Monday Poster Session
Category: Stomach and Spleen
P4187 - Inpatient Outcomes of Peptic Ulcer Disease in HIV-Positive Patients in the United States
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pooja Viswanath, MS, DO
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Pooja Viswanath, MS, DO1, Sushrruti Varatharaj, DO1, Abhishek Patel, MD1, Abdelrahman Yousef, MD2, Mohammed Quazi, PhD3, Abu Baker Sheikh, MD1
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico Hospital, Albuquerque, NM; 3West Virginia University, Morgantown, WV
Introduction: Peptic ulcer disease (PUD) remains a major cause of global morbidity and mortality, with annual deaths exceeding 250,000. In patients with Human Immunodeficiency Virus (HIV), prior studies suggest a reduced incidence of PUD, likely due to lower gastric acid production and altered physiology. However, the burden of inpatient complications and outcomes in HIV-positive (HIV+) patients with PUD remains under explored. This study evaluates the impact of HIV on PUD-related inpatient outcomes, complications, and healthcare resource utilization using national-level data.
Methods: We conducted a retrospective analysis of the National Inpatient Sample (2016–2021), identifying adults hospitalized with PUD, stratified by HIV status. Multivariable logistic regression adjusted for age, gender, race, Elixhauser comorbidity index, insurance, hospital teaching status, and bed size. Outcomes included in-hospital mortality, complications, resource utilization, and procedures.
Results: Among 200,830 patients with PUD, 835 (0.42%) were HIV+. HIV+ patients were younger (mean age: 56.3 vs. 66.2 years), predominantly male (72.5% vs. 52.1%, p< 0.001), Black (46.7% vs. 13.1%), and on Medicaid (34.1% vs. 12.7%, p< 0.001). HIV+ patients had higher rates of drug abuse (13.2% vs. 4.0%, p< 0.001), and smoking (52.1% vs. 39.5%, p< 0.001), but lower rates of hypertension (53.3% vs. 66.1%, p< 0.001) and obesity (8.4% vs. 15.7%, p< 0.001). Adjusted analyses showed significantly higher odds of in-hospital mortality (aOR: 2.34, 95% CI: 1.33–4.10, p= 0.003) and acute kidney injury requiring hemodialysis (aOR: 1.97, 95% CI: 1.18–3.27, p= 0.009) in HIV+ patients. Helicobacter pylori detection was markedly lower in HIV+ patients (aOR: 0.19, 95% CI: 0.05–0.75, p= 0.018). Adjusted costs were $35,099.28 higher (p= 0.025), and lengths of stay were 1.03 days longer (p= 0.189). Utilization of upper endoscopy and transfusion procedures were similar.
Discussion: HIV has been associated with a lower incidence of PUD due to reduced gastric acid production. Hospitalized HIV+ patients with PUD experience significantly worse outcomes with increased in-hospital mortality, higher likelihood of renal failure requiring hemodialysis, and prolonged hospital stay. The significantly lower odds of Helicobacter pylori detection suggest alternative ulcer etiologies such as medication-induced ulcers, opportunistic infections (e.g., CMV), or non-H. pylori dyspepsia, underscoring the need for tailored diagnostic strategies.
