Monday Poster Session
Category: Stomach and Spleen
P4200 - Fundal Foveolar Adenomatous Polyposis in Gardner’s Syndrome: Is EUS a Good Option to Detect Invasion?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hussam Almasri, MD, MRCP(UK)
University of North Dakota, School of Medicine and Health Sciences
Fargo, ND
Presenting Author(s)
Hussam Almasri, MD, MRCP(UK)1, Emilee Ohman, BS1, Rita Ahmad, MD1, Guneet Sidhu, MD1, John Bassett, MD2
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Gardner syndrome (GC) is a subtype of familial adenomatous polyposis syndrome (FAP), a rare autosomal dominant condition involving mutation of the APC gene with near-complete penetrance and variable expressivity. (GC) is associated with both extensive intestinal polyposis and extra-intestinal manifestations. Nearly 10% of patients with FAP syndrome will develop gastric polyposis, and the risk of gastric cancer is about 0.6%. It is recommended that patients with FAP undergo upper endoscopy screening primarily for early detection of duodenal adenocarcinoma. The utility of endoscopic ultrasound (EUS) for the assessment of gastric polyposis in this population is not well established. We present a case of GC who underwent assessment for large adenomatous gastric polyps with dysplasia.
Case Description/
Methods: 59-year-old female with Gardner’s syndrome confirmed by genetic testing, with a history of total colectomy. She also has a positive family history of GC with gastrectomy for an unclear indication. She presented for yearly surveillance EGD for gastric polyposis. It was noted that the largest polyp that was in the fundus had grown in size from 3 to 6 cm in 6 months. During the same time, the patient complained of increased symptoms of indigestion. EUS showed signs of submucosal invasion without muscularis propria involvement (Figure 1). A trial for en-block resection was unsuccessful. Histopathology examination showed fragments of foveolar polyps, and the immunohistochemical stain was negative for Helicobacter pylori. CT scan did not show significant peri-gastric lymphadenopathy. Given high-risk features, the decision was made to proceed with surgery. The patient underwent a total gastrectomy with a Roux-en-Y esophagojejunostomy. Histopathology showed innumerable polyposis with features of foveolar adenomas and low-grade dysplasia.
Discussion: Gastric polyposis in GC can be difficult to assess properly. Nearly 50% of patients with FAP will develop foveolar dysplasia. However, the risk of progression to gastric cancer is low. Biopsies and standard polypectomy techniques seem to be suboptimal measures to rule out the development of adenocarcinoma. On the other hand, while EUS is recommended for the evaluation of gastric/duodenal submucosal lesions, its utility in mucosal-based gastric polyps is limited, and thus the interpretation of EUS findings in these patients should be interpreted carefully.
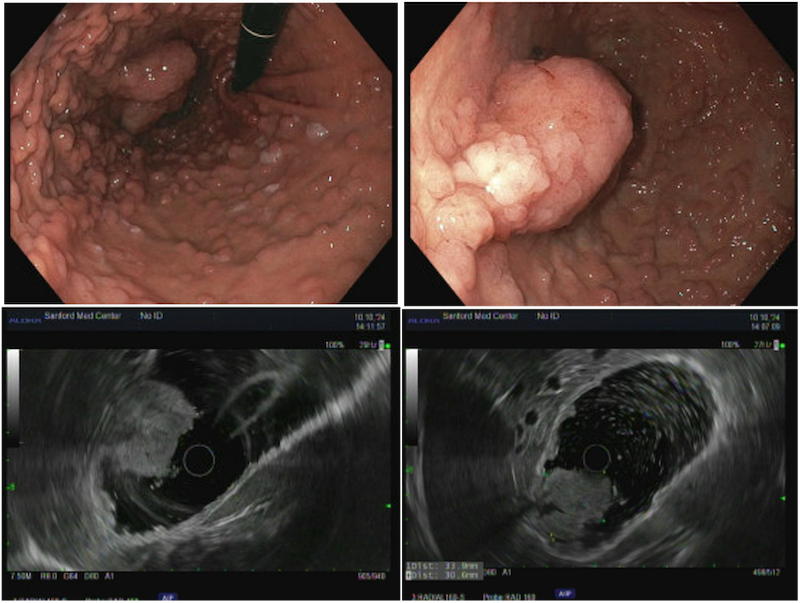
Figure: Figure 1A+B endoscopic visualization of the gastric fundus, showing extensive polyposis. C+D Large polyp under EUS imaging, showing signs of invasion to the submucosa
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Emilee Ohman indicated no relevant financial relationships.
Rita Ahmad indicated no relevant financial relationships.
