Monday Poster Session
Category: Stomach and Spleen
P4185 - Impact of Preoperative Cannabis Use on Outcomes Following Surgical Intervention for Gastroparesis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sven Eriksson, MD, MS
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Cannabis use delays gastric emptying and may exacerbate symptoms of gastroparesis. However, its impact on outcomes after surgical intervention remains poorly defined. We aimed to compare postoperative outcomes between patients with and without preoperative cannabis use.
Methods: A retrospective cohort study was conducted using TriNetX, a federated EMR database. Adults (18–89 years) with gastroparesis who underwent pyloric drainage surgery or gastric stimulator placement were stratified by the presence or absence of a cannabis-related diagnosis (ICD-10 F12) prior to surgery. Outcomes were assessed over the first 90 days and up to 5 years postoperatively. Statistical comparisons included risk analysis, Kaplan-Meier survival, and number of instances.
Results: Of 1,595 patients who underwent an intervention for gastroparesis, 108 (7.25%) had documented preoperative cannabis use. Baseline characteristics are presented in the Table. Cannabis users had higher rates of diabetes, GERD, and preoperative nausea/vomiting and abdominal pain symptoms, but similar rates of bloating. Within 90 days of surgery, cannabis users experienced higher rates of reintervention (9.3% vs 1.2%, p < 0.001) and inpatient admissions (32.4% vs 23.7%, p = 0.042), but fewer clinic visits (37.0% vs 54.5%, p < 0.001). At a mean (SD) follow-up of 1,049 (615) days, reintervention rates were similar (12.0% vs 11.3%, p = 0.808). However, cannabis users had higher hospital admission rates (59.2% vs 41.0%, p < 0.001), yet persistently lower outpatient utilization (54.6% vs 76.2%, p< 0.001) with a fewer number visits [8.0 (18) vs 12.2 (21), p=0.045) (Figure). Need for gastrectomy rates were similar (0.0% vs 0.7% p=0.989).
