Monday Poster Session
Category: Stomach and Spleen
P4176 - Endoscopic Recognition of Gastric Intestinal Metaplasia: How Well Are We Doing?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- UB
Umesh Bhagat, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Umesh Bhagat, MD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Pepper Pike, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Gastric intestinal metaplasia (GIM) is a prevalent precancerous change of the gastric mucosa and a step in the Correa cascade leading to gastric cancer. Although GIM has distinct endoscopic features, it is often diagnosed incidentally in the United States (US). One study evaluated EGD findings in patients with incidental GIM before 2016, but no studies have assessed GIM endoscopic recognition and mucosa description since the first US GIM surveillance guideline released in 2020. We evaluate endoscopists’ endoscopic description of the gastric mucosal in patients with biopsy-proven GIM.
Methods: In this retrospective cohort study, we included a cohort of adult patients who underwent EGD with gastric biopsies and who had GIM reported in the pathology report between 2022 and 2023 at out tertiary care center. Demographic, clinical, endoscopic and pathology characteristics were collected. Patients were stratified into high- and low-risk groups based on EGD indication. High-risk patients were defined as those undergoing EGD for GIM or gastric dysplasia surveillance, history of autoimmune gastritis, pernicious anemia or PTEN mutation. Sydney protocol was defined as biopsies taken from the corpus and antrum. Chi-square test was used to compare categorical variables. P-value< 0.05 was considered statistically significant.
Results: 81 patients were included and mean age was 66.7 ± 13.41 years. 61.7% were female, 70.4% White and 81.5% non-Hispanic. 88.5% of patients had proton pump inhibitors on their medication list at time of EGD. The most common EGD indications were GERD (30%) and abdominal pain (26.5%). Gastric biopsies were taken per Sydney protocol in 50.6% of patients and Helicobacter pylori infection was detected in 11.1%. Among gastric areas harboring GIM on pathology, erythema was the most common endoscopic description in 41.8% of patients, followed by erosion (20.3%), atrophy (18.1%), normal (15.2%) and nodular mucosa (12.7%). There was no difference in the endoscopic description of gastric mucosa harboring GIM in high vs. low-risk patients (Table2).
Discussion: Endoscopic descriptions of the gastric mucosa in patients with GIM remain variable and often non-specific, even among those with known GIM, AIG, or dysplasia. Larger studies are needed to validate these findings. Developing training modules and endoscopic image libraries may help improve the endoscopic detection of GIM and other precancerous lesions.
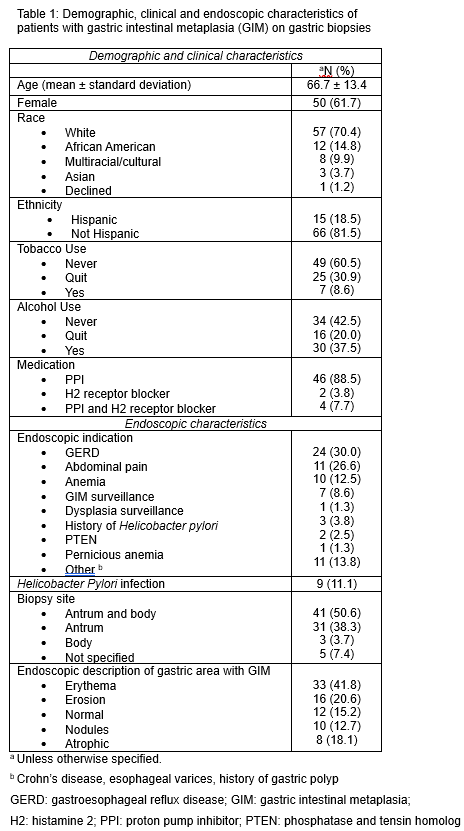
Figure: Demographic and clinical characteristics
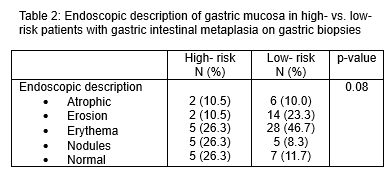
Figure: Endoscopic description of mucosa
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Kyungran Justina Cho indicated no relevant financial relationships.
Michelle Kang Kim indicated no relevant financial relationships.
Carol Rouphael indicated no relevant financial relationships.