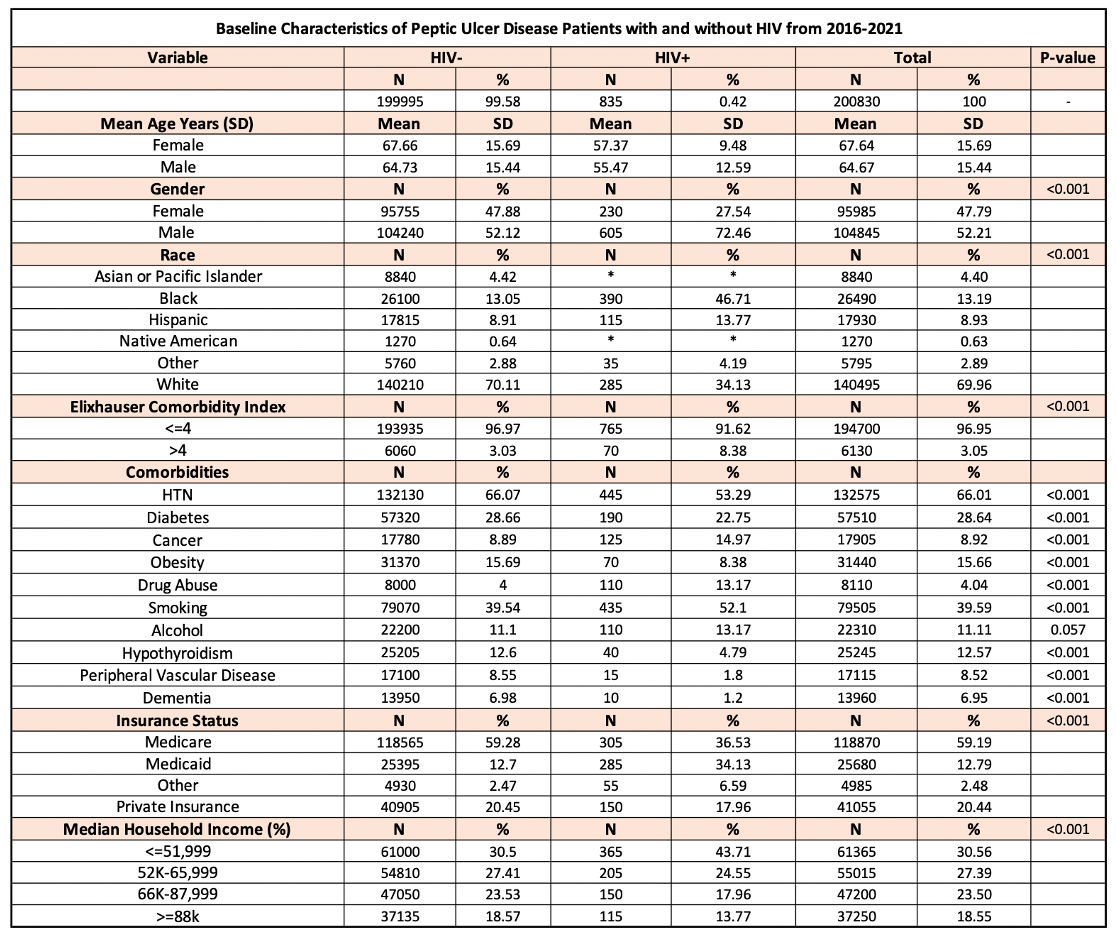
Figure: Table 1: Demographic characteristics of patients with Peptic Ulcer Disease stratified by HIV status including mean age years, gender, race, Elixhauser comorbidity index, comorbidities, insurance status and median household income.

Figure: Table 2: Inpatient outcomes in Peptic Ulcer Disease patients with HIV.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Sushrruti Varatharaj indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Abdelrahman Yousef indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Sushrruti Varatharaj, DO1, Abhishek Patel, MD1, Abdelrahman Yousef, MD2, Mohammed Quazi, PhD3, Abu Baker Sheikh, MD1. P4187 - Inpatient Outcomes of Peptic Ulcer Disease in HIV-Positive Patients in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico Hospital, Albuquerque, NM; 3West Virginia University, Morgantown, WV
Introduction: Peptic ulcer disease (PUD) remains a major cause of global morbidity and mortality, with annual deaths exceeding 250,000. In patients with Human Immunodeficiency Virus (HIV), prior studies suggest a reduced incidence of PUD, likely due to lower gastric acid production and altered physiology. However, the burden of inpatient complications and outcomes in HIV-positive (HIV+) patients with PUD remains under explored. This study evaluates the impact of HIV on PUD-related inpatient outcomes, complications, and healthcare resource utilization using national-level data.
Methods: We conducted a retrospective analysis of the National Inpatient Sample (2016–2021), identifying adults hospitalized with PUD, stratified by HIV status. Multivariable logistic regression adjusted for age, gender, race, Elixhauser comorbidity index, insurance, hospital teaching status, and bed size. Outcomes included in-hospital mortality, complications, resource utilization, and procedures.
Results: Among 200,830 patients with PUD, 835 (0.42%) were HIV+. HIV+ patients were younger (mean age: 56.3 vs. 66.2 years), predominantly male (72.5% vs. 52.1%, p< 0.001), Black (46.7% vs. 13.1%), and on Medicaid (34.1% vs. 12.7%, p< 0.001). HIV+ patients had higher rates of drug abuse (13.2% vs. 4.0%, p< 0.001), and smoking (52.1% vs. 39.5%, p< 0.001), but lower rates of hypertension (53.3% vs. 66.1%, p< 0.001) and obesity (8.4% vs. 15.7%, p< 0.001). Adjusted analyses showed significantly higher odds of in-hospital mortality (aOR: 2.34, 95% CI: 1.33–4.10, p= 0.003) and acute kidney injury requiring hemodialysis (aOR: 1.97, 95% CI: 1.18–3.27, p= 0.009) in HIV+ patients. Helicobacter pylori detection was markedly lower in HIV+ patients (aOR: 0.19, 95% CI: 0.05–0.75, p= 0.018). Adjusted costs were $35,099.28 higher (p= 0.025), and lengths of stay were 1.03 days longer (p= 0.189). Utilization of upper endoscopy and transfusion procedures were similar.