Discussion: Preoperative cannabis use is associated with a greater symptom burden, increased early reintervention, reduced outpatient engagement, and greater long-term healthcare utilization after surgical intervention for gastroparesis. These patients may represent a more symptomatic population and may benefit from closer follow-up to reduce readmissions.
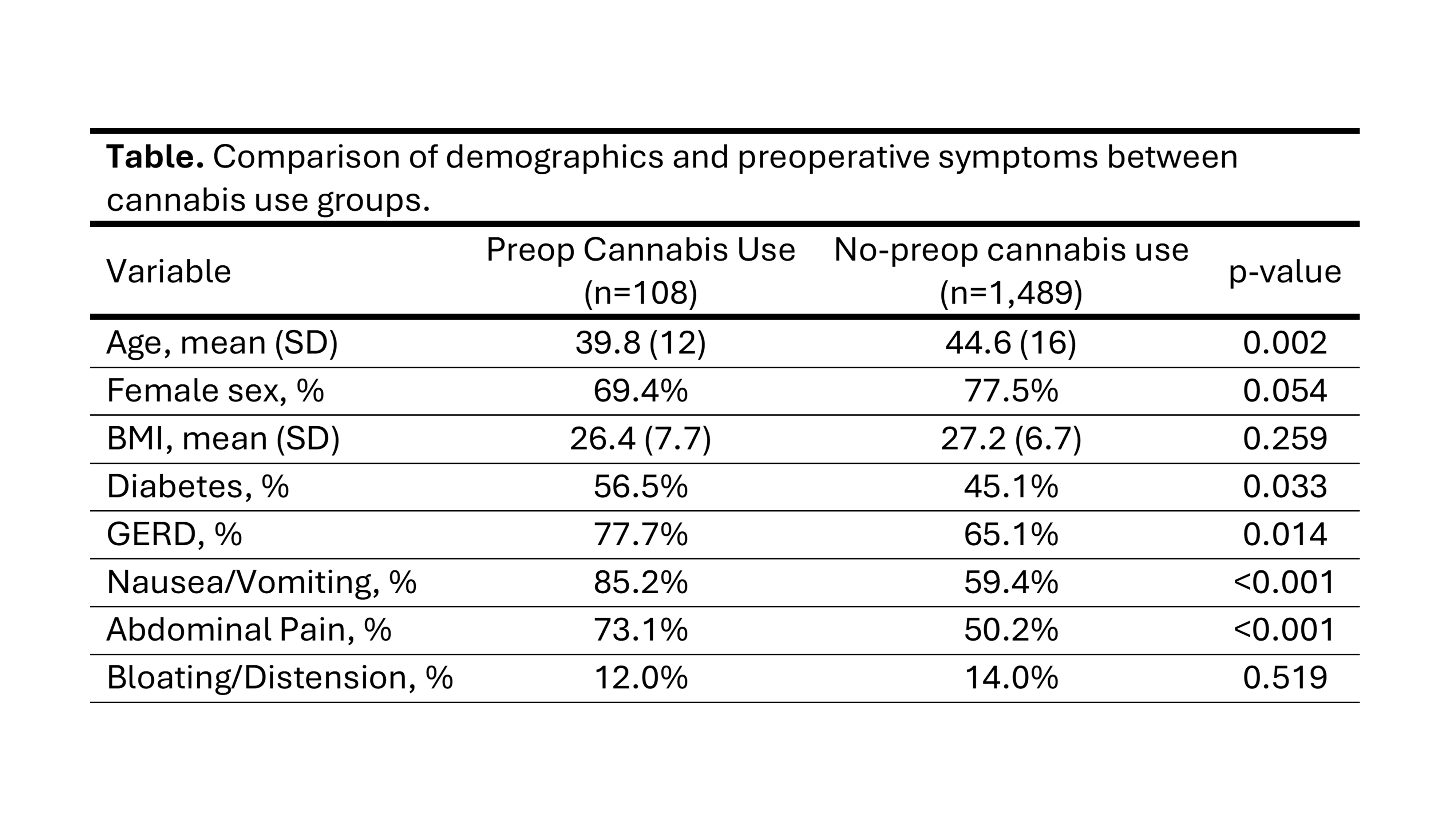
Figure: Table. Comparison of Demographics and preoperative symptoms between cannabis use groups.
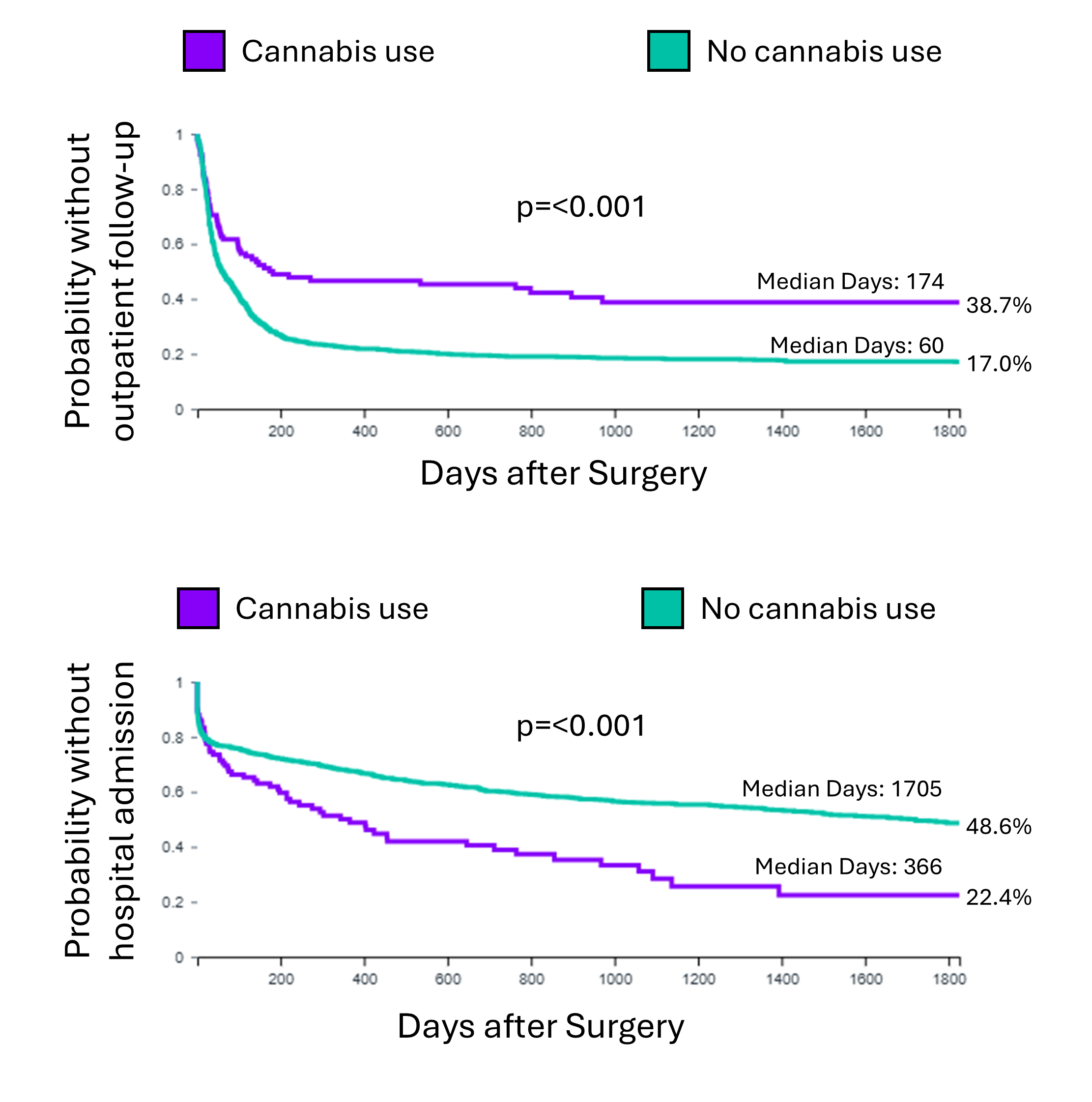
Figure: Figure. Kaplan-Meier curves showing the time to outpatient follow-up (Top) and to hospital admission (Bottom). Cannabis users were less likely to present to outpatient follow up with a significantly longer time to outpatient follow-up. However, they were more likely to require hospital admission with a shorter time to hospital admission.
Disclosures:
Sven Eriksson indicated no relevant financial relationships.
Inanc Sarici indicated no relevant financial relationships.
Ping Zheng indicated no relevant financial relationships.
Shahin Ayazi indicated no relevant financial relationships.
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2. P4185 - Impact of Preoperative Cannabis Use on Outcomes Following Surgical Intervention for Gastroparesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Cannabis use delays gastric emptying and may exacerbate symptoms of gastroparesis. However, its impact on outcomes after surgical intervention remains poorly defined. We aimed to compare postoperative outcomes between patients with and without preoperative cannabis use.
