Monday Poster Session
Category: Stomach and Spleen
Two <i>Pylori</i> Are Not Better Than One
P4202 - Two H. pylori Are Not Better Than One
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Maryanna Schweininger, DO (she/her/hers)
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Gabriella DeStefano, BS1, Krysta Contino, MD2, Maryanna Schweininger, DO3
1Cooper Medical School of Rowan University, Dorothy, NJ; 2Cooper Health Gastroenterology, Mount Laurel, NJ; 3Cooper University Hospital, Camden, NJ
Introduction: Peptic ulcer disease (PUD) is characterized by disruption of the gastrointestinal (GI) tract lining due to an excess of gastric acid. If untreated or poorly managed, PUD can lead to consequences such as upper GI tract bleeding, gastric outlet obstruction, or perforation. Uncommonly, peptic ulcers can erode to such an extent that a fistula is created between the stomach and duodenal bulb, resulting in an acquired “double pylorus.” The presence of a double pylorus has a reported prevalence of 0.001%-0.4% in all esophagogastroduodenoscopies (EGD). This case highlights a rare occurrence of a double pylorus in a patient with a history of gastroesophageal reflux disease (GERD) and PUD and aims to raise awareness of this uncommon anatomical finding.
Case Description/
Methods: This is the case of a 60 year-old man with a history of GERD and PUD, who presented with severe reflux symptoms. Previous EGDs in 2014 revealed esophagitis, a pyloric ulcer, and a possible fistula beneath the ulcer. In 2015, a repeat EGD showed healing of the ulcer. In 2024, he expressed worsening reflux symptoms, prompting a follow-up EGD, which identified a gastric fistula and a nonbleeding gastric ulcer. Pathology from random gastric biopsies showed intestinal metaplasia, but the ulcer identified no metaplasia or malignancy. He was treated with pantoprazole 40 mg twice daily and carafate 4 times daily. Follow up endoscopy showed persistence of a double pylorus with small area of erosion.
Discussion: Most cases of a double pylorus are the result of peptic ulcer erosion, but congenital double pylorus has also been reported. Given this patient's history of PUD and ulcer at the site of the fistula suggests an acquired double pylorus. Increasing awareness of this rare pathology will lead to increased recognition of this entity, particularly in the setting of PUD. Early identification can aid in more accurate diagnosis and improved management. Additionally, heightened awareness can enhance the safety of EGDs in this setting with improved patient outcomes.
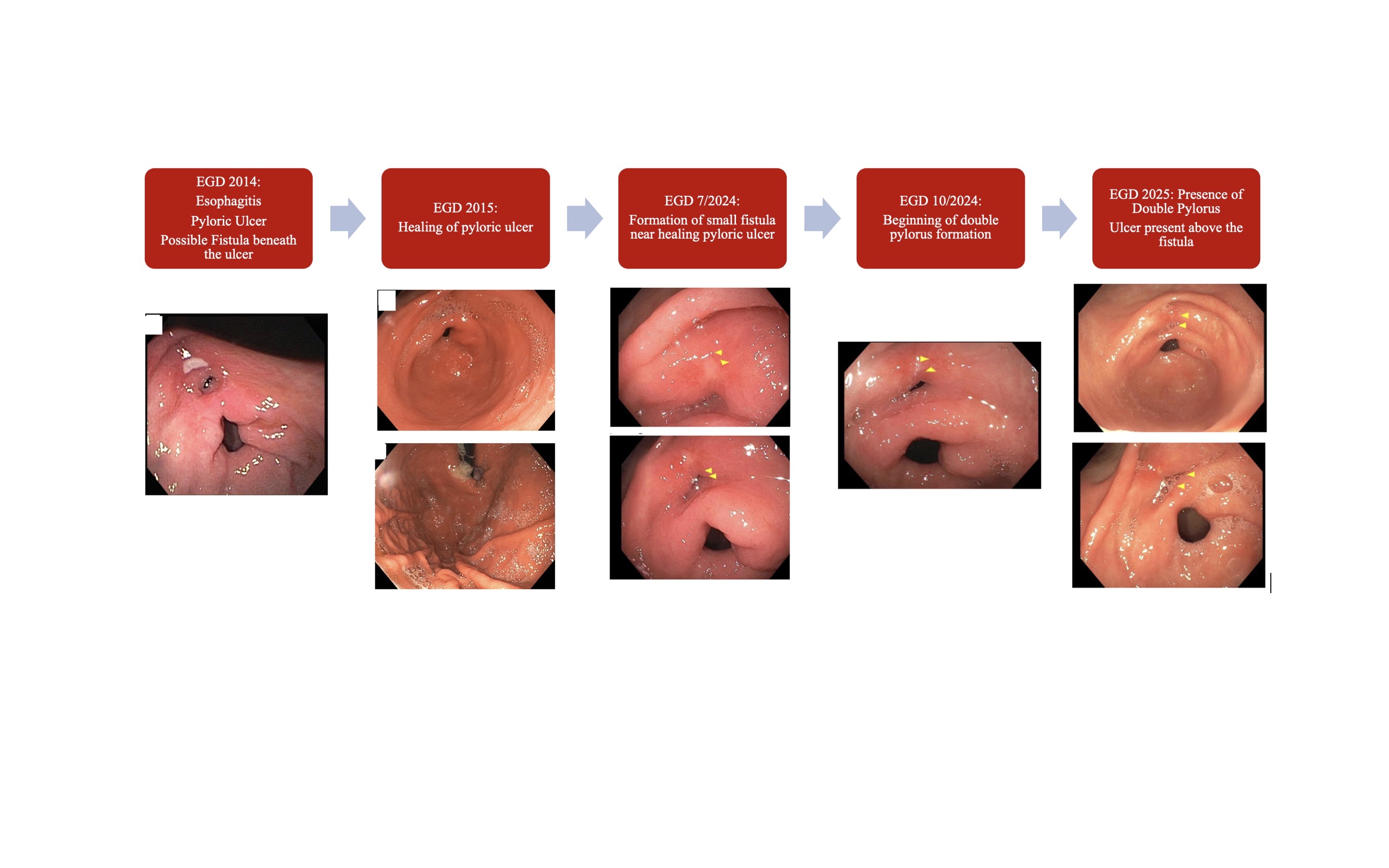
