Monday Poster Session
Category: Stomach and Spleen
P4194 - Trends and Disparities in Mortality Rates Due to Upper GI Ulcers in the United States Over the Past 20 Years: A CDC WONDER Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kashif Ali, MD
University of Texas Rio Grande Valley
Edinburg, TX
Presenting Author(s)
Kashif Ali, MD1, Asif Zamir, MD, FACG2
1University of Texas Rio Grande Valley, Edinburg, TX; 2DHR Health Gastroenterology, Edinburg, TX
Introduction: Gastrointestinal tract ulcers carry significant risk when associated with complications such as bleeding and perforation, often requiring surgical or endoscopic intervention. Our study aims to analyze trends in mortality rates over the past two decades in the United States.
Methods: A retrospective study was conducted using the CDC WONDER dataset. Mortality trends were calculated by identifying ICD-10 codes for gastric ulcer (K25), duodenal ulcer (K26), peptic ulcer (K27), and gastrojejunal ulcer (K28). Crude mortality rates per 100,000 and annual percentage change (APC) with 95% confidence intervals were calculated using Join point software.
Results: Our study shows that a total of 76,444 people died from upper gastrointestinal (GI) ulcer complications—including hemorrhage and perforation—between 1999 and 2020 in the United States. Of these, males accounted for 50.5% of the deaths. Our study shows an increasing APC among American Indians starting in 2004 (APC 2.33), Asian or Pacific Islanders showed an increasing APC of 4.36 since 2011. Black or African Americans had a rising APC of 2.53 beginning in 2012, while White individuals had an increasing APC of 4.76% starting in 2015. Geographic trends also showed rising mortality in both urban and rural settings. Large central metro areas saw an increase in mortality beginning in 2009 (APC 1.01%), and large fringe metros showed a more pronounced rise starting in 2014 (APC 4.35%). Medium metro areas had an increasing trend since 2011 (APC 2.9). Mortality rose in small metro areas from 2017 onward (APC 7.67%), and non-metro regions experienced a steady increase as well (APC 4.04% through 2020). By age group, mortality has been increasing among individuals aged 55–64, with an APC of 1.88 since 2007. The 65–74 age group showed a significant rise, with an APC of 11.8 since 2018. Additionally, the 75–84 age group had an increasing APC of 1.99 starting in 2014. Texas was found to have the highest increase in mortality trend, with an APC of 10.1% since 2016, followed by Nevada with an APC of 8.86% since 2008.
Discussion: Our study shows that mortality rates due to upper GI ulcers have been on the rise over the past decade in the United States. Smaller towns and rural areas demonstrated higher increases in mortality compared to larger metropolitan areas. Among racial groups, White individuals experienced the most significant increase in mortality over the last decade. Geographically, Texas had the highest rise in mortality, followed by Nevada.
