Monday Poster Session
Category: Stomach and Spleen
P4217 - Clinical Dilemma in Eosinophilic Gastritis: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark Anthony Fallorina, MD (he/him/his)
NYC Health + Hospitals/South Brooklyn Health
Brooklyn, NY
Presenting Author(s)
Mark Anthony Fallorina, MD1, Jarin Prasa, DO2, Yasar Ahtsham, MD3, Joshua Diaz, MD3, Michael Bernstein, MD1
1NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 2NYC Health + Hospitals/South Brooklyn Health, New York, NY; 3South brooklyn Health, Brooklyn, NY
Introduction: Eosinophilic Gastrointestinal Disease (EGID) is a condition characterized by an abnormal presence of eosinophils in the gastrointestinal tract, without identifiable secondary causes, affecting approximately 6.3 out of 100,000 people in the U.S., mostly women with atopic conditions. Diagnosis typically occurs when biopsies show 20 or more eosinophils per high-power field (HPF) alongside gastrointestinal symptoms. The 2022 consensus introduced a classification system: eosinophilic gastritis (EoG) affects the stomach, eosinophilic enteritis (EoN) targets the small intestine, and eosinophilic colitis (EoC) impacts the colon. The mechanisms are still being studied, but immune responses to allergens are believed to play a significant role.
Case Description/
Methods: A 69-year-old female with a history of asthma with recent exacerbations on oral steroids, type 2 diabetes mellitus, and hypothyroidism presented with three weeks of nausea, vomiting, diarrhea, and poor oral intake. Imaging studies revealed a large hiatal hernia, while other diagnostic evaluations were negative. An initial esophagogastroduodenoscopy (EGD) with stomach biopsy showed eosinophilia, revealing 60-90 eosinophils per high power field (HPF) infiltrating the lamina propria and muscularis mucosa (Figure A). Following the initiation of high-dose steroid treatment, the patient exhibited marked clinical improvement. Follow up EGD confirmed the resolution of eosinophilic infiltration (Figure B), and was subsequently discharged with a steroid taper.
Discussion: The patient’s case raises questions about the interplay between the hiatal hernia and eosinophilic gastritis, in light of her history of oral steroid use due to recent asthma exacerbations and ongoing symptoms. Hiatal hernia may weaken the lower esophageal sphincter, which can lead to reflux of stomach acid and contents into the esophagus and, potentially, the stomach. Prolonged exposure to stomach acid could irritate the stomach lining and exacerbate the inflammatory response characteristic of eosinophilic gastritis (EoG). This cumulative pathological burden could potentially lead to complications related to EoG. Furthermore, the absence of established treatment guidelines for eosinophilic gastritis—where systemic corticosteroids are typically the standard treatment—highlights the urgent need for additional research to identify optimal therapeutic options for managing this condition.
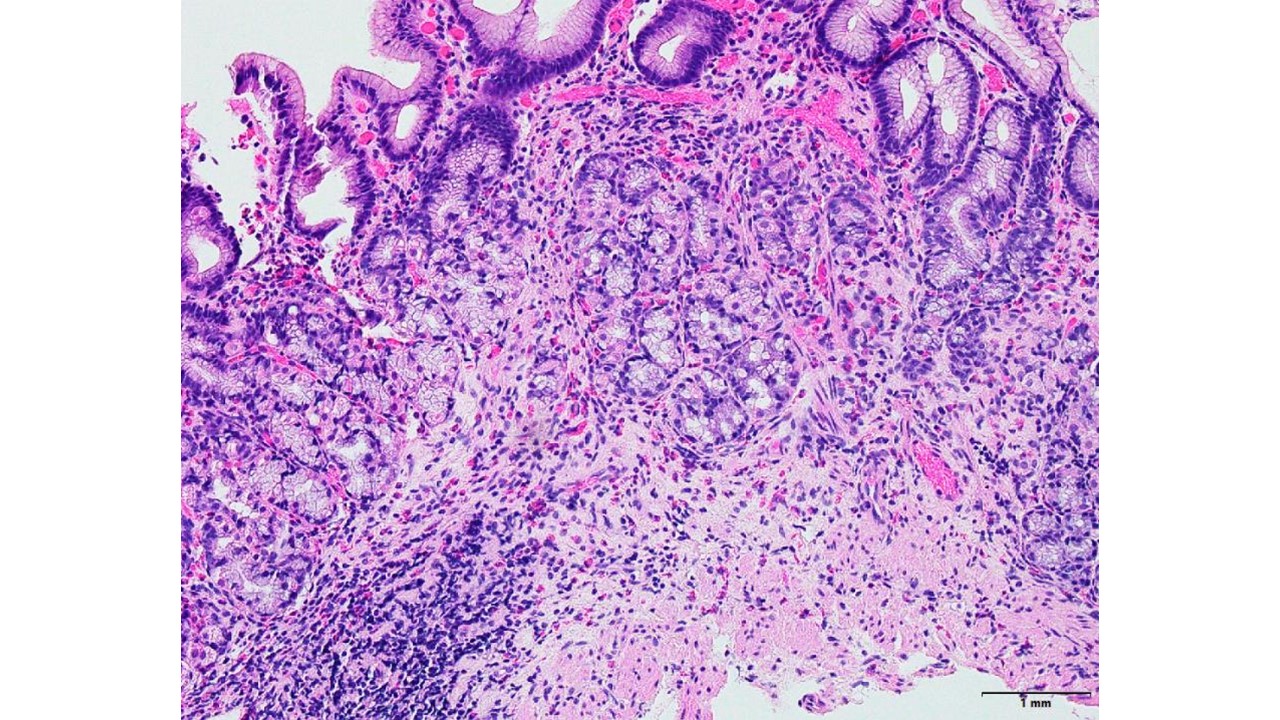
Figure: Figure A. Initial EGD with biopsy: Stomach body and antrum showed eosinophilic-rich gastritis. Small fragments of gastric oxyntic and antral type gastric mucosa with lamina propria edema and increased eosinophils ( 50-60 eosinophils per hpf). These eosinophils are primarily located within the lamina propria and the muscularis mucosa.
