Monday Poster Session
Category: Stomach and Spleen
P4186 - Emerging Disparities in Gastric Ulcer Perforation Mortality in the United States: A CDC WONDER Database Analysis (1999-2020)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Muhammad Sohaib, MD
UCHealth Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Haneen Kamran, MBBS1, Umm e Aimen Minhas, MBBS1, Juaquito Jorge, MD2, Muhammad Umer, MBBS3, Sameen Tahira, MBBS1, Muhammad Sohaib, MD4
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2Private Practice/Independent Clinical Affiliate, USA, Chicago, IL; 3Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 4UCHealth Parkview Medical Center, Pueblo, CO
Introduction: Gastric ulcer perforation is a life-threatening condition with high mortality, driven by delayed diagnosis, severe presentations, and complex surgical management. Yet national data on mortality trends remains limited, making it difficult to assess the full burden and associated disparities. Using CDC mortality data, this study examines U.S. trends and highlights high-risk populations through evaluation of demographic and geographic disparities.
Methods: Using the CDC WONDER database, deaths attributed to ulcer perforations (K25.1-.2, .5-.6; K26.1-.2, .5-.6; K27.1-.2, .5-.6; K28.1-.2, .5-.6) were extracted for adults ≥25 years for identification of early onset trends that may be masked when focusing solely on older populations. Age-adjusted mortality rates (AAMRs) per 1,000,000 were calculated using the 2000 U.S. standard population. Joinpoint regression estimated annual percent changes (APCs), with significance defined by 95% confidence intervals excluding zero. Analyses followed STROBE guidelines.
Results: Between 1999 and 2020, there were 46,730 deaths (AAMR:9.71 per 1,000,000), with an overall decline in mortality (APC=-2.64, CI:-3.45 to -1.78). Males had a higher AAMR than females (10.62 vs. 8.95). Male mortality declined markedly (APC = -6.09, CI:-6.83- -5.34) before a significant post-2010 increase (APC=1.36, CI:0.42-2.31). Female trends were more variable, with a brief non-significant period, followed by two significant declines (APC = -8.69 and -3.14), and a notable increase post-2014 (APC=3.93, CI:1.84-6.05). Patients aged 80–84 had the highest crude mortality rate (57.15). Racial disparities were pronounced: non-Hispanic (NH) Whites had the highest AAMR (9.85), followed by American Indian/Alaskan Natives (9.29) and NH Blacks (8.71); Hispanics had the lowest (5.93). Significant increases were observed among Hispanics after 2015 (APC=7.07, CI:1.27 to 13.2) with non-significant increases seen across all races. Regionally, the West had the highest AAMR (10.39), with District of Columbia and Massachusetts marking the highest (16.50) and lowest (7.91) state-level AAMRs, respectively.
Discussion: While overall mortality from ulcer perforation has declined, demographic and geographic disparities, with significant recent increases, demonstrate its growing public health burden. Given its often nonspecific presentation and rapid progression, these findings call for renewed focus on timely recognition, risk stratification, and research in high-risk groups.