Methods: A retrospective cohort study was conducted using TriNetX, a federated EMR database. Adults (18–89 years) with gastroparesis who underwent pyloric drainage surgery or gastric stimulator placement were stratified by the presence or absence of a cannabis-related diagnosis (ICD-10 F12) prior to surgery. Outcomes were assessed over the first 90 days and up to 5 years postoperatively. Statistical comparisons included risk analysis, Kaplan-Meier survival, and number of instances.
Results: Of 1,595 patients who underwent an intervention for gastroparesis, 108 (7.25%) had documented preoperative cannabis use. Baseline characteristics are presented in the Table. Cannabis users had higher rates of diabetes, GERD, and preoperative nausea/vomiting and abdominal pain symptoms, but similar rates of bloating. Within 90 days of surgery, cannabis users experienced higher rates of reintervention (9.3% vs 1.2%, p < 0.001) and inpatient admissions (32.4% vs 23.7%, p = 0.042), but fewer clinic visits (37.0% vs 54.5%, p < 0.001). At a mean (SD) follow-up of 1,049 (615) days, reintervention rates were similar (12.0% vs 11.3%, p = 0.808). However, cannabis users had higher hospital admission rates (59.2% vs 41.0%, p < 0.001), yet persistently lower outpatient utilization (54.6% vs 76.2%, p< 0.001) with a fewer number visits [8.0 (18) vs 12.2 (21), p=0.045) (Figure). Need for gastrectomy rates were similar (0.0% vs 0.7% p=0.989).
Discussion: Preoperative cannabis use is associated with a greater symptom burden, increased early reintervention, reduced outpatient engagement, and greater long-term healthcare utilization after surgical intervention for gastroparesis. These patients may represent a more symptomatic population and may benefit from closer follow-up to reduce readmissions.
