Monday Poster Session
Category: Stomach and Spleen
P4175 - Frailty Scoring in Diabetic vs Non-Diabetic Gastroparesis Patients
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manasa Devi Vallabhaneni, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Manasa Devi. Vallabhaneni, MD, Ali Makhdoom, MD, Reena Anand, MBBS, Rona Cooper, MS, Henry P.. Parkman, MD, FACG
Temple University Hospital, Philadelphia, PA
Introduction: Gastroparesis (Gp) is commonly categorized into idiopathic, diabetic, and postsurgical subtypes. Idiopathic cases account for up to two-thirds of presentations. Other causes include diabetic neuropathy, post-vagotomy, and Parkinson’s disease. Regardless of cause, symptoms tend to be similar and negatively impact quality of life. In a prior study that was completed, gastroparesis patients were found to have increased frailty across various clinical frailty scales. This study is a subgroup analysis comparing frailty and symptom burden between patients with diabetic and non-diabetic gastroparesis.
Methods: Patients with gastroparesis completed several assessments: Patient Assessment of Upper Gastrointestinal Disorders-Symptom Severity Index (PAG-SYMI), SF-8 quality of life scale, FRAIL score, Clinical Frailty Scale-8 (CFS-8), Canadian Study of Health and Aging (CSHA) frailty scale, and Edmonton Frailty Scale. The PAG-SYMI (0–5) evaluates GI symptom severity, with higher scores indicating worse symptoms. CFS-8 and FRAIL assess emotional and physical frailty, respectively. The CSHA (1–6) and Edmonton (0–10+) scores measure functional fitness and multidimensional frailty. Handgrip strength was measured using a Jamar dynamometer.
Results: A total of 73 gastroparesis patients were included: 14 with diabetes and 59 without. No statistically significant differences were found between groups across clinical and functional measures. PAG-SYMI scores were similar (diabetic: 2.61 ± 1.04; non-diabetic: 2.55 ± 1.13; p = 0.42), as were SF-8 scores (2.06 ± 0.87 vs. 2.03 ± 0.88; p = 0.46). Frailty assessments showed no significant differences: FRAIL (1.79 ± 0.97 vs. 1.55 ± 1.14; p = 0.34), CSHA (3.21 ± 1.42 vs. 3.16 ± 1.33; p = 0.42), and Edmonton (5.00 ± 3.28 vs. 4.15 ± 2.79; p = 0.20). Diabetic patients had slightly lower handgrip strength (23.50 ± 8.93 kg vs. 26.73 ± 8.12 kg; p = 0.14), though this difference was not significant.
Discussion: Patients with diabetic and non-diabetic gastroparesis demonstrated similar levels of symptom severity, quality of life impairment, and frailty. Although diabetic patients had marginally lower physical strength and higher frailty scores, these differences were not statistically significant. These findings suggest that gastroparesis imposes a comparable clinical burden regardless of underlying etiology. Larger studies are needed to determine whether specific subgroups may benefit from tailored interventions.
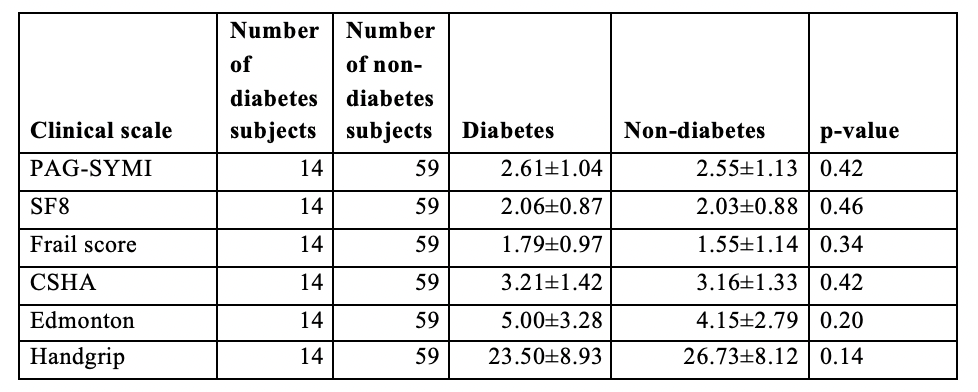
Figure: Averages and standard deviations for clinical scales between diabetic and non-diabetic gastroparesis subjects
Disclosures:
Manasa Vallabhaneni indicated no relevant financial relationships.
Ali Makhdoom indicated no relevant financial relationships.
Reena Anand indicated no relevant financial relationships.
Rona Cooper indicated no relevant financial relationships.
Henry Parkman indicated no relevant financial relationships.