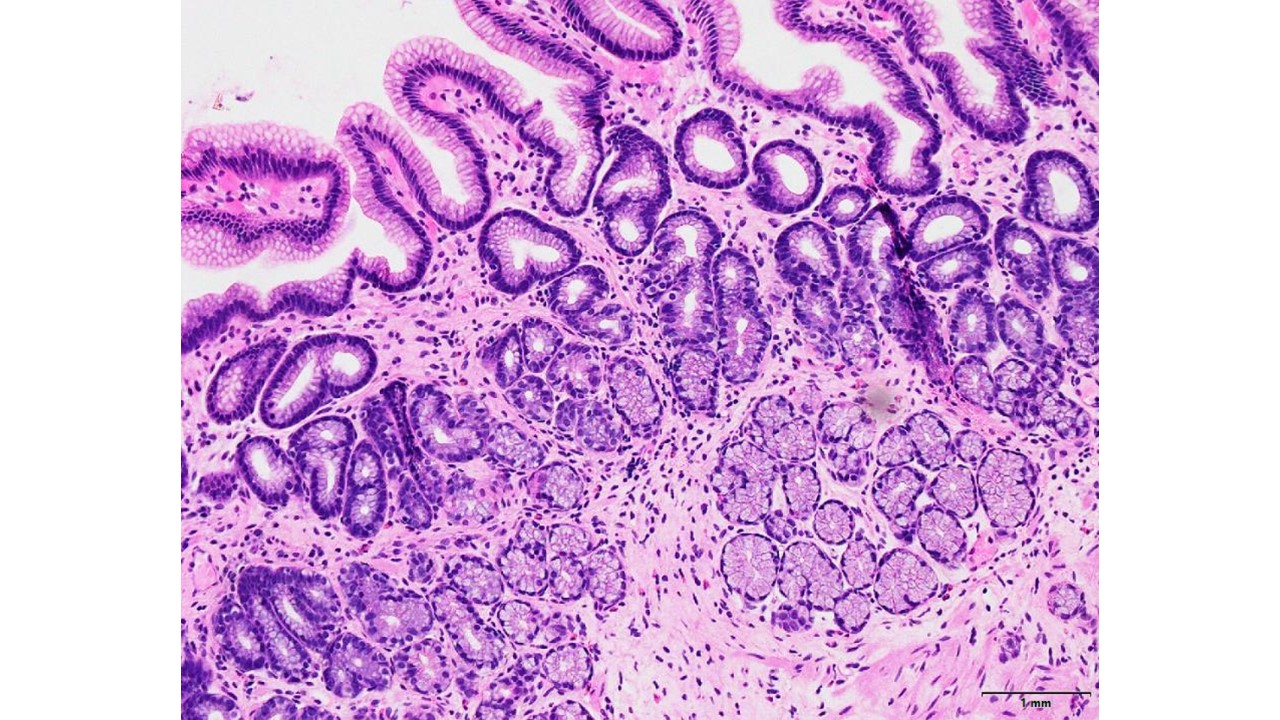
Figure: Figure B. Repeat EGD with biopsy: The antrum and gastric body showed mild chronic inactive gastritis.
Disclosures:
Mark Anthony Fallorina indicated no relevant financial relationships.
Jarin Prasa indicated no relevant financial relationships.
Yasar Ahtsham indicated no relevant financial relationships.
Joshua Diaz indicated no relevant financial relationships.
Michael Bernstein indicated no relevant financial relationships.
