Monday Poster Session
Category: Stomach and Spleen
P4215 - A Tale of Two Types: A Case of Amyloid Lambda Light Chain and Apolipoprotein A-IV Type Diagnosed on Endoscopic Biopsy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Venkat Arutla, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Venkat Arutla, MD1, Mark S. McFarland, MD, MSc2, Lucy A. Sheils, MD1
1Rochester General Hospital, Rochester, NY; 2Rochester General Hospital, Pittsford, NY
Introduction: Amyloidosis is a disease where amyloid fibrils deposit in various tissues and cause a multitude of symptoms. Gastrointestinal (GI) amyloidosis occurs when these fibrils deposit in the GI tract and cause symptoms such as weight loss, abdominal pain, and altered bowel movements. Here, we present a patient diagnosed with two concurrent types of GI amyloidosis.
Case Description/
Methods: A 70-year-old female with past medical history of chronic kidney disease stage III, hypertension and type 2 diabetes mellitus was initially referred to Hematology 3 years earlier for IgA lambda paraproteinemia. Initial bone marrow biopsy showed interstitial plasma cell infiltrate with 9-10% plasma cells, concerning for monoclonal gammopathy of undetermined significance (MGUS) or plasma cell myeloma. There was no report of amyloid in the bone marrow. Bone survey did not reveal radiographic evidence of myeloma, and she was managed with active surveillance. However, over the course of 3 years the patient was diagnosed with an elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) and unknown cause of heart failure with preserved ejection fraction. Interestingly, the pyrophosphate (PYP) scan was negative for cardiac amyloidosis. She then presented for an outpatient GI encounter with chief complaint