Figure: This image depicts the progression of the double pylorus formation through subsequent EGDs
Disclosures:
Gabriella DeStefano indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Gabriella DeStefano, BS1, Krysta Contino, MD2, Maryanna Schweininger, DO3. P4202 - Two <i>Pylori</i> Are Not Better Than One, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper Medical School of Rowan University, Dorothy, NJ; 2Cooper Health Gastroenterology, Mount Laurel, NJ; 3Cooper University Hospital, Camden, NJ
Introduction: Peptic ulcer disease (PUD) is characterized by disruption of the gastrointestinal (GI) tract lining due to an excess of gastric acid. If untreated or poorly managed, PUD can lead to consequences such as upper GI tract bleeding, gastric outlet obstruction, or perforation. Uncommonly, peptic ulcers can erode to such an extent that a fistula is created between the stomach and duodenal bulb, resulting in an acquired “double pylorus.” The presence of a double pylorus has a reported prevalence of 0.001%-0.4% in all esophagogastroduodenoscopies (EGD). This case highlights a rare occurrence of a double pylorus in a patient with a history of gastroesophageal reflux disease (GERD) and PUD and aims to raise awareness of this uncommon anatomical finding.
Case Description/
Methods: This is the case of a 60 year-old man with a history of GERD and PUD, who presented with severe reflux symptoms. Previous EGDs in 2014 revealed esophagitis, a pyloric ulcer, and a possible fistula beneath the ulcer. In 2015, a repeat EGD showed healing of the ulcer. In 2024, he expressed worsening reflux symptoms, prompting a follow-up EGD, which identified a gastric fistula and a nonbleeding gastric ulcer. Pathology from random gastric biopsies showed intestinal metaplasia, but the ulcer identified no metaplasia or malignancy. He was treated with pantoprazole 40 mg twice daily and carafate 4 times daily. Follow up endoscopy showed persistence of a double pylorus with small area of erosion.
Discussion: Most cases of a double pylorus are the result of peptic ulcer erosion, but congenital double pylorus has also been reported. Given this patient's history of PUD and ulcer at the site of the fistula suggests an acquired double pylorus. Increasing awareness of this rare pathology will lead to increased recognition of this entity, particularly in the setting of PUD. Early identification can aid in more accurate diagnosis and improved management. Additionally, heightened awareness can enhance the safety of EGDs in this setting with improved patient outcomes.