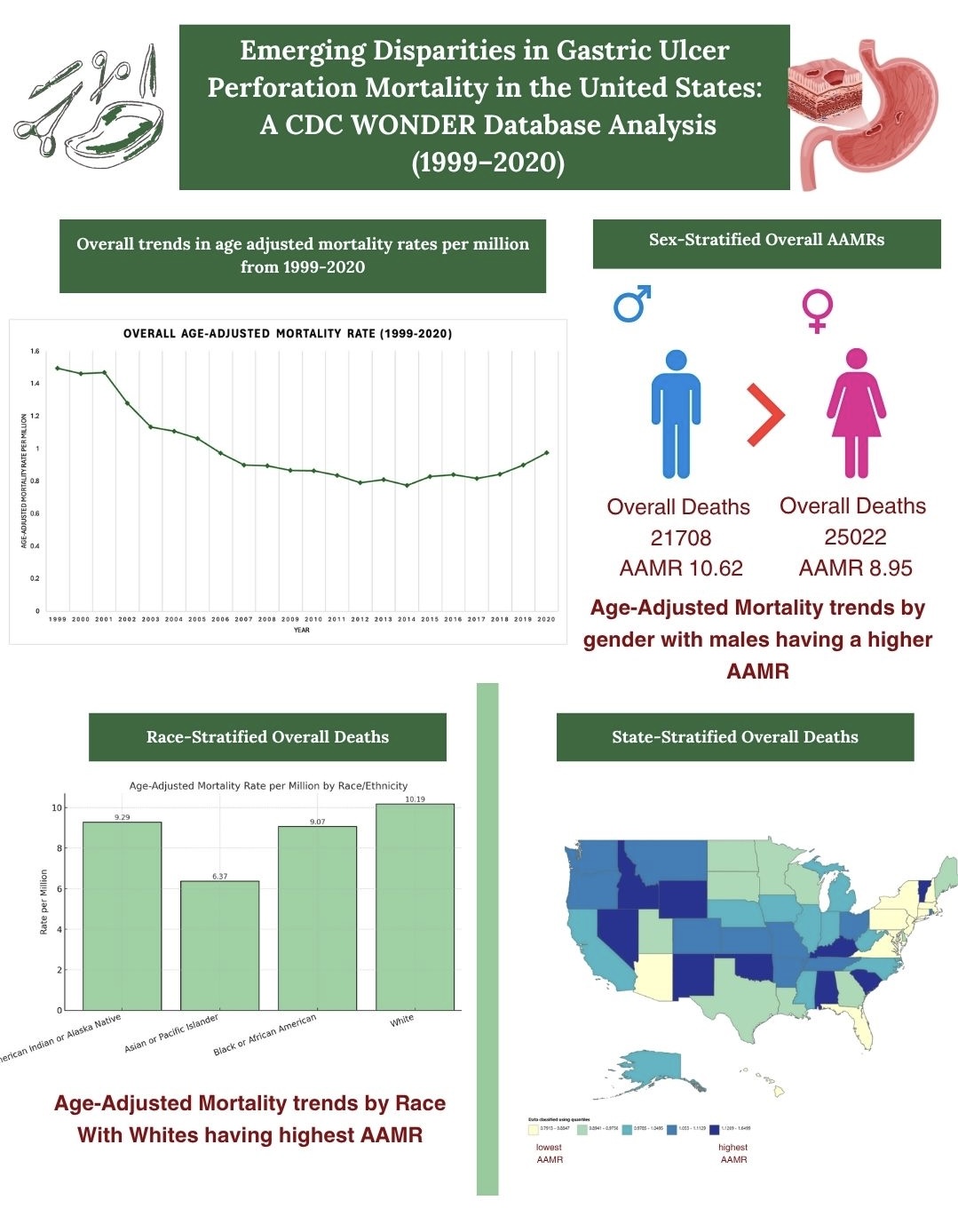
Figure: Overall trends in AAMRs per million, alongwith sex-stratified, race-stratified and state-stratified overall deaths

Figure: Joinpoint analyses of mortality trends by gender and race
Disclosures:
Haneen Kamran indicated no relevant financial relationships.
Umm e Aimen Minhas indicated no relevant financial relationships.
Juaquito Jorge indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Sameen Tahira indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Haneen Kamran, MBBS1, Umm e Aimen Minhas, MBBS1, Juaquito Jorge, MD2, Muhammad Umer, MBBS3, Sameen Tahira, MBBS1, Muhammad Sohaib, MD4. P4186 - Emerging Disparities in Gastric Ulcer Perforation Mortality in the United States: A CDC WONDER Database Analysis (1999-2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2Private Practice/Independent Clinical Affiliate, USA, Chicago, IL; 3Sahiwal Medical College, Sahiwal, Punjab, Pakistan; 4UCHealth Parkview Medical Center, Pueblo, CO
Introduction: Gastric ulcer perforation is a life-threatening condition with high mortality, driven by delayed diagnosis, severe presentations, and complex surgical management. Yet national data on mortality trends remains limited, making it difficult to assess the full burden and associated disparities. Using CDC mortality data, this study examines U.S. trends and highlights high-risk populations through evaluation of demographic and geographic disparities.
Methods: Using the CDC WONDER database, deaths attributed to ulcer perforations (K25.1-.2, .5-.6; K26.1-.2, .5-.6; K27.1-.2, .5-.6; K28.1-.2, .5-.6) were extracted for adults ≥25 years for identification of early onset trends that may be masked when focusing solely on older populations. Age-adjusted mortality rates (AAMRs) per 1,000,000 were calculated using the 2000 U.S. standard population. Joinpoint regression estimated annual percent changes (APCs), with significance defined by 95% confidence intervals excluding zero. Analyses followed STROBE guidelines.
Results: Between 1999 and 2020, there were 46,730 deaths (AAMR:9.71 per 1,000,000), with an overall decline in mortality (APC=-2.64, CI:-3.45 to -1.78). Males had a higher AAMR than females (10.62 vs. 8.95). Male mortality declined markedly (APC = -6.09, CI:-6.83- -5.34) before a significant post-2010 increase (APC=1.36, CI:0.42-2.31). Female trends were more variable, with a brief non-significant period, followed by two significant declines (APC = -8.69 and -3.14), and a notable increase post-2014 (APC=3.93, CI:1.84-6.05). Patients aged 80–84 had the highest crude mortality rate (57.15). Racial disparities were pronounced: non-Hispanic (NH) Whites had the highest AAMR (9.85), followed by American Indian/Alaskan Natives (9.29) and NH Blacks (8.71); Hispanics had the lowest (5.93). Significant increases were observed among Hispanics after 2015 (APC=7.07, CI:1.27 to 13.2) with non-significant increases seen across all races. Regionally, the West had the highest AAMR (10.39), with District of Columbia and Massachusetts marking the highest (16.50) and lowest (7.91) state-level AAMRs, respectively.