of diarrhea, dysphagia and 50lbs of unintentional weight loss. She underwent esophagogastroduodenoscopy (EGD) with biopsies of areas with paleness and scattered erythema. The histology revealed submucosal perivascular hyaline deposits that were positive by Congo red stain, consistent with amyloid in both the stomach (Figures 1 and 2) and duodenum. Further peptide profiling detected both amyloid light chain (AL) lambda and apolipoprotein A-IV (AApoAIV) type amyloid. Repeat bone marrow biopsy showed hypercellular marrow with lambda light chain restricted plasma cell neoplasm and amyloid deposition. She was subsequently initiated on systemic therapy with Daratumumab, Cyclophosphamide, Bortezomib, and Dexamethasone (Dara-CyBorD).
Discussion: This case reveals a very rare diagnosis of two different types of amyloidosis, AL and AApoAIV. Although AL amyloidosis can be commonly found in the GI tract, AApoAIV is extremely rare. It is also interesting to note that multiple types of amyloid deposits typically do not present together. Furthermore, as PYP scan cannot diagnose cardiac amyloidosis due to AApoAIV, this patient’s endoscopic diagnosis may provide insight into the cause of the patient’s heart failure.
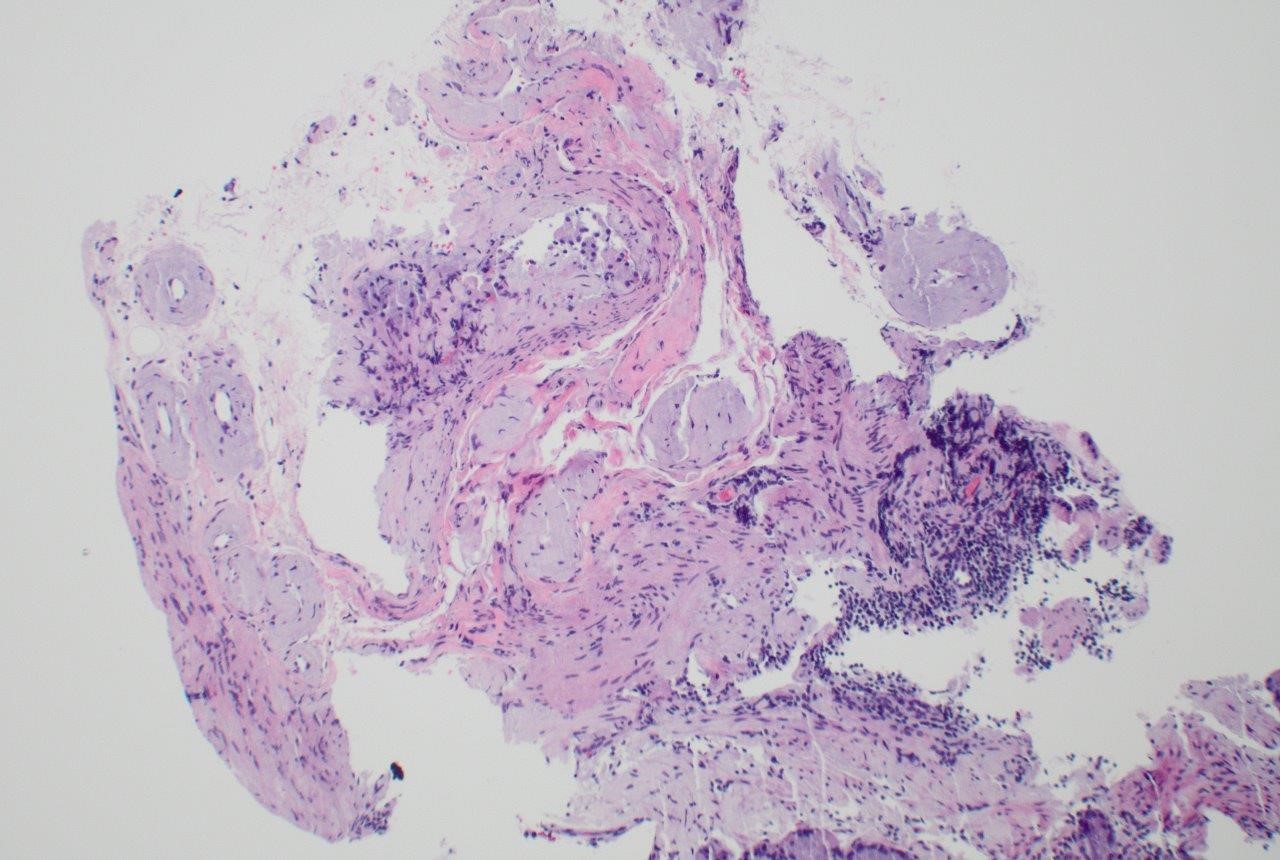
Figure: Figure 1: Hematoxylin & Eosin stain of stomach showing perivascular hyaline deposits in the submucosa.
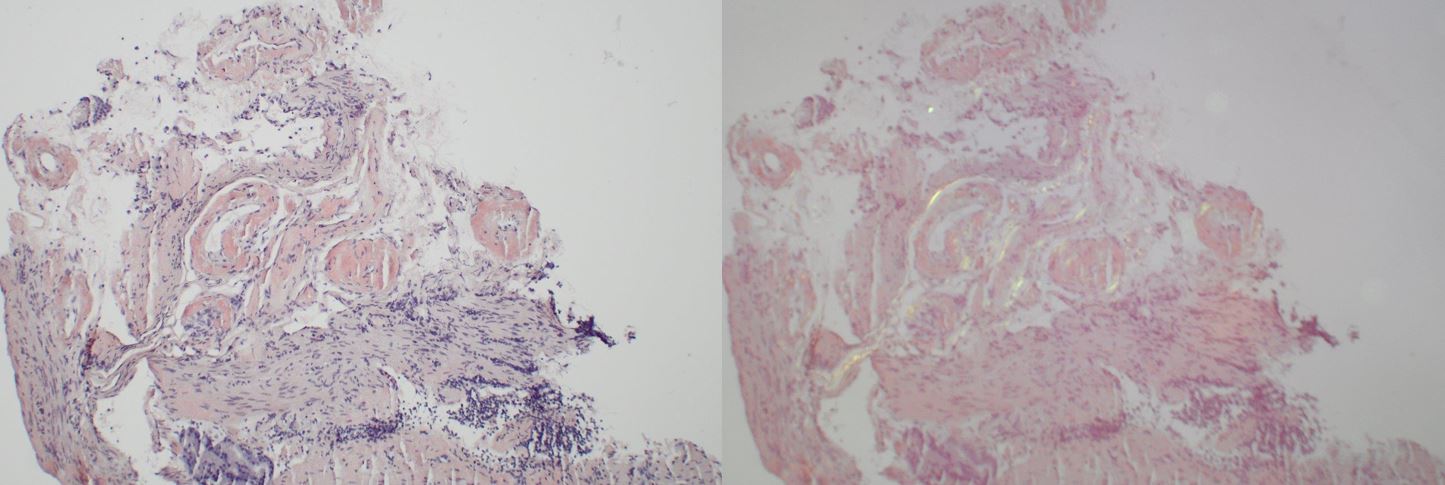
Figure: Figure 2: Congo red stain of stomach showing red-orange staining (left) and apple green birefringence (right) of perivascular hyaline deposits.
Disclosures:
Venkat Arutla indicated no relevant financial relationships.
Mark McFarland indicated no relevant financial relationships.
Lucy Sheils indicated no relevant financial relationships.