Mark Anthony Fallorina, MD1, Jarin Prasa, DO2, Yasar Ahtsham, MD3, Joshua Diaz, MD3, Michael Bernstein, MD1. P4217 - Clinical Dilemma in Eosinophilic Gastritis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 2NYC Health + Hospitals/South Brooklyn Health, New York, NY; 3South brooklyn Health, Brooklyn, NY
Introduction: Eosinophilic Gastrointestinal Disease (EGID) is a condition characterized by an abnormal presence of eosinophils in the gastrointestinal tract, without identifiable secondary causes, affecting approximately 6.3 out of 100,000 people in the U.S., mostly women with atopic conditions. Diagnosis typically occurs when biopsies show 20 or more eosinophils per high-power field (HPF) alongside gastrointestinal symptoms. The 2022 consensus introduced a classification system: eosinophilic gastritis (EoG) affects the stomach, eosinophilic enteritis (EoN) targets the small intestine, and eosinophilic colitis (EoC) impacts the colon. The mechanisms are still being studied, but immune responses to allergens are believed to play a significant role.
Case Description/
Methods: A 69-year-old female with a history of asthma with recent exacerbations on oral steroids, type 2 diabetes mellitus, and hypothyroidism presented with three weeks of nausea, vomiting, diarrhea, and poor oral intake. Imaging studies revealed a large hiatal hernia, while other diagnostic evaluations were negative. An initial esophagogastroduodenoscopy (EGD) with stomach biopsy showed eosinophilia, revealing 60-90 eosinophils per high power field (HPF) infiltrating the lamina propria and muscularis mucosa (Figure A). Following the initiation of high-dose steroid treatment, the patient exhibited marked clinical improvement. Follow up EGD confirmed the resolution of eosinophilic infiltration (Figure B), and was subsequently discharged with a steroid taper.
Discussion: The patient’s case raises questions about the interplay between the hiatal hernia and eosinophilic gastritis, in light of her history of oral steroid use due to recent asthma exacerbations and ongoing symptoms. Hiatal hernia may weaken the lower esophageal sphincter, which can lead to reflux of stomach acid and contents into the esophagus and, potentially, the stomach. Prolonged exposure to stomach acid could irritate the stomach lining and exacerbate the inflammatory response characteristic of eosinophilic gastritis (EoG). This cumulative pathological burden could potentially lead to complications related to EoG. Furthermore, the absence of established treatment guidelines for eosinophilic gastritis—where systemic corticosteroids are typically the standard treatment—highlights the urgent need for additional research to identify optimal therapeutic options for managing this condition.
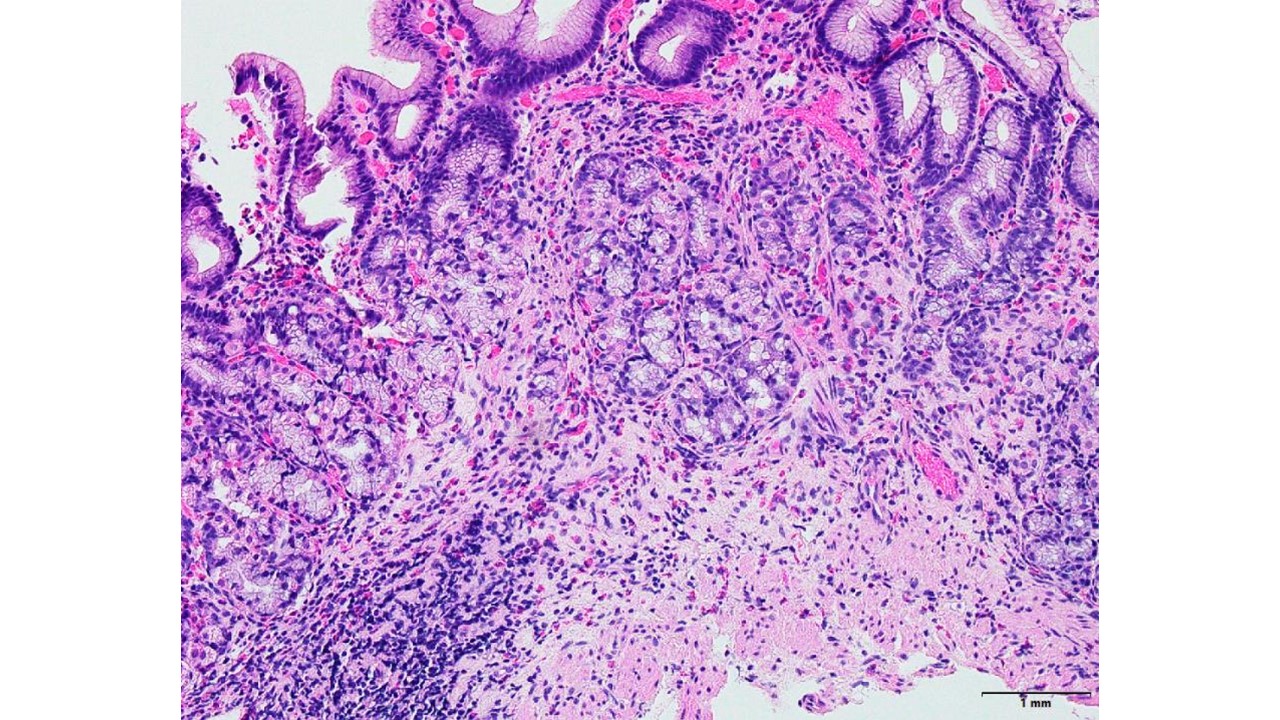
Figure: Figure A. Initial EGD with biopsy: Stomach body and antrum showed eosinophilic-rich gastritis. Small fragments of gastric oxyntic and antral type gastric mucosa with lamina propria edema and increased eosinophils ( 50-60 eosinophils per hpf). These eosinophils are primarily located within the lamina propria and the muscularis mucosa.