Discussion: HIV has been associated with a lower incidence of PUD due to reduced gastric acid production. Hospitalized HIV+ patients with PUD experience significantly worse outcomes with increased in-hospital mortality, higher likelihood of renal failure requiring hemodialysis, and prolonged hospital stay. The significantly lower odds of Helicobacter pylori detection suggest alternative ulcer etiologies such as medication-induced ulcers, opportunistic infections (e.g., CMV), or non-H. pylori dyspepsia, underscoring the need for tailored diagnostic strategies.
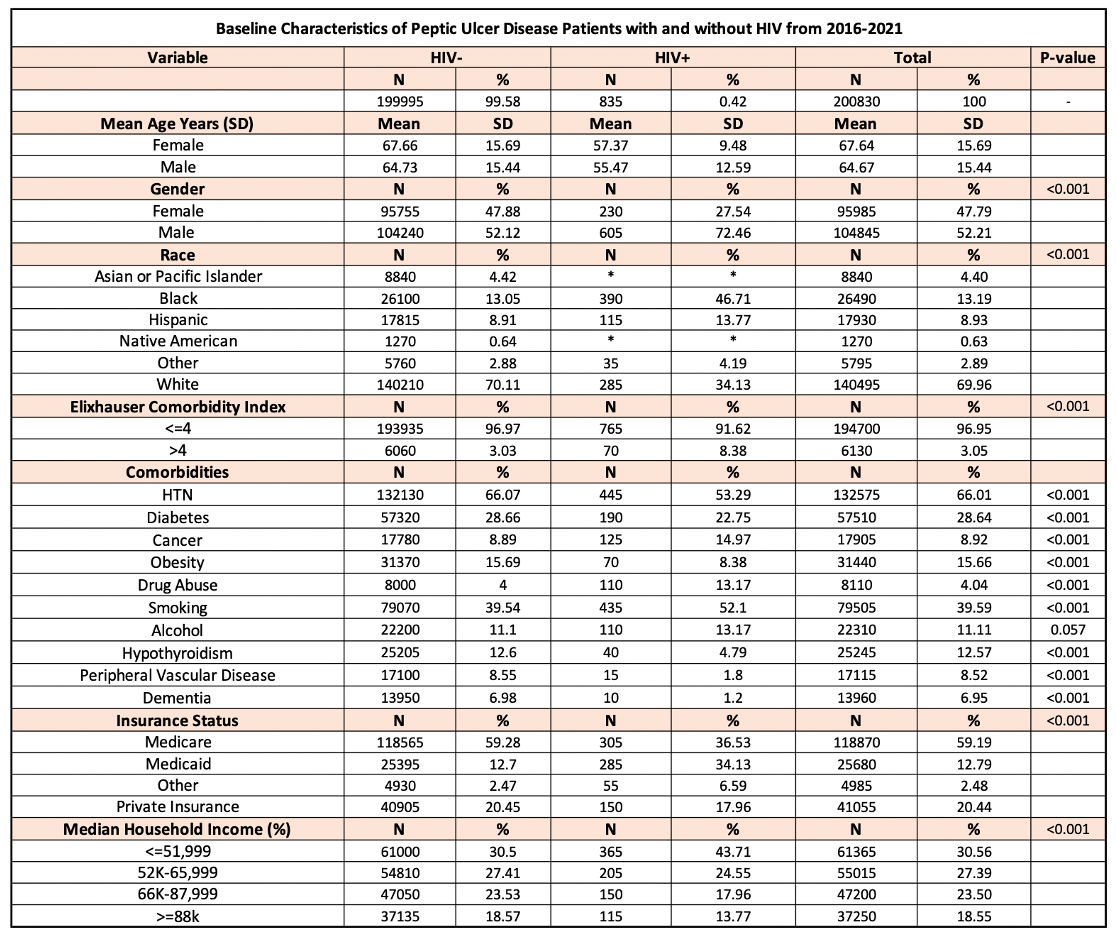
Figure: Table 1: Demographic characteristics of patients with Peptic Ulcer Disease stratified by HIV status including mean age years, gender, race, Elixhauser comorbidity index, comorbidities, insurance status and median household income.

Figure: Table 2: Inpatient outcomes in Peptic Ulcer Disease patients with HIV.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Sushrruti Varatharaj indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Abdelrahman Yousef indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Sushrruti Varatharaj, DO1, Abhishek Patel, MD1, Abdelrahman Yousef, MD2, Mohammed Quazi, PhD3, Abu Baker Sheikh, MD1. P4187 - Inpatient Outcomes of Peptic Ulcer Disease in HIV-Positive Patients in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