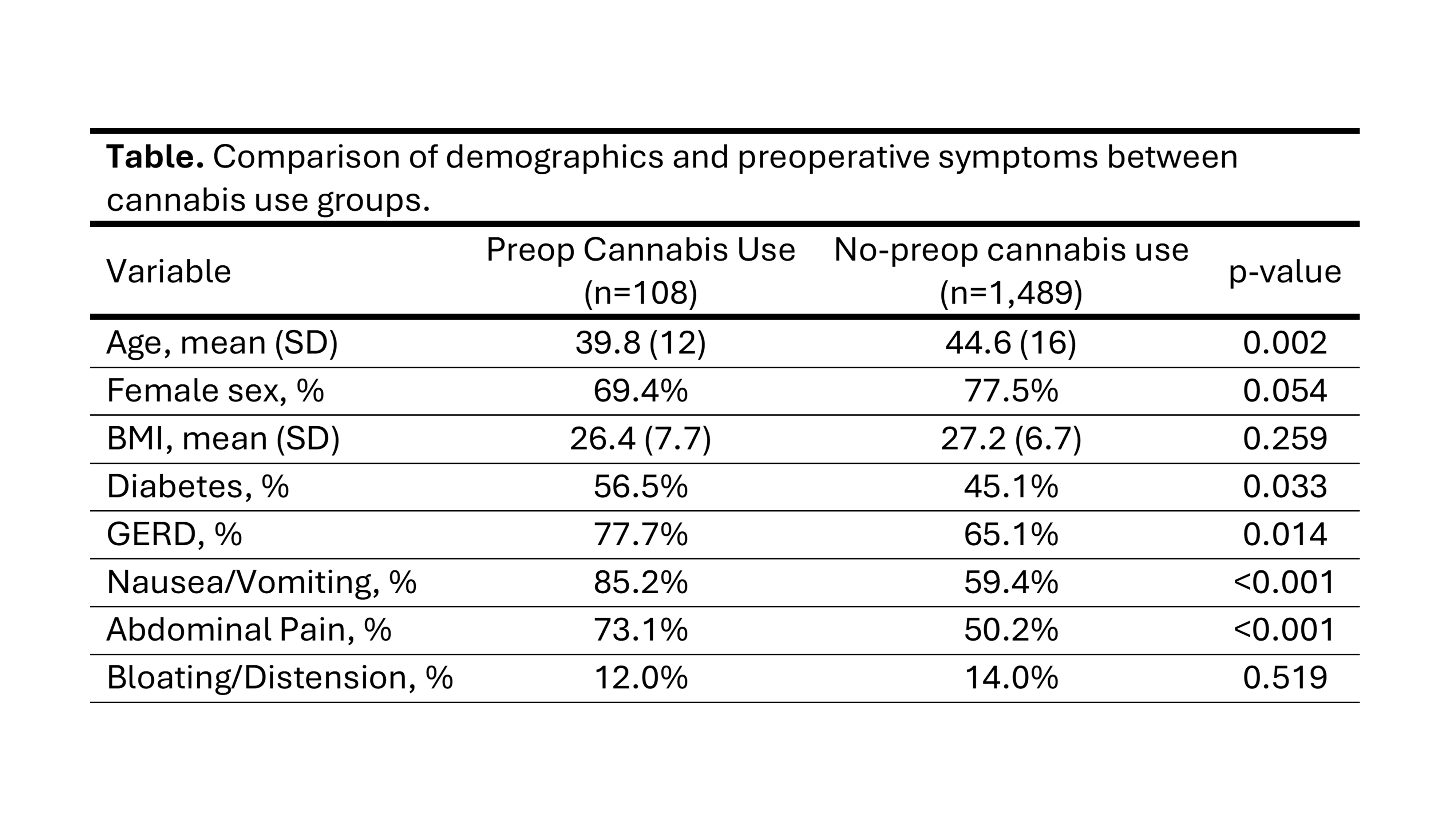
Figure: Table. Comparison of Demographics and preoperative symptoms between cannabis use groups.
