Monday Poster Session
Category: Stomach and Spleen
P4182 - Long-Term Metabolic Outcomes of Endoscopic Sleeve Gastroplasty in Patients With Type 2 Diabetes: A Systematic Review
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AN
Alexandra Nieto Dominguez (she/her/hers)
Universidad Latina de Panamá
Panamá, Panama, Panama
Presenting Author(s)
Alejandro Nieto Dominguez, MD1, Alexandra Nieto Dominguez, 2, Adriana Guevara Arrocha, 2, Patricia Zarza Gulino, MD3, Jose Nieto, 4, Maria Grba, MD3, Saksham Kohli, MBBS3
1Cook County Health and Hospital Systems, Chicago, IL; 2Universidad Latina de Panamá, Panamá, Panama, Panama; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Universidad Latina de Panama, Panama City, Panama, Panama
Introduction: Endoscopic sleeve gastroplasty (ESG) is a minimally invasive procedure that reduces gastric volume by ~70% using endoscopic suturing. It has shown short-term metabolic benefits in patients with obesity and type 2 diabetes mellitus (T2DM), including improved glycemia, weight, blood pressure, liver enzymes, and lipid profiles. However, most data are limited to 6–24 months, and the long-term durability of these effects in T2DM remains unclear. The objective of this study is to determine the sustained impact of ESG on metabolic outcomes thereby contributing to a more complete understanding of ESG’s long-term role in the management of T2DM.
Methods: We conducted a systematic review following PRISMA guidelines, searching PubMed, Embase, and Scopus from inception through March 2025. Inclusion criteria were prospective or retrospective studies reporting ≥3-year outcomes after ESG in adults with T2DM. We excluded studies involving non-adult populations, non-ESG bariatric therapies, follow-up < 36 months, absence of extractable T2DM metabolic data, case series < 10 patients, reviews or duplicates, and non-English papers without accessible full text.
Primary outcomes included changes in glycemic control, diabetes remission rates, and total body weight loss (TBWL). Risk of bias was assessed using the Newcastle–Ottawa Scale.
Results: Out of 161 records identified, 118 unique studies were screened after deduplication. 3 studies met inclusion criteria, with follow-up durations of 4 to 5 years and T2DM subgroups ranging from 14% to 44% of each cohort. Diabetes remission or improvement ranged from 51.2% to 66.7%. Only one study reported granular metabolic data, including a 0.42% absolute HbA1c reduction and improvement in insulin resistance (HOMA-IR). TBWL at 5 years ranged from 11.8% to 12.2% in two studies; a third reported 18.2% TBWL at 4 years. Risk of bias was low in one study and moderate in the other two.
Discussion: Our study demonstrates that endoscopic sleeve gastroplasty (ESG) is associated with sustained improvements in glycemic control, insulin resistance, and weight loss in patients with type 2 diabetes mellitus. Despite the limited number of long-term studies, available evidence indicates that the metabolic benefits of ESG can be maintained over time.
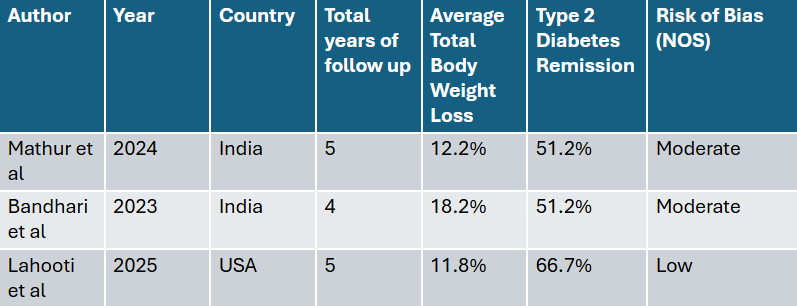
Figure: Summary of Included Studies and Main Results.
Disclosures:
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Alexandra Nieto Dominguez indicated no relevant financial relationships.
Adriana Guevara Arrocha indicated no relevant financial relationships.
Patricia Zarza Gulino indicated no relevant financial relationships.