Venkat Arutla, MD1, Mark S. McFarland, MD, MSc2, Lucy A. Sheils, MD1. P4215 - A Tale of Two Types: A Case of Amyloid Lambda Light Chain and Apolipoprotein A-IV Type Diagnosed on Endoscopic Biopsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rochester General Hospital, Pittsford, NY
Introduction: Amyloidosis is a disease where amyloid fibrils deposit in various tissues and cause a multitude of symptoms. Gastrointestinal (GI) amyloidosis occurs when these fibrils deposit in the GI tract and cause symptoms such as weight loss, abdominal pain, and altered bowel movements. Here, we present a patient diagnosed with two concurrent types of GI amyloidosis.
Case Description/
Methods: A 70-year-old female with past medical history of chronic kidney disease stage III, hypertension and type 2 diabetes mellitus was initially referred to Hematology 3 years earlier for IgA lambda paraproteinemia. Initial bone marrow biopsy showed interstitial plasma cell infiltrate with 9-10% plasma cells, concerning for monoclonal gammopathy of undetermined significance (MGUS) or plasma cell myeloma. There was no report of amyloid in the bone marrow. Bone survey did not reveal radiographic evidence of myeloma, and she was managed with active surveillance. However, over the course of 3 years the patient was diagnosed with an elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) and unknown cause of heart failure with preserved ejection fraction. Interestingly, the pyrophosphate (PYP) scan was negative for cardiac amyloidosis. She then presented for an outpatient GI encounter with chief complaint of diarrhea, dysphagia and 50lbs of unintentional weight loss. She underwent esophagogastroduodenoscopy (EGD) with biopsies of areas with paleness and scattered erythema. The histology revealed submucosal