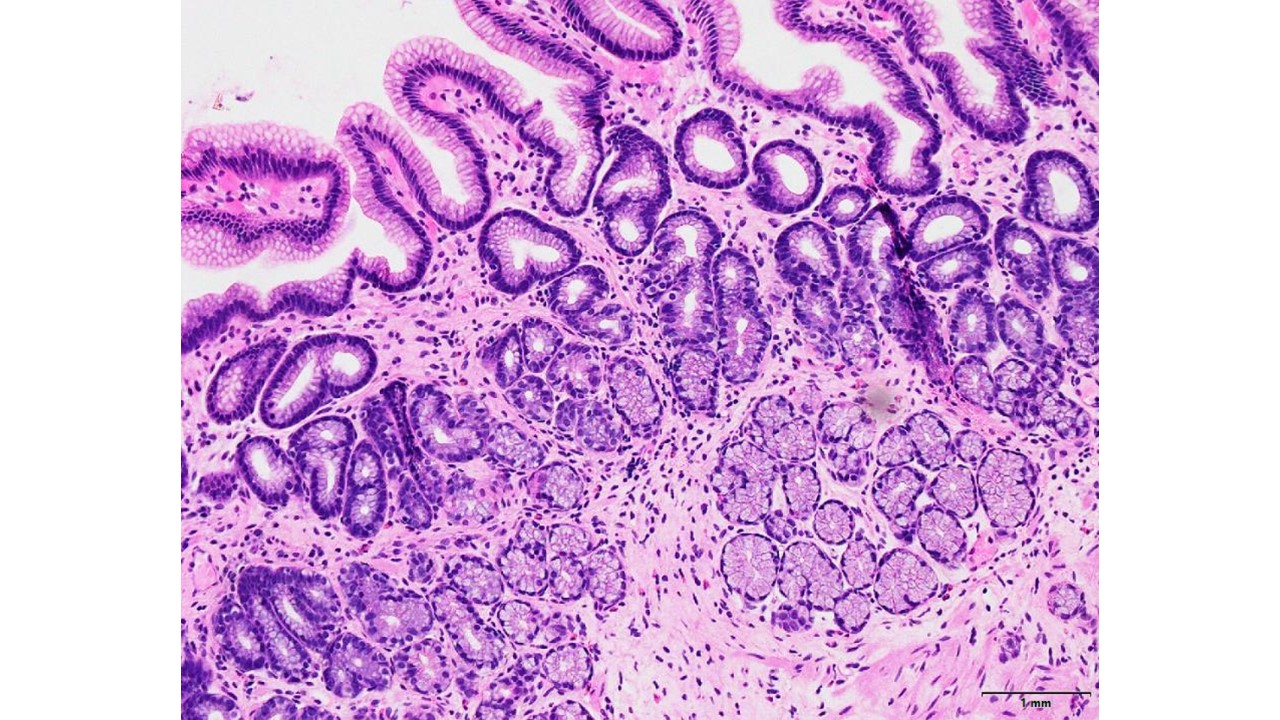
Figure: Figure B. Repeat EGD with biopsy: The antrum and gastric body showed mild chronic inactive gastritis.
Disclosures:
Mark Anthony Fallorina indicated no relevant financial relationships.
Jarin Prasa indicated no relevant financial relationships.
Yasar Ahtsham indicated no relevant financial relationships.
Joshua Diaz indicated no relevant financial relationships.
Michael Bernstein indicated no relevant financial relationships.
Mark Anthony Fallorina, MD1, Jarin Prasa, DO2, Yasar Ahtsham, MD3, Joshua Diaz, MD3, Michael Bernstein, MD1. P4217 - Clinical Dilemma in Eosinophilic Gastritis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
