure 1: A,D) EGD images displaying extent of intragastric hemorrhage in the mid-gastric region; C,D) visualization of gastric perforation as an identified source of bleeding.
Disclosures:
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Ahmed Aref indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Naveen Reddy indicated no relevant financial relationships.
Nathanial Bartosek, MD1, Melina Brown, DO2, Ahmed Aref, MBBCh3, Fady Banno, MD3, Naveen Reddy, MD4. P4255 - Synergistic Gastrointestinal Toxicity of Immune Checkpoint Inhibitors and Corticosteroids Leading to Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 2William Beaumont Hospital, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI; 4Corewell Health, Royal Oak, MI
Introduction: Immune checkpoint inhibitors (ICIs) are widely used in cancer treatment regimens but are associated with a variety of adverse events, including gastrointestinal (GI)+ complications. Although rare, GI bleeding and gastric perforation are serious complications linked to ICIs and prolonged corticosteroid use, which are often prescribed to mediate side effects of ICIs. Steroid treatment can impair mucosal defenses and delay healing, increasing risk of ulceration and perforation. This case highlights the relationship between ICIs and steroids, demonstrating the risk of severe upper GI complications and need for vigilant monitoring and early recognition in high-risk patients.
Case Description/
Methods: This is a 72-year-old female with a history of malignant mesothelioma and chronic lymphocytic leukemia who presented from a skilled nursing facility with altered mental status and hematemesis. Due to hemodynamic instability, she was intubated and started on vasopressors for hemorrhagic shock. CT abdomen/pelvis showed a left upper quadrant hematoma or mass. Her hemoglobin was 6.5 g/dL (normal: 12.1-15 g/dL), requiring blood transfusion. Emergent EGD revealed a large gastric perforation (figure 1), multiple gastric ulcers (Forrest IIB), duodenitis, and abnormal esophageal mucosa. Hemostasis was achieved endoscopically with clipping and argon plasma coagulation. Further history revealed she had been on 20 mg prednisone daily for 3 months due to immunotherapy-induced diarrhea from treatment for peritoneal mesothelioma. She was nonadherent to pantoprazole. Despite management, bleeding persisted, and the patient expired on day 7 with comfort measures.
Discussion: This case highlights the severe risk of gastrointestinal complications in patients on combined immunotherapy and prolonged corticosteroids. Immune checkpoint inhibitors can cause GI inflammation, which may be worsened by steroids impairing mucosal healing. In this patient, the rapid progression from a normal EGD three months prior to gastric ulceration and perforation exemplifies how quickly injury can occur. Nonadherence to proton pump inhibitors likely contributed to ulcer formation. Despite aggressive resuscitation and endoscopic therapy, the patient’s condition deteriorated, reflecting the high morbidity and mortality risk. This case emphasizes the importance of vigilant monitoring, adherence to gastroprotective measures, and early endoscopic evaluation in high-risk patients to prevent and manage GI complications.
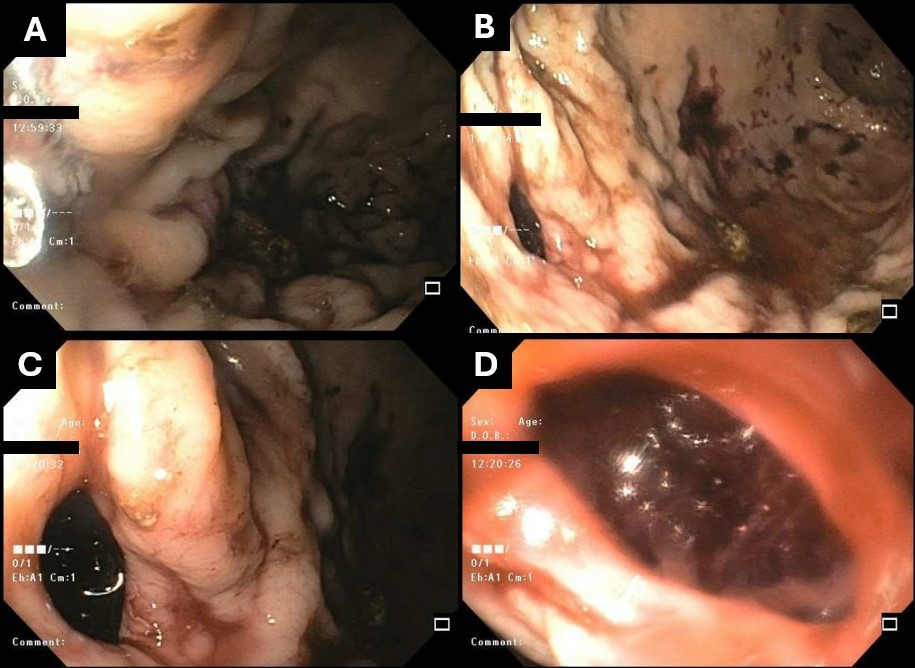
Figure: Figure 1: A,D) EGD images displaying extent of intragastric hemorrhage in the mid-gastric region; C,D) visualization of gastric perforation as an identified source of bleeding.
Disclosures:
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Ahmed Aref indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Naveen Reddy indicated no relevant financial relationships.
Nathanial Bartosek, MD1, Melina Brown, DO2, Ahmed Aref, MBBCh3, Fady Banno, MD3, Naveen Reddy, MD4. P4255 - Synergistic Gastrointestinal Toxicity of Immune Checkpoint Inhibitors and Corticosteroids Leading to Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

