Monday Poster Session
Category: Small Intestine
P4147 - When Purpura Meets Hematemesis: A Rare Adult Onset Presentation of IgA Vasculitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rameesha Zubair, MBBS (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rameesha Zubair, MBBS1, Karmen Brar, MD1, Abdul Khuram, DO1, Akaash Mittal, MD1, Thomas Corredine, DO2
1University of Connecticut Health, Farmington, CT; 2Saint Francis Hospital, Trinity Health of New England, Hartford, CT
Introduction: Immunoglobulin A (IgA) vasculitis, formerly known as Henoch–Shönlein purpura, is a small vessel vasculitis defined by IgA1-dominant immune complex deposition. It classically presents as a tetrad of palpable purpura, arthralgias, renal involvement, and gastrointestinal (GI) symptoms. While GI manifestations are more commonly recognized in pediatric populations, they are often underdiagnosed in adults. Here, we present a unique cause of adult-onset IgA vasculitis with prominent GI involvement.
Case Description/
Methods: A 35-year-old male with a history of obesity, hypertension and hyperlipidemia presented with chest pain and a purpuric rash on his lower abdomen extending to his extremities. Initially diagnosed with contact dermatitis, he was discharged on systemic and topical steroids. However, he returned two days later with hematemesis, hematochezia, and abdominal pain. Exam revealed a distended, non-tender abdomen with diffuse palpable purpura and bilateral lower extremity edema. CT abdomen/pelvis showed severe jejunal thickening, moderate small bowel wall edema and right-sided colitis. Skin biopsies were obtained and he was treated with systemic steroids and PPIs. Despite initial stabilization, he developed increasing abdominal distention. Repeat imaging showed worsening enteritis and ileus versus a partial small bowel obstruction with moderate-large ascites. Once bowel ischemia and obstruction were ruled out, the patient’s condition normalized with steroids and supportive care. Skin biopsies ultimately confirmed IgA vasculitis with superficial perivascular IgA and C3 deposition, and he was discharged on a steroid taper with ongoing symptom resolution during outpatient follow-up.
Discussion: GI involvement in IgA vasculitis is typically seen with pediatric patients but can occur in adults and may present with significant morbidity. Symptoms typically include abdominal pain, GI bleeding, vomiting and diarrhea. Imaging findings often reveal duodenitis, jejunitis, and ileitis. Although not required, endoscopic biopsy can reveal vasculitis changes such as leukocytoclastic vasculitis and lamina propria hemorrhage even without active symptoms. Severe complications include intussusception, bowel perforation and gallbladder hydrops. Treatment is usually supportive but systemic corticosteroids are often used for severe cases. Immunosuppressants such as mycophenolate or rituximab can be considered for refractory cases. Further studies should be directed at exploring GI manifestations of IgA vasculitis.
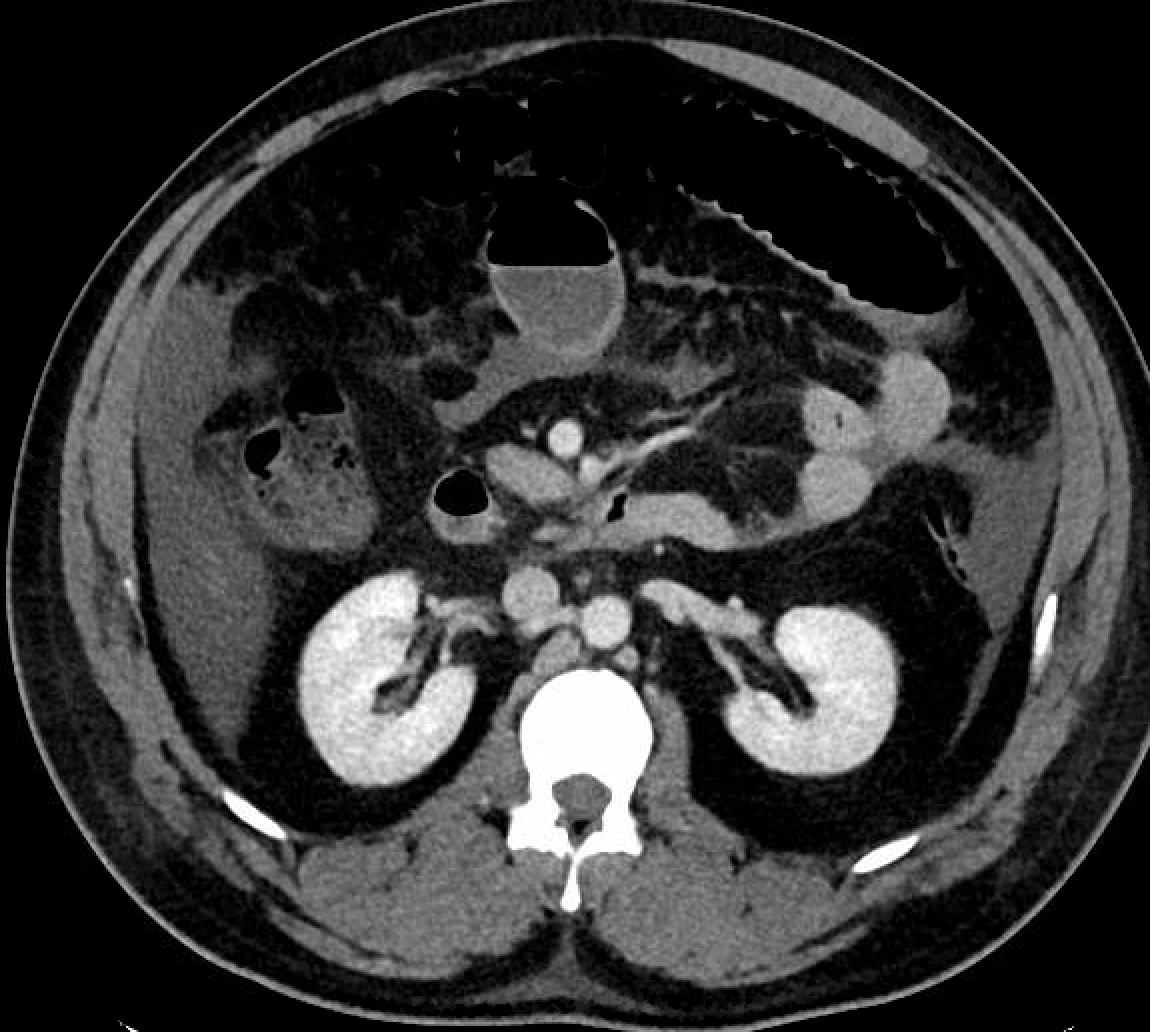
Figure: Figure 1: Worsening small bowel enteritis appreciated on CT abdomen & pelvis

Figure: Figure 2: Abdominal rash consistent with IgA vasculitis
