Monday Poster Session
Category: Stomach and Spleen
P4254 - Gastric Perforation Secondary to Ingested Fishbone: A Case of Delayed Presentation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nathanial Bartosek, MD
Corewell Health East William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nathanial Bartosek, MD1, Melina Brown, DO2, Fady Banno, MD3, Andrew Aneese, MD2
1Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 2William Beaumont Hospital, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Foreign body ingestion causing gastric perforation is uncommon, fishbones present unique challenges due to their radiolucent nature and ability to migrate. We present a chronic gastric perforation from an ingested fishbone resulting in hepatic adhesions and abscess formation, requiring surgical intervention after failed endoscopic management.
Case Description/
Methods: A 69-year-old female with a history of a pulmonary embolism on apixaban presented with three months of intermittent abdominal pain, acutely worsening over several weeks. She reported fevers and chills but denied dysphagia or dietary changes. Examination revealed focal epigastric tenderness. Laboratory values were unremarkable. Non-contrast CT revealed a linear radiopaque density >2.5cm extending from the gastric wall into adjacent fat (Figure 1), abutting the left hepatic lobe, concerning for foreign body perforation.
Endoscopic investigation on hospital day 2 identified a raised area with purulent drainage (Figure 2a) along the lesser curvature of the stomach. Despite probing, the foreign body could not be visualized. Endoscopic clip placement was performed for localization and attempted closure (Figure 2b).
Following unsuccessful endoscopic retrieval, robotic surgery was performed on hospital day 4. Dense adhesions were encountered between the left hepatic lobe and lesser gastric curvature. Dissection revealed a phlegmonous, walled-off cavity containing a 2.7cm fishbone. Primary repair with omental patch was performed after right gastric artery ligation. The patient was discharged on hospital day 6 without antibiotics. Anticoagulation was resumed without complications.
Discussion: This case illustrates unique features of fishbone perforation. The delayed presentation with chronic walled-off perforation and hepatic adhesion formation is unusual, as most present acutely. The patient's inability to recall fishbone ingestion highlights often-asymptomatic passage through the upper gastrointestinal tract.
Endoscopic management proved inadequate due to extraluminal migration and inflammatory changes obscuring visualization. The development of hepatic adhesions and abscess formation necessitated surgical intervention, demonstrating the importance of multidisciplinary management.
This case emphasizes the need for high clinical suspicion when linear densities are identified on imaging, even without clear ingestion history, and highlights potential chronic complications requiring surgical management when endoscopic retrieval fails
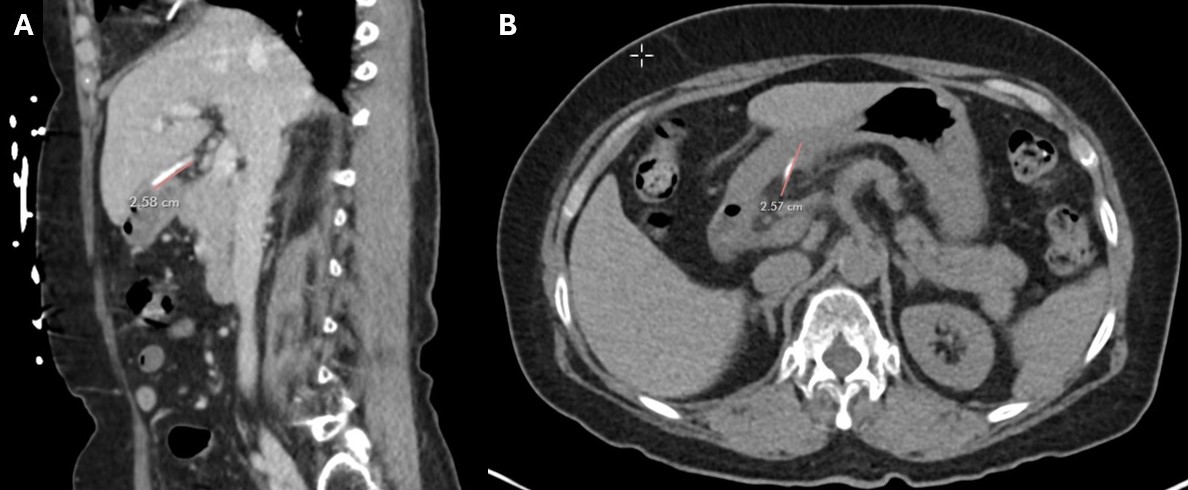
Figure: Figure 1: CT imaging revealing a roughly 2.6cm linear hyperdensity adjacent to the lesser curvature of the stomach in sagittal (A) and transverse (B) view, later revealed to be a fishbone.