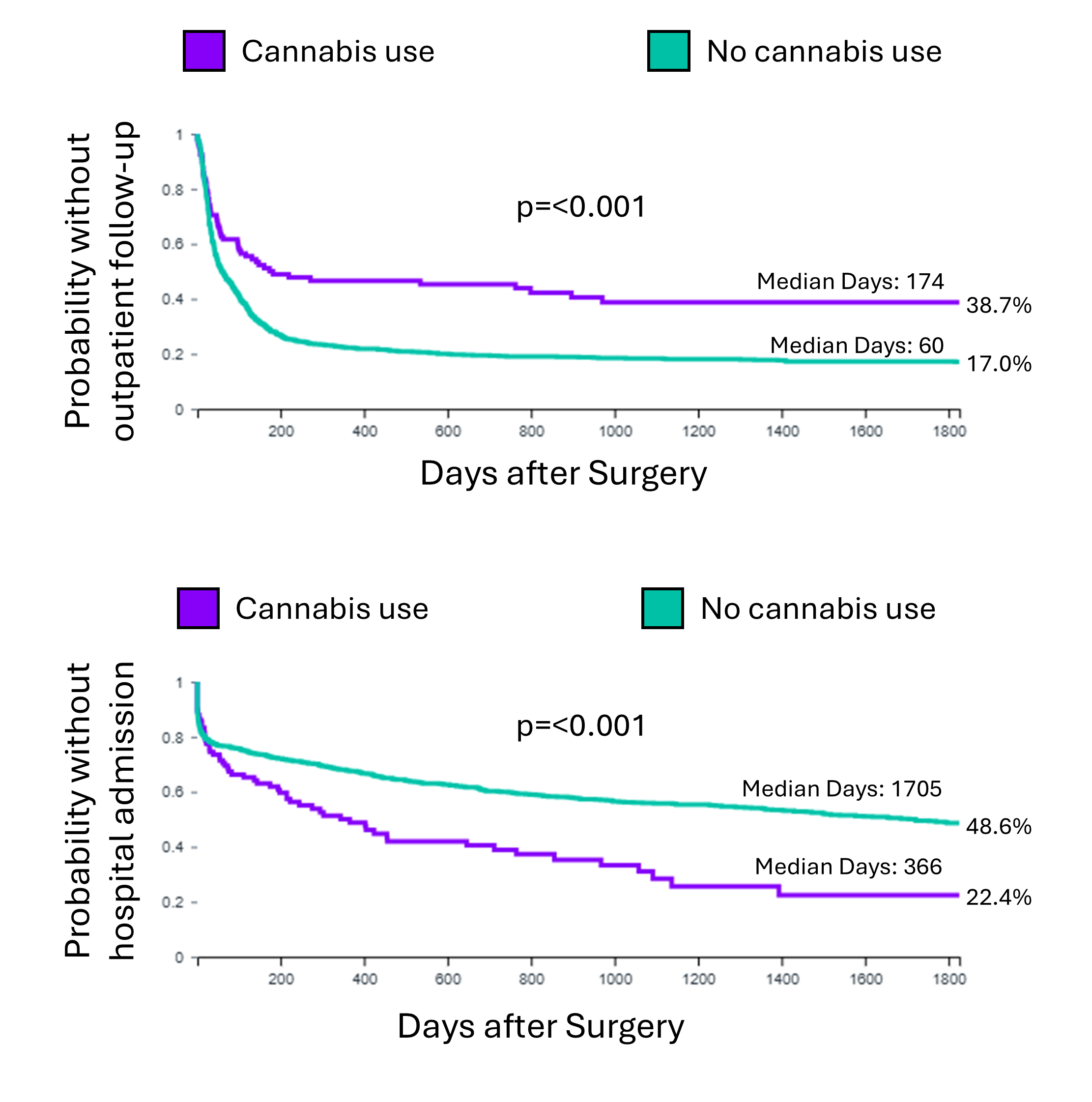
Figure: Figure. Kaplan-Meier curves showing the time to outpatient follow-up (Top) and to hospital admission (Bottom). Cannabis users were less likely to present to outpatient follow up with a significantly longer time to outpatient follow-up. However, they were more likely to require hospital admission with a shorter time to hospital admission.
Disclosures:
Sven Eriksson indicated no relevant financial relationships.
Inanc Sarici indicated no relevant financial relationships.
Ping Zheng indicated no relevant financial relationships.
Shahin Ayazi indicated no relevant financial relationships.
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2. P4185 - Impact of Preoperative Cannabis Use on Outcomes Following Surgical Intervention for Gastroparesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