Disclosures:
Rameesha Zubair indicated no relevant financial relationships.
Karmen Brar indicated no relevant financial relationships.
Abdul Khuram indicated no relevant financial relationships.
Akaash Mittal indicated no relevant financial relationships.
Thomas Corredine indicated no relevant financial relationships.
Rameesha Zubair, MBBS1, Karmen Brar, MD1, Abdul Khuram, DO1, Akaash Mittal, MD1, Thomas Corredine, DO2. P4147 - When Purpura Meets Hematemesis: A Rare Adult Onset Presentation of IgA Vasculitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2Saint Francis Hospital, Trinity Health of New England, Hartford, CT
Introduction: Immunoglobulin A (IgA) vasculitis, formerly known as Henoch–Shönlein purpura, is a small vessel vasculitis defined by IgA1-dominant immune complex deposition. It classically presents as a tetrad of palpable purpura, arthralgias, renal involvement, and gastrointestinal (GI) symptoms. While GI manifestations are more commonly recognized in pediatric populations, they are often underdiagnosed in adults. Here, we present a unique cause of adult-onset IgA vasculitis with prominent GI involvement.
Case Description/
Methods: A 35-year-old male with a history of obesity, hypertension and hyperlipidemia presented with chest pain and a purpuric rash on his lower abdomen extending to his extremities. Initially diagnosed with contact dermatitis, he was discharged on systemic and topical steroids. However, he returned two days later with hematemesis, hematochezia, and abdominal pain. Exam revealed a distended, non-tender abdomen with diffuse palpable purpura and bilateral lower extremity edema. CT abdomen/pelvis showed severe jejunal thickening, moderate small bowel wall edema and right-sided colitis. Skin biopsies were obtained and he was treated with systemic steroids and PPIs. Despite initial stabilization, he developed increasing abdominal distention. Repeat imaging showed worsening enteritis and ileus versus a partial small bowel obstruction with moderate-large ascites. Once bowel ischemia and obstruction were ruled out, the patient’s condition normalized with steroids and supportive care. Skin biopsies ultimately confirmed IgA vasculitis with superficial perivascular IgA and C3 deposition, and he was discharged on a steroid taper with ongoing symptom resolution during outpatient follow-up.
Discussion: GI involvement in IgA vasculitis is typically seen with pediatric patients but can occur in adults and may present with significant morbidity. Symptoms typically include abdominal pain, GI bleeding, vomiting and diarrhea. Imaging findings often reveal duodenitis, jejunitis, and ileitis. Although not required, endoscopic biopsy can reveal vasculitis changes such as leukocytoclastic vasculitis and lamina propria hemorrhage even without active symptoms. Severe complications include intussusception, bowel perforation and gallbladder hydrops. Treatment is usually supportive but systemic corticosteroids are often used for severe cases. Immunosuppressants such as mycophenolate or rituximab can be considered for refractory cases. Further studies should be directed at exploring GI manifestations of IgA vasculitis.