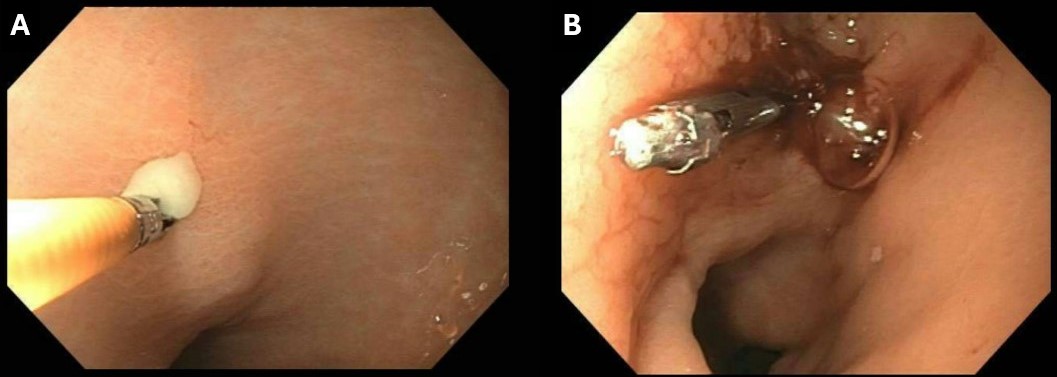
Figure: Figure 2: Raised area with purulent drainage along the lesser curvature between the incisura and pylorus with purulent drainage (A), marked with clip for identification and closure (B).
Disclosures:
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Andrew Aneese indicated no relevant financial relationships.
Nathanial Bartosek, MD1, Melina Brown, DO2, Fady Banno, MD3, Andrew Aneese, MD2. P4254 - Gastric Perforation Secondary to Ingested Fishbone: A Case of Delayed Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 2William Beaumont Hospital, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Foreign body ingestion causing gastric perforation is uncommon, fishbones present unique challenges due to their radiolucent nature and ability to migrate. We present a chronic gastric perforation from an ingested fishbone resulting in hepatic adhesions and abscess formation, requiring surgical intervention after failed endoscopic management.
Case Description/
Methods: A 69-year-old female with a history of a pulmonary embolism on apixaban presented with three months of intermittent abdominal pain, acutely worsening over several weeks. She reported fevers and chills but denied dysphagia or dietary changes. Examination revealed focal epigastric tenderness. Laboratory values were unremarkable. Non-contrast CT revealed a linear radiopaque density >2.5cm extending from the gastric wall into adjacent fat (Figure 1), abutting the left hepatic lobe, concerning for foreign body perforation.
Endoscopic investigation on hospital day 2 identified a raised area with purulent drainage (Figure 2a) along the lesser curvature of the stomach. Despite probing, the foreign body could not be visualized. Endoscopic clip placement was performed for localization and attempted closure (Figure 2b).
Following unsuccessful endoscopic retrieval, robotic surgery was performed on hospital day 4. Dense adhesions were encountered between the left hepatic lobe and lesser gastric curvature. Dissection revealed a phlegmonous, walled-off cavity containing a 2.7cm fishbone. Primary repair with omental patch was performed after right gastric artery ligation. The patient was discharged on hospital day 6 without antibiotics. Anticoagulation was resumed without complications.
Discussion: This case illustrates unique features of fishbone perforation. The delayed presentation with chronic walled-off perforation and hepatic adhesion formation is unusual, as most present acutely. The patient's inability to recall fishbone ingestion highlights often-asymptomatic passage through the upper gastrointestinal tract.
Endoscopic management proved inadequate due to extraluminal migration and inflammatory changes obscuring visualization. The development of hepatic adhesions and abscess formation necessitated surgical intervention, demonstrating the importance of multidisciplinary management.