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP(UK)1, Emilee Ohman, BS1, Rita Ahmad, MD1, Guneet Sidhu, MD1, John Bassett, MD2. P4200 - Fundal Foveolar Adenomatous Polyposis in Gardner’s Syndrome: Is EUS a Good Option to Detect Invasion?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Gardner syndrome (GC) is a subtype of familial adenomatous polyposis syndrome (FAP), a rare autosomal dominant condition involving mutation of the APC gene with near-complete penetrance and variable expressivity. (GC) is associated with both extensive intestinal polyposis and extra-intestinal manifestations. Nearly 10% of patients with FAP syndrome will develop gastric polyposis, and the risk of gastric cancer is about 0.6%. It is recommended that patients with FAP undergo upper endoscopy screening primarily for early detection of duodenal adenocarcinoma. The utility of endoscopic ultrasound (EUS) for the assessment of gastric polyposis in this population is not well established. We present a case of GC who underwent assessment for large adenomatous gastric polyps with dysplasia.
Case Description/
Methods: 59-year-old female with Gardner’s syndrome confirmed by genetic testing, with a history of total colectomy. She also has a positive family history of GC with gastrectomy for an unclear indication. She presented for yearly surveillance EGD for gastric polyposis. It was noted that the largest polyp that was in the fundus had grown in size from 3 to 6 cm in 6 months. During the same time, the patient complained of increased symptoms of indigestion. EUS showed signs of submucosal invasion without muscularis propria involvement (Figure 1). A trial for en-block resection was unsuccessful. Histopathology examination showed fragments of foveolar polyps, and the immunohistochemical stain was negative for Helicobacter pylori. CT scan did not show significant peri-gastric lymphadenopathy. Given high-risk features, the decision was made to proceed with surgery. The patient underwent a total gastrectomy with a Roux-en-Y esophagojejunostomy. Histopathology showed innumerable polyposis with features of foveolar adenomas and low-grade dysplasia.
Discussion: Gastric polyposis in GC can be difficult to assess properly. Nearly 50% of patients with FAP will develop foveolar dysplasia. However, the risk of progression to gastric cancer is low. Biopsies and standard polypectomy techniques seem to be suboptimal measures to rule out the development of adenocarcinoma. On the other hand, while EUS is recommended for the evaluation of gastric/duodenal submucosal lesions, its utility in mucosal-based gastric polyps is limited, and thus the interpretation of EUS findings in these patients should be interpreted carefully.
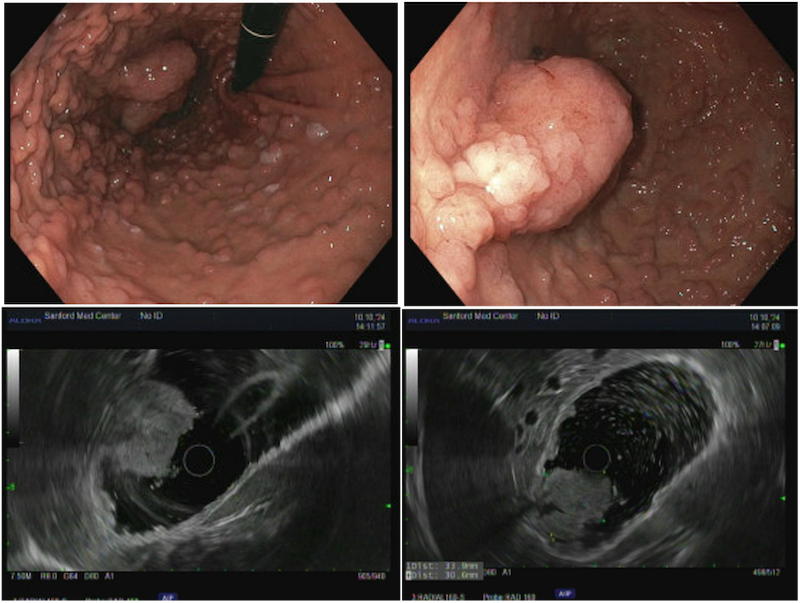
Figure: Figure 1A+B endoscopic visualization of the gastric fundus, showing extensive polyposis. C+D Large polyp under EUS imaging, showing signs of invasion to the submucosa
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Emilee Ohman indicated no relevant financial relationships.
Rita Ahmad indicated no relevant financial relationships.
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP(UK)1, Emilee Ohman, BS1, Rita Ahmad, MD1, Guneet Sidhu, MD1, John Bassett, MD2. P4200 - Fundal Foveolar Adenomatous Polyposis in Gardner’s Syndrome: Is EUS a Good Option to Detect Invasion?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