Jose Nieto indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Alejandro Nieto Dominguez, MD1, Alexandra Nieto Dominguez, 2, Adriana Guevara Arrocha, 2, Patricia Zarza Gulino, MD3, Jose Nieto, 4, Maria Grba, MD3, Saksham Kohli, MBBS3. P4182 - Long-Term Metabolic Outcomes of Endoscopic Sleeve Gastroplasty in Patients With Type 2 Diabetes: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health and Hospital Systems, Chicago, IL; 2Universidad Latina de Panamá, Panamá, Panama, Panama; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Universidad Latina de Panama, Panama City, Panama, Panama
Introduction: Endoscopic sleeve gastroplasty (ESG) is a minimally invasive procedure that reduces gastric volume by ~70% using endoscopic suturing. It has shown short-term metabolic benefits in patients with obesity and type 2 diabetes mellitus (T2DM), including improved glycemia, weight, blood pressure, liver enzymes, and lipid profiles. However, most data are limited to 6–24 months, and the long-term durability of these effects in T2DM remains unclear. The objective of this study is to determine the sustained impact of ESG on metabolic outcomes thereby contributing to a more complete understanding of ESG’s long-term role in the management of T2DM.
Methods: We conducted a systematic review following PRISMA guidelines, searching PubMed, Embase, and Scopus from inception through March 2025. Inclusion criteria were prospective or retrospective studies reporting ≥3-year outcomes after ESG in adults with T2DM. We excluded studies involving non-adult populations, non-ESG bariatric therapies, follow-up < 36 months, absence of extractable T2DM metabolic data, case series < 10 patients, reviews or duplicates, and non-English papers without accessible full text.
Primary outcomes included changes in glycemic control, diabetes remission rates, and total body weight loss (TBWL). Risk of bias was assessed using the Newcastle–Ottawa Scale.
Results: Out of 161 records identified, 118 unique studies were screened after deduplication. 3 studies met inclusion criteria, with follow-up durations of 4 to 5 years and T2DM subgroups ranging from 14% to 44% of each cohort. Diabetes remission or improvement ranged from 51.2% to 66.7%. Only one study reported granular metabolic data, including a 0.42% absolute HbA1c reduction and improvement in insulin resistance (HOMA-IR). TBWL at 5 years ranged from 11.8% to 12.2% in two studies; a third reported 18.2% TBWL at 4 years. Risk of bias was low in one study and moderate in the other two.
Discussion: Our study demonstrates that endoscopic sleeve gastroplasty (ESG) is associated with sustained improvements in glycemic control, insulin resistance, and weight loss in patients with type 2 diabetes mellitus. Despite the limited number of long-term studies, available evidence indicates that the metabolic benefits of ESG can be maintained over time.
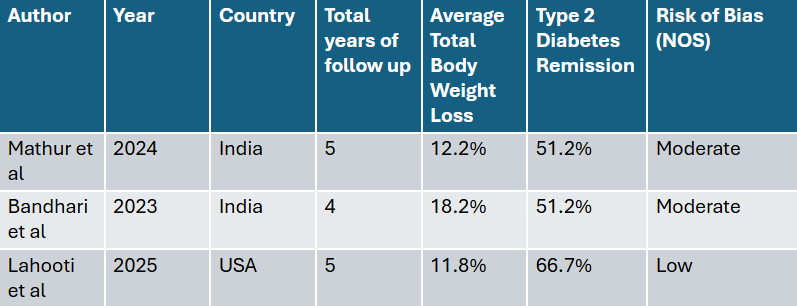
Figure: Summary of Included Studies and Main Results.
Disclosures:
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Alexandra Nieto Dominguez indicated no relevant financial relationships.
Adriana Guevara Arrocha indicated no relevant financial relationships.
Patricia Zarza Gulino indicated no relevant financial relationships.
Jose Nieto indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Alejandro Nieto Dominguez, MD1, Alexandra Nieto Dominguez, 2, Adriana Guevara Arrocha, 2, Patricia Zarza Gulino, MD3, Jose Nieto, 4, Maria Grba, MD3, Saksham Kohli, MBBS3. P4182 - Long-Term Metabolic Outcomes of Endoscopic Sleeve Gastroplasty in Patients With Type 2 Diabetes: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