This case emphasizes the need for high clinical suspicion when linear densities are identified on imaging, even without clear ingestion history, and highlights potential chronic complications requiring surgical management when endoscopic retrieval fails
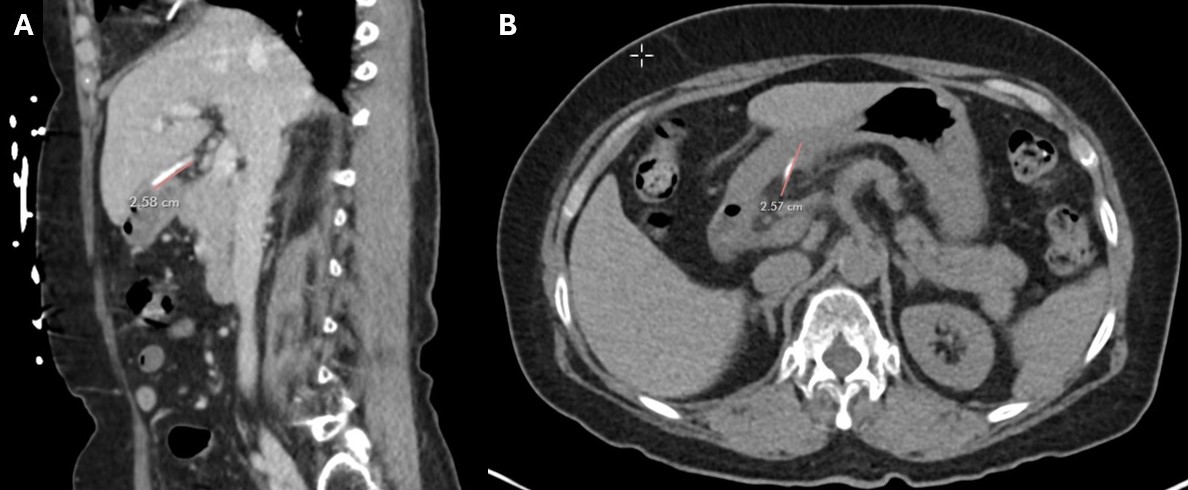
Figure: Figure 1: CT imaging revealing a roughly 2.6cm linear hyperdensity adjacent to the lesser curvature of the stomach in sagittal (A) and transverse (B) view, later revealed to be a fishbone.
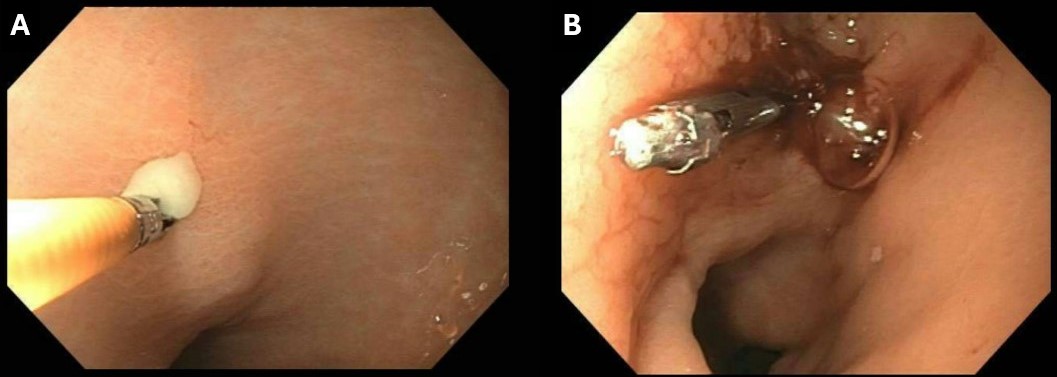
Figure: Figure 2: Raised area with purulent drainage along the lesser curvature between the incisura and pylorus with purulent drainage (A), marked with clip for identification and closure (B).
Disclosures:
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Andrew Aneese indicated no relevant financial relationships.
Nathanial Bartosek, MD1, Melina Brown, DO2, Fady Banno, MD3, Andrew Aneese, MD2. P4254 - Gastric Perforation Secondary to Ingested Fishbone: A Case of Delayed Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