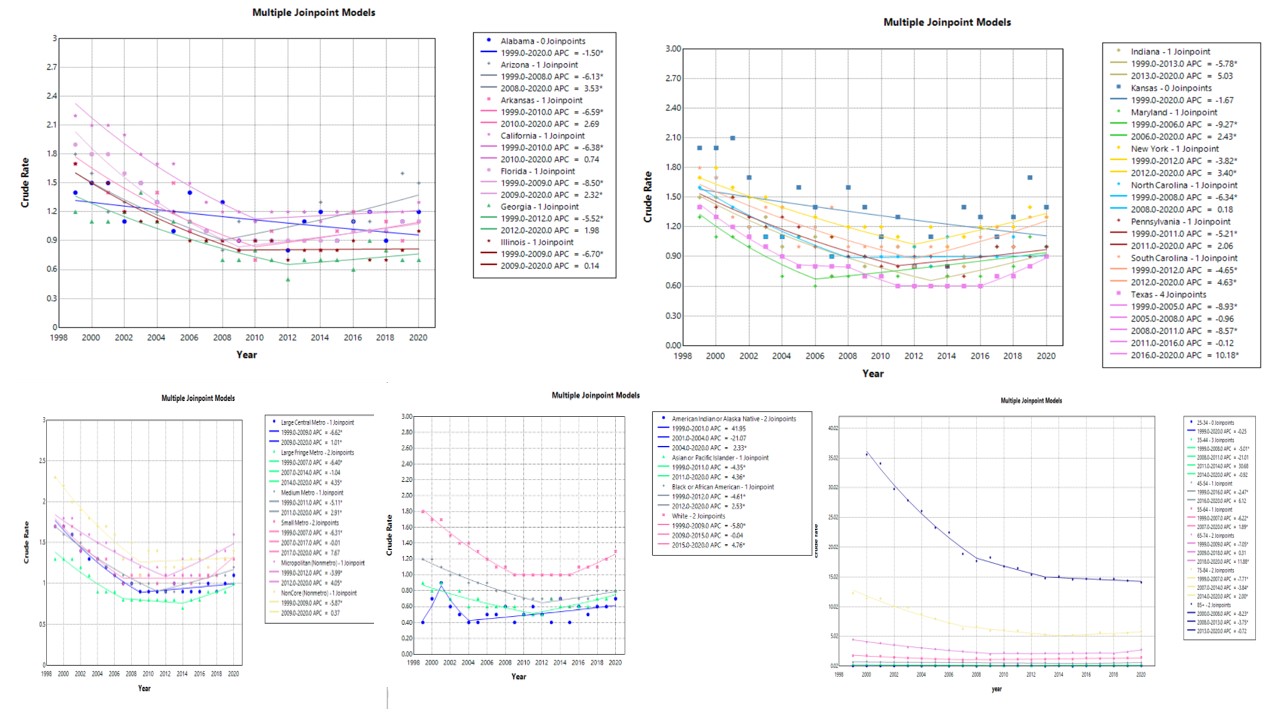
Figure: Mortality trends of Upper GI Ulcer over past 2 decades in United States.
Disclosures:
Kashif Ali indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Kashif Ali, MD1, Asif Zamir, MD, FACG2. P4194 - Trends and Disparities in Mortality Rates Due to Upper GI Ulcers in the United States Over the Past 20 Years: A CDC WONDER Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Rio Grande Valley, Edinburg, TX; 2DHR Health Gastroenterology, Edinburg, TX
Introduction: Gastrointestinal tract ulcers carry significant risk when associated with complications such as bleeding and perforation, often requiring surgical or endoscopic intervention. Our study aims to analyze trends in mortality rates over the past two decades in the United States.
Methods: A retrospective study was conducted using the CDC WONDER dataset. Mortality trends were calculated by identifying ICD-10 codes for gastric ulcer (K25), duodenal ulcer (K26), peptic ulcer (K27), and gastrojejunal ulcer (K28). Crude mortality rates per 100,000 and annual percentage change (APC) with 95% confidence intervals were calculated using Join point software.
Results: Our study shows that a total of 76,444 people died from upper gastrointestinal (GI) ulcer complications—including hemorrhage and perforation—between 1999 and 2020 in the United States. Of these, males accounted for 50.5% of the deaths. Our study shows an increasing APC among American Indians starting in 2004 (APC 2.33), Asian or Pacific Islanders showed an increasing APC of 4.36 since 2011. Black or African Americans had a rising APC of 2.53 beginning in 2012, while White individuals had an increasing APC of 4.76% starting in 2015. Geographic trends also showed rising mortality in both urban and rural settings. Large central metro areas saw an increase in mortality beginning in 2009 (APC 1.01%), and large fringe metros showed a more pronounced rise starting in 2014 (APC 4.35%). Medium metro areas had an increasing trend since 2011 (APC 2.9). Mortality rose in small metro areas from 2017 onward (APC 7.67%), and non-metro regions experienced a steady increase as well (APC 4.04% through 2020). By age group, mortality has been increasing among individuals aged 55–64, with an APC of 1.88 since 2007. The 65–74 age group showed a significant rise, with an APC of 11.8 since 2018. Additionally, the 75–84 age group had an increasing APC of 1.99 starting in 2014. Texas was found to have the highest increase in mortality trend, with an APC of 10.1% since 2016, followed by Nevada with an APC of 8.86% since 2008.