Manasa Devi. Vallabhaneni, MD, Ali Makhdoom, MD, Reena Anand, MBBS, Rona Cooper, MS, Henry P.. Parkman, MD, FACG. P4175 - Frailty Scoring in Diabetic vs Non-Diabetic Gastroparesis Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Temple University Hospital, Philadelphia, PA
Introduction: Gastroparesis (Gp) is commonly categorized into idiopathic, diabetic, and postsurgical subtypes. Idiopathic cases account for up to two-thirds of presentations. Other causes include diabetic neuropathy, post-vagotomy, and Parkinson’s disease. Regardless of cause, symptoms tend to be similar and negatively impact quality of life. In a prior study that was completed, gastroparesis patients were found to have increased frailty across various clinical frailty scales. This study is a subgroup analysis comparing frailty and symptom burden between patients with diabetic and non-diabetic gastroparesis.
Methods: Patients with gastroparesis completed several assessments: Patient Assessment of Upper Gastrointestinal Disorders-Symptom Severity Index (PAG-SYMI), SF-8 quality of life scale, FRAIL score, Clinical Frailty Scale-8 (CFS-8), Canadian Study of Health and Aging (CSHA) frailty scale, and Edmonton Frailty Scale. The PAG-SYMI (0–5) evaluates GI symptom severity, with higher scores indicating worse symptoms. CFS-8 and FRAIL assess emotional and physical frailty, respectively. The CSHA (1–6) and Edmonton (0–10+) scores measure functional fitness and multidimensional frailty. Handgrip strength was measured using a Jamar dynamometer.
Results: A total of 73 gastroparesis patients were included: 14 with diabetes and 59 without. No statistically significant differences were found between groups across clinical and functional measures. PAG-SYMI scores were similar (diabetic: 2.61 ± 1.04; non-diabetic: 2.55 ± 1.13; p = 0.42), as were SF-8 scores (2.06 ± 0.87 vs. 2.03 ± 0.88; p = 0.46). Frailty assessments showed no significant differences: FRAIL (1.79 ± 0.97 vs. 1.55 ± 1.14; p = 0.34), CSHA (3.21 ± 1.42 vs. 3.16 ± 1.33; p = 0.42), and Edmonton (5.00 ± 3.28 vs. 4.15 ± 2.79; p = 0.20). Diabetic patients had slightly lower handgrip strength (23.50 ± 8.93 kg vs. 26.73 ± 8.12 kg; p = 0.14), though this difference was not significant.
Discussion: Patients with diabetic and non-diabetic gastroparesis demonstrated similar levels of symptom severity, quality of life impairment, and frailty. Although diabetic patients had marginally lower physical strength and higher frailty scores, these differences were not statistically significant. These findings suggest that gastroparesis imposes a comparable clinical burden regardless of underlying etiology. Larger studies are needed to determine whether specific subgroups may benefit from tailored interventions.
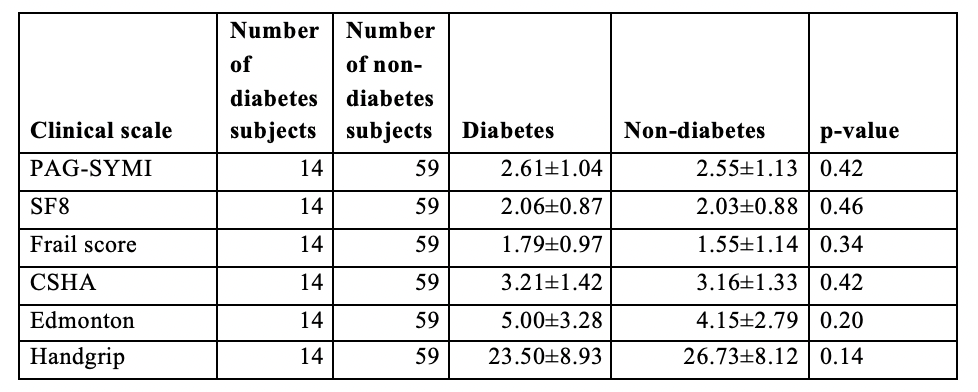
Figure: Averages and standard deviations for clinical scales between diabetic and non-diabetic gastroparesis subjects
Disclosures:
Manasa Vallabhaneni indicated no relevant financial relationships.
Ali Makhdoom indicated no relevant financial relationships.
Reena Anand indicated no relevant financial relationships.
Rona Cooper indicated no relevant financial relationships.
Henry Parkman indicated no relevant financial relationships.
Manasa Devi. Vallabhaneni, MD, Ali Makhdoom, MD, Reena Anand, MBBS, Rona Cooper, MS, Henry P.. Parkman, MD, FACG. P4175 - Frailty Scoring in Diabetic vs Non-Diabetic Gastroparesis Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