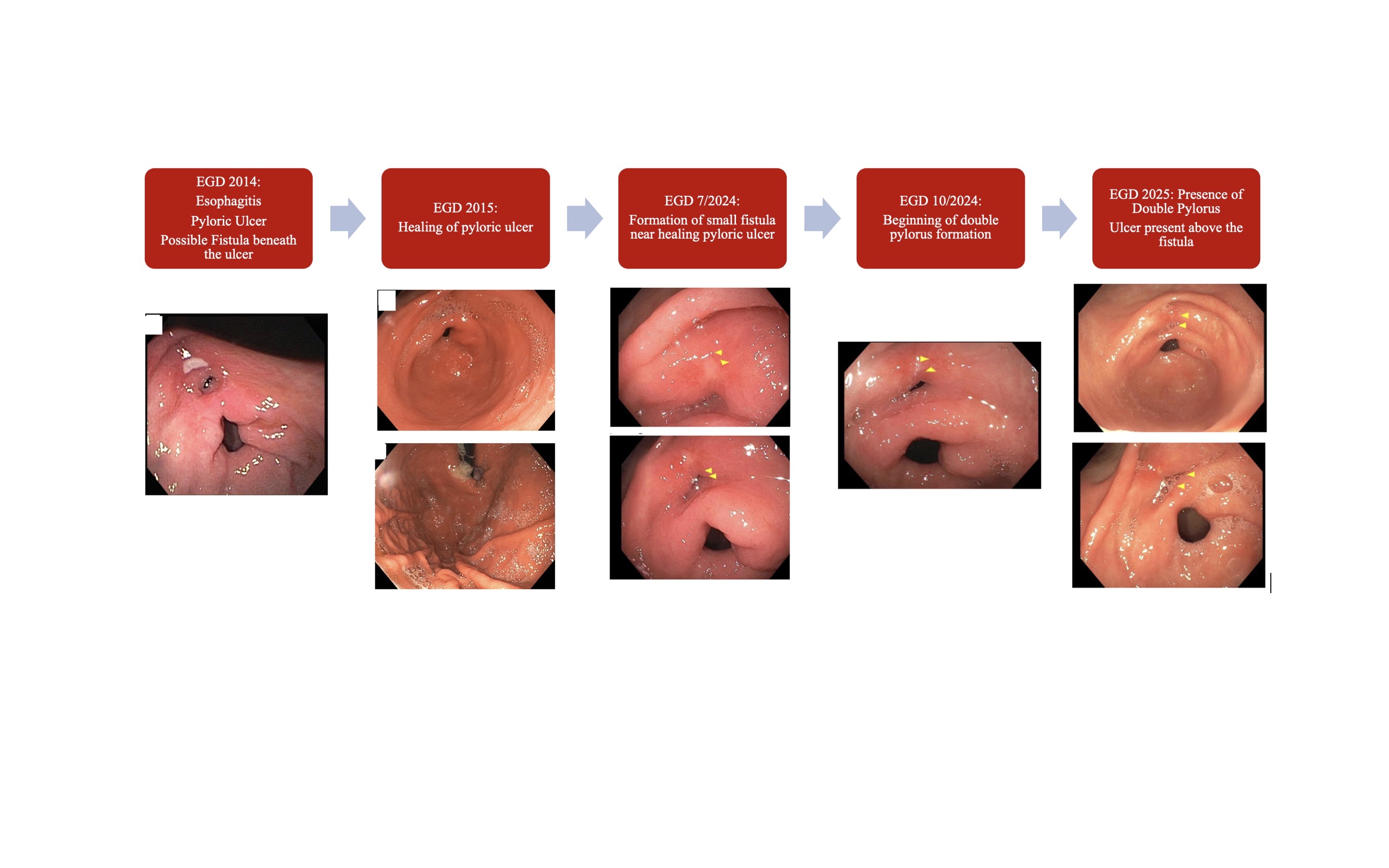
Figure: This image depicts the progression of the double pylorus formation through subsequent EGDs
Disclosures:
Gabriella DeStefano indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Gabriella DeStefano, BS1, Krysta Contino, MD2, Maryanna Schweininger, DO3. P4202 - Two <i>Pylori</i> Are Not Better Than One, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