Discussion: Our study shows that mortality rates due to upper GI ulcers have been on the rise over the past decade in the United States. Smaller towns and rural areas demonstrated higher increases in mortality compared to larger metropolitan areas. Among racial groups, White individuals experienced the most significant increase in mortality over the last decade. Geographically, Texas had the highest rise in mortality, followed by Nevada.
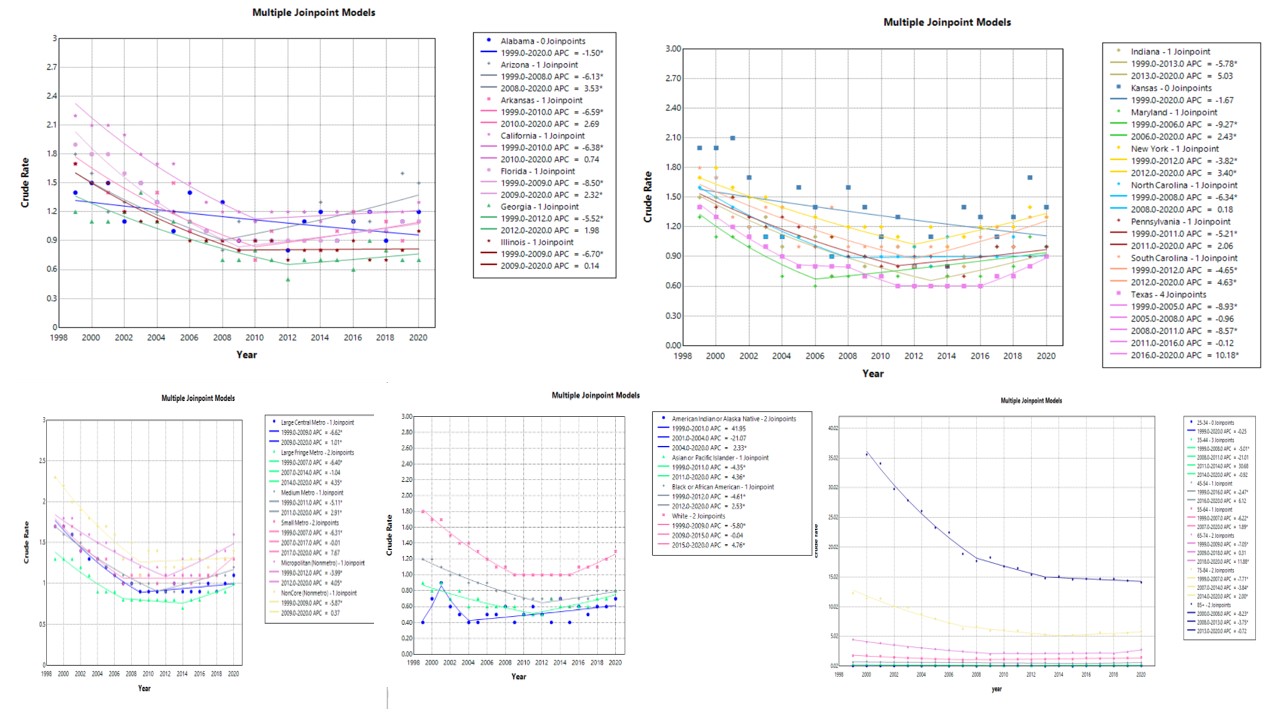
Figure: Mortality trends of Upper GI Ulcer over past 2 decades in United States.
Disclosures:
Kashif Ali indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Kashif Ali, MD1, Asif Zamir, MD, FACG2. P4194 - Trends and Disparities in Mortality Rates Due to Upper GI Ulcers in the United States Over the Past 20 Years: A CDC WONDER Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