Discussion: While overall mortality from ulcer perforation has declined, demographic and geographic disparities, with significant recent increases, demonstrate its growing public health burden. Given its often nonspecific presentation and rapid progression, these findings call for renewed focus on timely recognition, risk stratification, and research in high-risk groups.
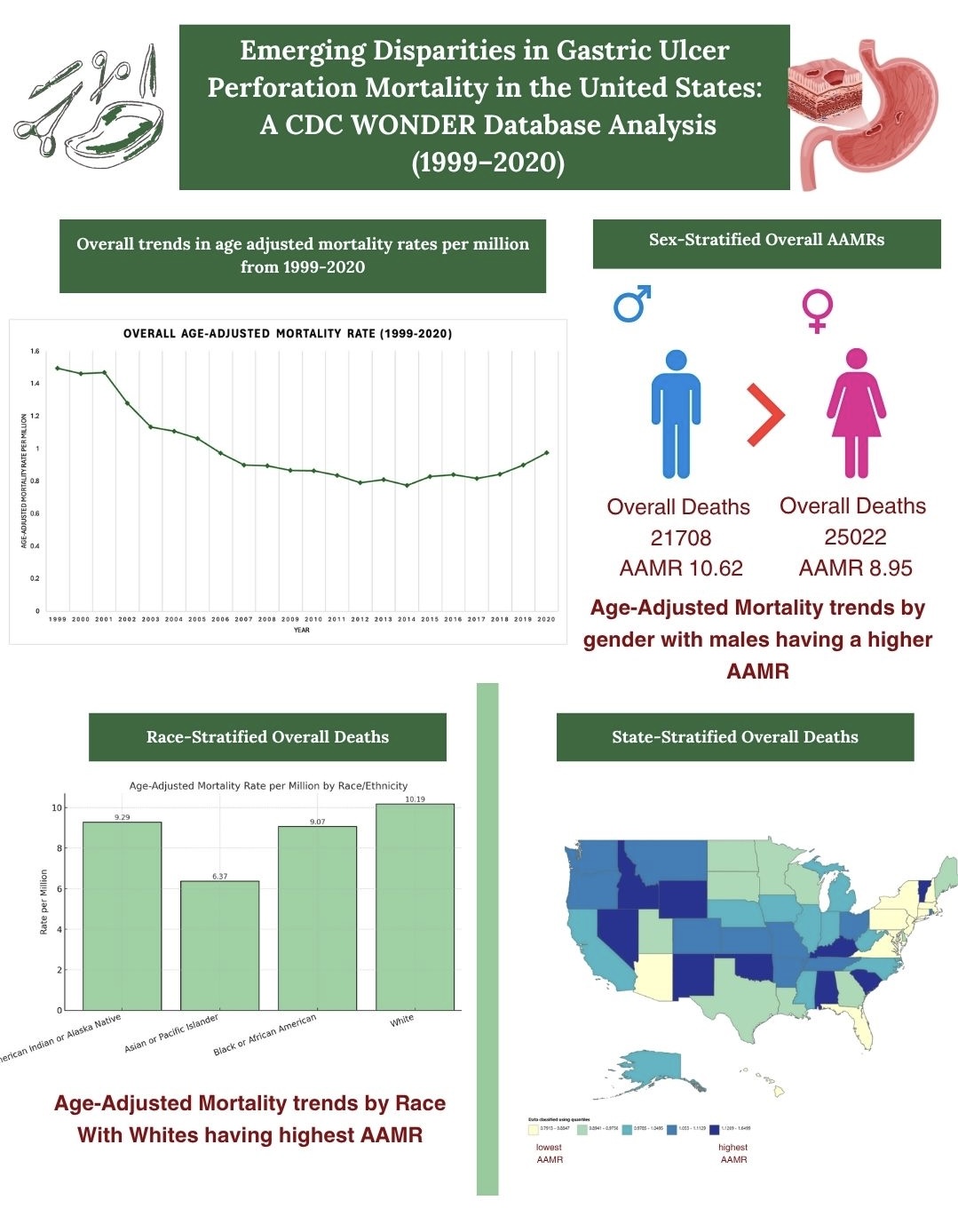
Figure: Overall trends in AAMRs per million, alongwith sex-stratified, race-stratified and state-stratified overall deaths

Figure: Joinpoint analyses of mortality trends by gender and race
Disclosures:
Haneen Kamran indicated no relevant financial relationships.
Umm e Aimen Minhas indicated no relevant financial relationships.
Juaquito Jorge indicated no relevant financial relationships.
Muhammad Umer indicated no relevant financial relationships.
Sameen Tahira indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Haneen Kamran, MBBS1, Umm e Aimen Minhas, MBBS1, Juaquito Jorge, MD2, Muhammad Umer, MBBS3, Sameen Tahira, MBBS1, Muhammad Sohaib, MD4. P4186 - Emerging Disparities in Gastric Ulcer Perforation Mortality in the United States: A CDC WONDER Database Analysis (1999-2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