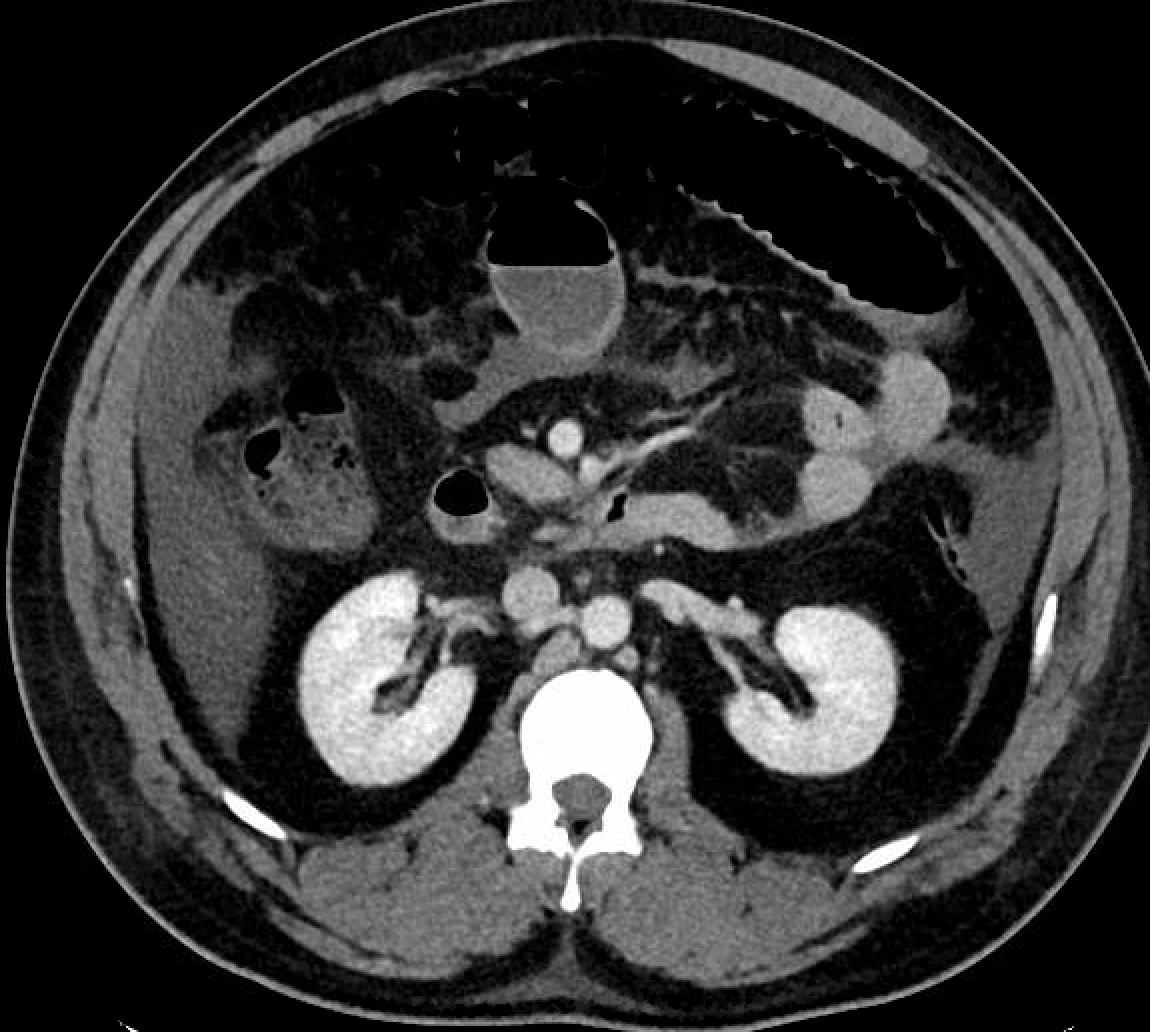
Figure: Figure 1: Worsening small bowel enteritis appreciated on CT abdomen & pelvis

Figure: Figure 2: Abdominal rash consistent with IgA vasculitis
Disclosures:
Rameesha Zubair indicated no relevant financial relationships.
Karmen Brar indicated no relevant financial relationships.
Abdul Khuram indicated no relevant financial relationships.
Akaash Mittal indicated no relevant financial relationships.
Thomas Corredine indicated no relevant financial relationships.
Rameesha Zubair, MBBS1, Karmen Brar, MD1, Abdul Khuram, DO1, Akaash Mittal, MD1, Thomas Corredine, DO2. P4147 - When Purpura Meets Hematemesis: A Rare Adult Onset Presentation of IgA Vasculitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
