Monday Poster Session
Category: Stomach and Spleen
P4239 - Delayed Splenic Abscess Following Splenic Artery Aneurysm Embolization in a Patient With Decompensated Cirrhosis: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nisar Amin, MD
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Nisar Amin, MD, Roberta J.. Hunter, MD, Harleen Chela, MD, Ebubekir Daglilar, MD
Charleston Area Medical Center, Charleston, WV
Introduction: Splenic artery aneurysm is a known complication of cirrhosis. Various endoluminal techniques are employed for aneurysm exclusion, with the choice guided by anatomical and patient-specific factors. Embolization is a commonly used approach with a generally favorable safety profile. We present a rare case of splenic abscess 2 months following splenic artery embolization.
Case Description/
Methods: A 64-year-old male with a complex medical history including cirrhosis secondary to HCV (eradicated in 2016), esophageal and gastric varices, status-post CARTO, hepatocellular carcinoma status post TACE and recent Y-90 radioembolization, and a splenic artery aneurysm >3cm status post embolization two months prior, presented to the emergency department with worsening abdominal distention, left upper quadrant abdominal pain, and shortness of breath over three days. On presentation, the patient was tachypneic (RR 40s), tachycardic (HR 150s), and hypotensive, requiring vasopressors and BiPAP support. Physical examination revealed a distended, diffusely tender abdomen with maximal tenderness in the LUQ. Laboratory results showed leukocytosis (WBC 10.8) with 46% bandemia, INR 1.35, lactate 10.4 mmol/L, and mild renal and hepatic dysfunction. A CT scan of the abdomen and pelvis demonstrated moderate ascites, cirrhotic liver with two hypodense lesions, and a large splenic fluid collection near the previously embolized hilum (Figure1). Diagnostic paracentesis revealed neutrophilic ascites without malignant cells. Ultrasound-guided drainage of the splenic cyst yielded 1L of purulent fluid, and a catheter was placed for continuous drainage; cultures were negative. The patient completed a two-week course of piperacillin-tazobactam. His hospital course was complicated by COVID-19 requiring ICU care. Follow-up imaging showed resolution of the collection, and the catheter was removed two months later. He was discharged home in stable condition.
Discussion: Splenic abscess is a rare but serious complication of splenic artery embolization, often due to ischemia from reduced splenic perfusion. The risk is higher in patients with poor collateral circulation and is influenced by both patient factors and embolization technique. Hayes et al. found a higher rate of perisplenic abscess with gelfoam compared to coil embolization. While most abscesses occur within six months, delayed presentations are possible. Management usually involves percutaneous drainage and antibiotics, though splenectomy may be necessary in resistant cases.