perivascular hyaline deposits that were positive by Congo red stain, consistent with amyloid in both the stomach (Figures 1 and 2) and duodenum. Further peptide profiling detected both amyloid light chain (AL) lambda and apolipoprotein A-IV (AApoAIV) type amyloid. Repeat bone marrow biopsy showed hypercellular marrow with lambda light chain restricted plasma cell neoplasm and amyloid deposition. She was subsequently initiated on systemic therapy with Daratumumab, Cyclophosphamide, Bortezomib, and Dexamethasone (Dara-CyBorD).
Discussion: This case reveals a very rare diagnosis of two different types of amyloidosis, AL and AApoAIV. Although AL amyloidosis can be commonly found in the GI tract, AApoAIV is extremely rare. It is also interesting to note that multiple types of amyloid deposits typically do not present together. Furthermore, as PYP scan cannot diagnose cardiac amyloidosis due to AApoAIV, this patient’s endoscopic diagnosis may provide insight into the cause of the patient’s heart failure.
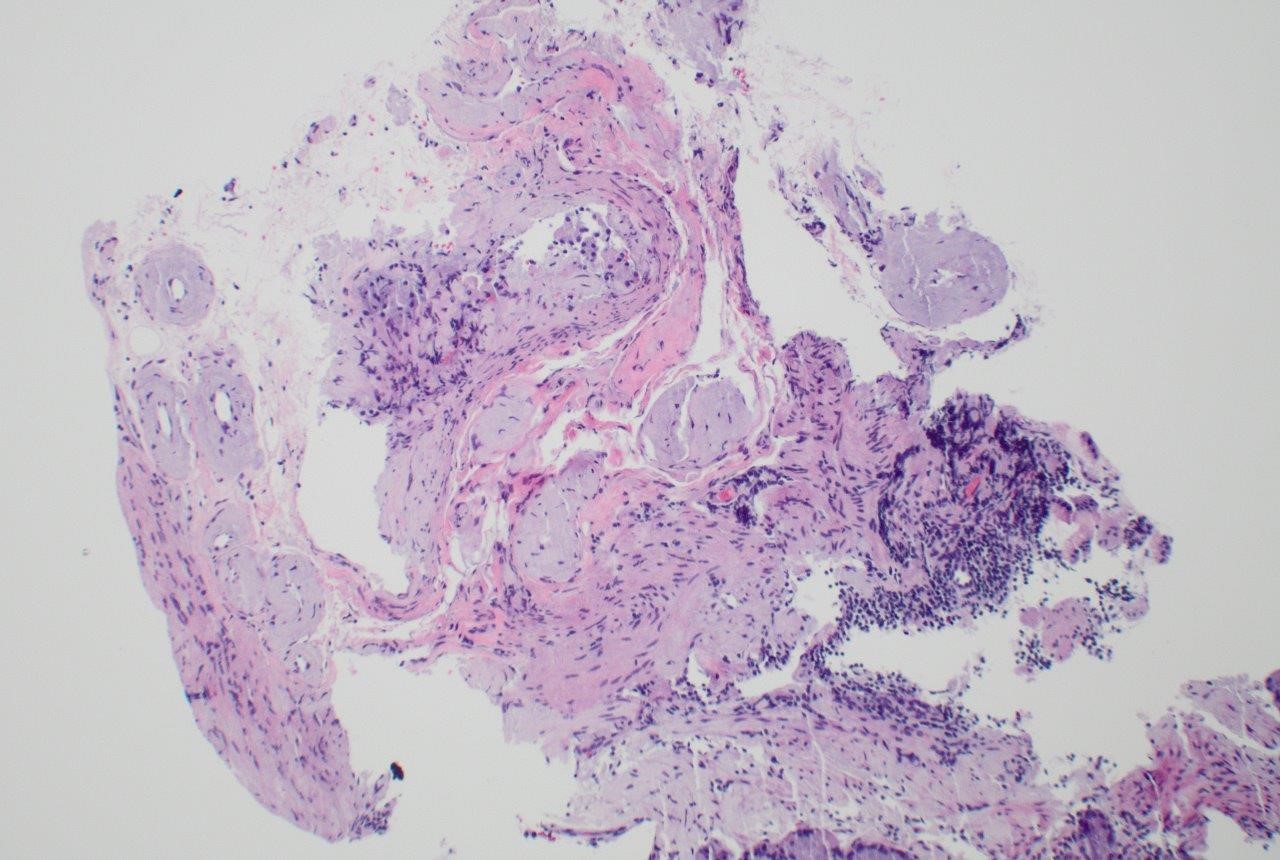
Figure: Figure 1: Hematoxylin & Eosin stain of stomach showing perivascular hyaline deposits in the submucosa.
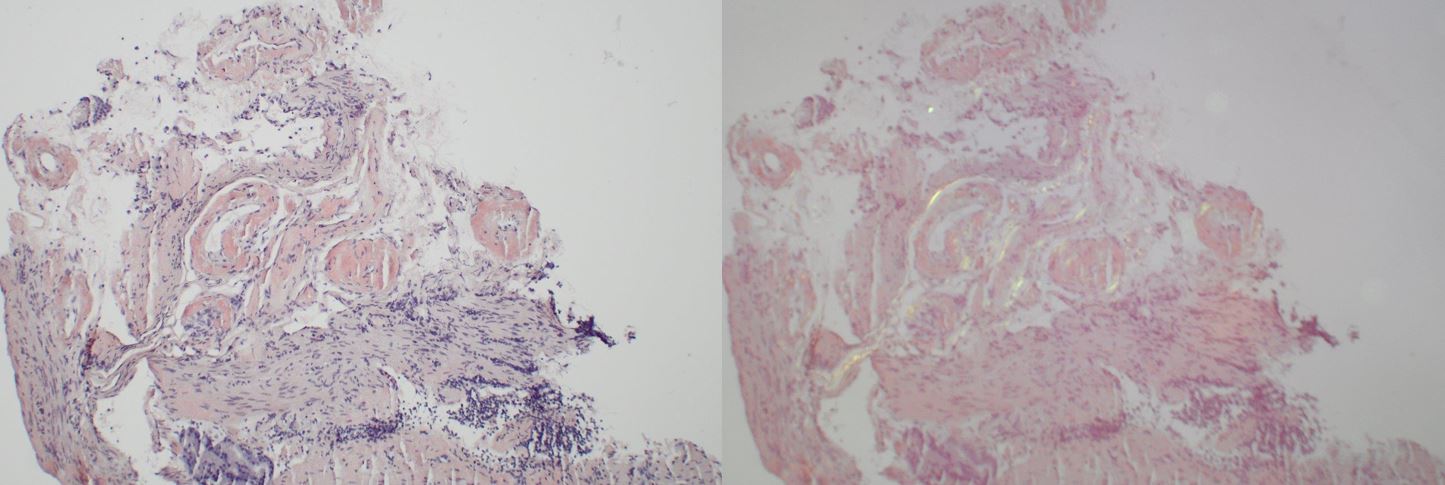
Figure: Figure 2: Congo red stain of stomach showing red-orange staining (left) and apple green birefringence (right) of perivascular hyaline deposits.
Disclosures:
Venkat Arutla indicated no relevant financial relationships.
Mark McFarland indicated no relevant financial relationships.
Lucy Sheils indicated no relevant financial relationships.
Venkat Arutla, MD1, Mark S. McFarland, MD, MSc2, Lucy A. Sheils, MD1. P4215 - A Tale of Two Types: A Case of Amyloid Lambda Light Chain and Apolipoprotein A-IV Type Diagnosed on Endoscopic Biopsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