Umesh Bhagat, MD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3. P4176 - Endoscopic Recognition of Gastric Intestinal Metaplasia: How Well Are We Doing?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Pepper Pike, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Gastric intestinal metaplasia (GIM) is a prevalent precancerous change of the gastric mucosa and a step in the Correa cascade leading to gastric cancer. Although GIM has distinct endoscopic features, it is often diagnosed incidentally in the United States (US). One study evaluated EGD findings in patients with incidental GIM before 2016, but no studies have assessed GIM endoscopic recognition and mucosa description since the first US GIM surveillance guideline released in 2020. We evaluate endoscopists’ endoscopic description of the gastric mucosal in patients with biopsy-proven GIM.
Methods: In this retrospective cohort study, we included a cohort of adult patients who underwent EGD with gastric biopsies and who had GIM reported in the pathology report between 2022 and 2023 at out tertiary care center. Demographic, clinical, endoscopic and pathology characteristics were collected. Patients were stratified into high- and low-risk groups based on EGD indication. High-risk patients were defined as those undergoing EGD for GIM or gastric dysplasia surveillance, history of autoimmune gastritis, pernicious anemia or PTEN mutation. Sydney protocol was defined as biopsies taken from the corpus and antrum. Chi-square test was used to compare categorical variables. P-value< 0.05 was considered statistically significant.
Results: 81 patients were included and mean age was 66.7 ± 13.41 years. 61.7% were female, 70.4% White and 81.5% non-Hispanic. 88.5% of patients had proton pump inhibitors on their medication list at time of EGD. The most common EGD indications were GERD (30%) and abdominal pain (26.5%). Gastric biopsies were taken per Sydney protocol in 50.6% of patients and Helicobacter pylori infection was detected in 11.1%. Among gastric areas harboring GIM on pathology, erythema was the most common endoscopic description in 41.8% of patients, followed by erosion (20.3%), atrophy (18.1%), normal (15.2%) and nodular mucosa (12.7%). There was no difference in the endoscopic description of gastric mucosa harboring GIM in high vs. low-risk patients (Table2).
Discussion: Endoscopic descriptions of the gastric mucosa in patients with GIM remain variable and often non-specific, even among those with known GIM, AIG, or dysplasia. Larger studies are needed to validate these findings. Developing training modules and endoscopic image libraries may help improve the endoscopic detection of GIM and other precancerous lesions.
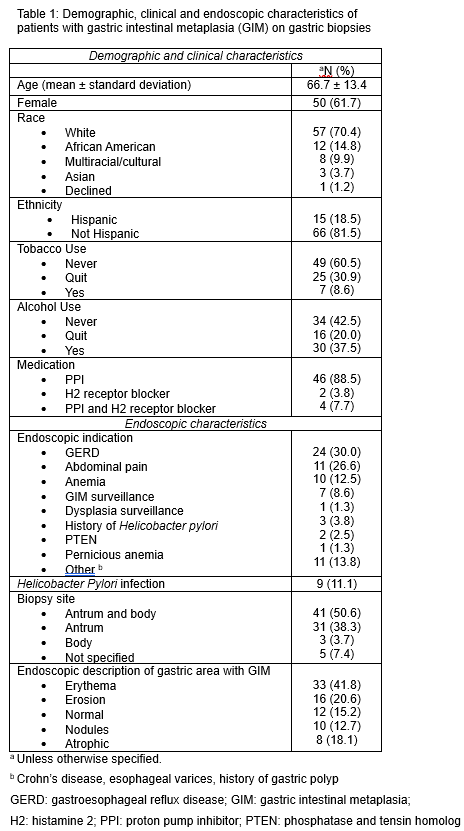
Figure: Demographic and clinical characteristics
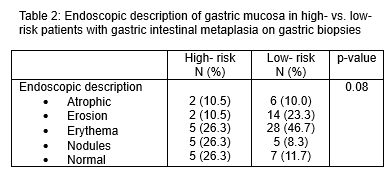
Figure: Endoscopic description of mucosa
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Kyungran Justina Cho indicated no relevant financial relationships.
Michelle Kang Kim indicated no relevant financial relationships.
Carol Rouphael indicated no relevant financial relationships.
Umesh Bhagat, MD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3. P4176 - Endoscopic Recognition of Gastric Intestinal Metaplasia: How Well Are We Doing?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