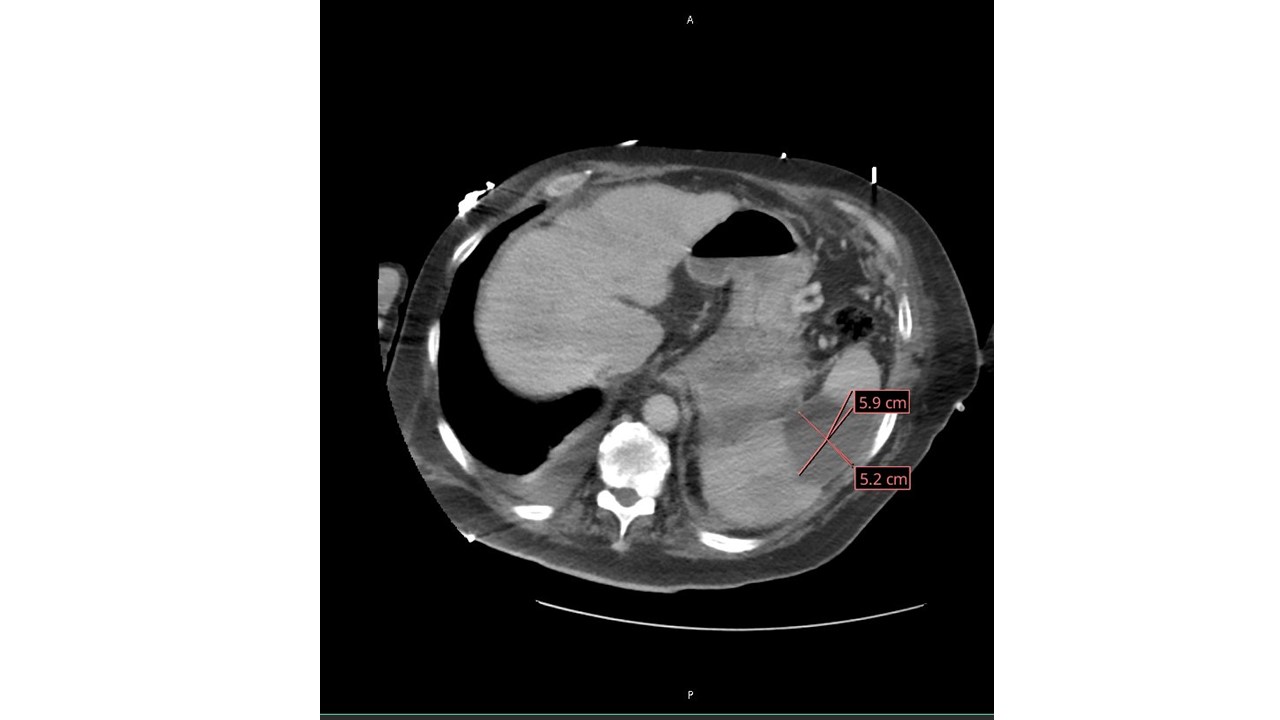
Figure: Splenomegaly with large 5.9 cm x 5.2 cm cystic lesion of the spleen.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Roberta Hunter indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD, Roberta J.. Hunter, MD, Harleen Chela, MD, Ebubekir Daglilar, MD. P4239 - Delayed Splenic Abscess Following Splenic Artery Aneurysm Embolization in a Patient With Decompensated Cirrhosis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Charleston Area Medical Center, Charleston, WV
Introduction: Splenic artery aneurysm is a known complication of cirrhosis. Various endoluminal techniques are employed for aneurysm exclusion, with the choice guided by anatomical and patient-specific factors. Embolization is a commonly used approach with a generally favorable safety profile. We present a rare case of splenic abscess 2 months following splenic artery embolization.
Case Description/
Methods: A 64-year-old male with a complex medical history including cirrhosis secondary to HCV (eradicated in 2016), esophageal and gastric varices, status-post CARTO, hepatocellular carcinoma status post TACE and recent Y-90 radioembolization, and a splenic artery aneurysm >3cm status post embolization two months prior, presented to the emergency department with worsening abdominal distention, left upper quadrant abdominal pain, and shortness of breath over three days. On presentation, the patient was tachypneic (RR 40s), tachycardic (HR 150s), and hypotensive, requiring vasopressors and BiPAP support. Physical examination revealed a distended, diffusely tender abdomen with maximal tenderness in the LUQ. Laboratory results showed leukocytosis (WBC 10.8) with 46% bandemia, INR 1.35, lactate 10.4 mmol/L, and mild renal and hepatic dysfunction. A CT scan of the abdomen and pelvis demonstrated moderate ascites, cirrhotic liver with two hypodense lesions, and a large splenic fluid collection near the previously embolized hilum (Figure1). Diagnostic paracentesis revealed neutrophilic ascites without malignant cells. Ultrasound-guided drainage of the splenic cyst yielded 1L of purulent fluid, and a catheter was placed for continuous drainage; cultures were negative. The patient completed a two-week course of piperacillin-tazobactam. His hospital course was complicated by COVID-19 requiring ICU care. Follow-up imaging showed resolution of the collection, and the catheter was removed two months later. He was discharged home in stable condition.
Discussion: Splenic abscess is a rare but serious complication of splenic artery embolization, often due to ischemia from reduced splenic perfusion. The risk is higher in patients with poor collateral circulation and is influenced by both patient factors and embolization technique. Hayes et al. found a higher rate of perisplenic abscess with gelfoam compared to coil embolization. While most abscesses occur within six months, delayed presentations are possible. Management usually involves percutaneous drainage and antibiotics, though splenectomy may be necessary in resistant cases.
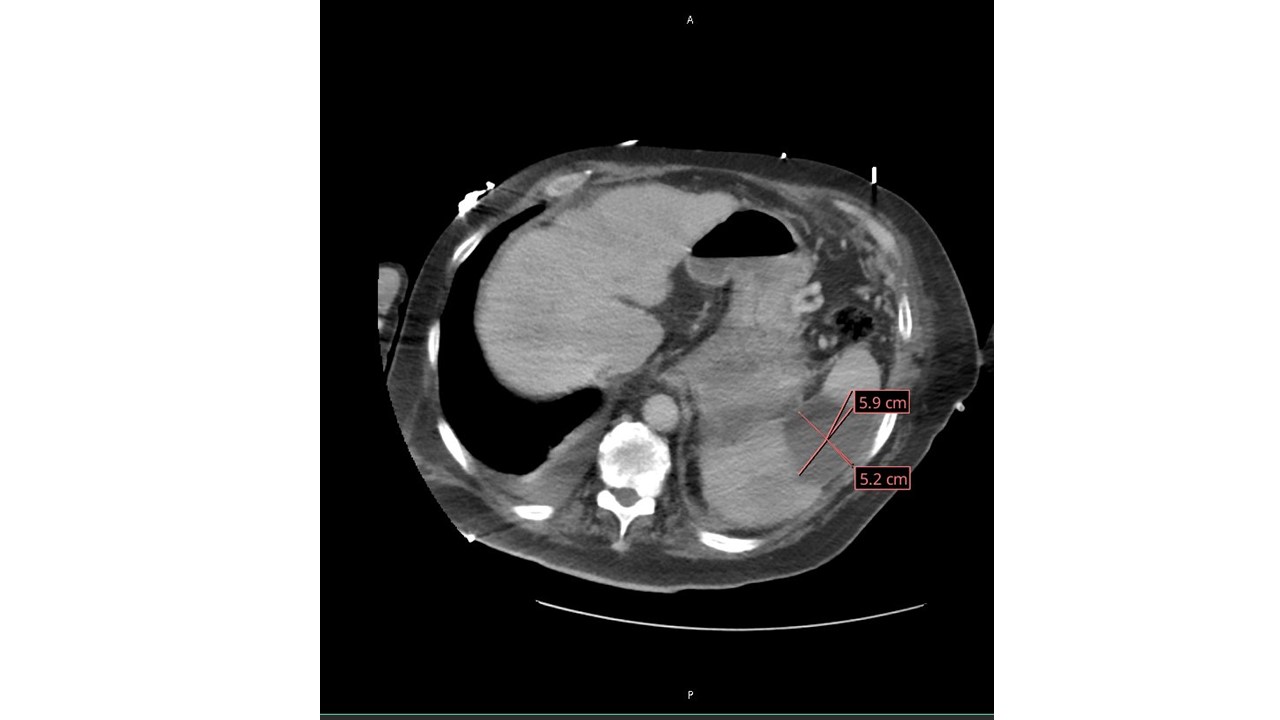
Figure: Splenomegaly with large 5.9 cm x 5.2 cm cystic lesion of the spleen.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Roberta Hunter indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD, Roberta J.. Hunter, MD, Harleen Chela, MD, Ebubekir Daglilar, MD. P4239 - Delayed Splenic Abscess Following Splenic Artery Aneurysm Embolization in a Patient With Decompensated Cirrhosis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
