Monday Poster Session
Category: Small Intestine
P4142 - Endoscopic Management of a Duodenal Ulcer Perforation in a Decompensated Cirrhotic Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

James Vu, MD
University of California Davis Medical Center
Sacramento, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
James Vu, MD1, Robert Pecha, MD1, Andrew Yen, MD2, Vikrant Rachakonda, MD1
1University of California Davis Medical Center, Sacramento, CA; 2Sacramento VA Medical Center, Veterans Affairs Northern California Health Care System, Mather, CA
Introduction: Duodenal ulcer perforation is a life-threatening complication of peptic ulcer disease (PUD), with increased incidence and mortality in patients with cirrhosis. Surgical repair remains the standard of care, but operative risk is significantly higher in decompensated cirrhotics. Endoscopic stenting offers a potential alternative in non-operative candidates.
Case Description/
Methods: A 69-year-old man with alcohol-related decompensated cirrhosis underwent screening EGD, which revealed a 2 cm duodenal bulb ulcer. The following day, he developed acute abdominal pain and altered mental status. CT imaging revealed free intraperitoneal air consistent with duodenal perforation. Ascitic fluid analysis confirmed spontaneous bacterial peritonitis (19,000 WBC, 90% neutrophils). Due to his decompensated cirrhosis, he was deemed unfit for surgery and managed conservatively with IV antibiotics, bowel rest, and high-dose PPI.
Despite conservative management, he had persistent leukocytosis and imaging identified a loculated abscess. Interventional radiology placed two percutaneous drains. Repeat EGD revealed a 9 mm ulcer at the anterior duodenal bulb. Due to fibrosis and ulcer location, through-the-scope (TTS) clip closure was unsuccessful. Over-the-scope clip and suturing were considered technically unfeasible. A 20 × 80 mm fully covered self-expandable metal stent (fcSEMS) was deployed, spanning the ulcer and anchored proximally in the antrum with TTS clips. The patient improved clinically with no further signs of leak or abscess on follow-up imaging. Six weeks later, EGD confirmed ulcer healing and the stent was removed. Drains were subsequently withdrawn, and the patient was discharged in stable condition.
Discussion: This case demonstrates successful delayed endoscopic stent placement for duodenal perforation in a cirrhotic patient after failed conservative therapy. Reports of fcSEMS for duodenal perforations are limited to early management in non-cirrhotic or postoperative leak scenarios. Although early endoscopic closure is ideal, fibrosis and defect location may preclude clip-based repair. Securely anchored fcSEMS can effectively seal perforations and facilitate healing in high-risk patients. Further studies are needed to establish guidelines for endoscopic management of perforations in cirrhotic populations.
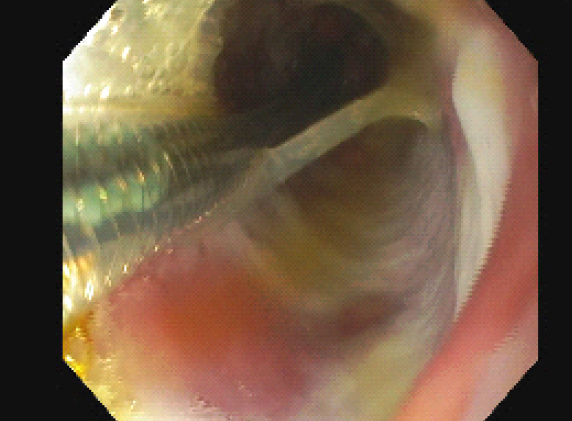
Figure: Follow-up endoscopy with placement of fcSEMS across site of duodenal ulcer perforation
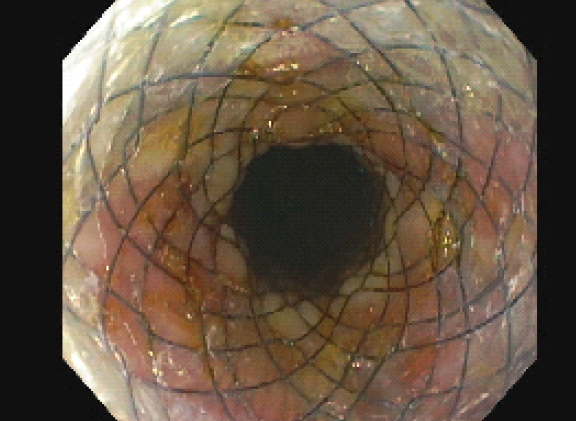
Figure: Visualization of fully expanded fcSEMS
Disclosures:
James Vu indicated no relevant financial relationships.
Robert Pecha indicated no relevant financial relationships.
Andrew Yen indicated no relevant financial relationships.
Vikrant Rachakonda indicated no relevant financial relationships.
James Vu, MD1, Robert Pecha, MD1, Andrew Yen, MD2, Vikrant Rachakonda, MD1. P4142 - Endoscopic Management of a Duodenal Ulcer Perforation in a Decompensated Cirrhotic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
James Vu, MD1, Robert Pecha, MD1, Andrew Yen, MD2, Vikrant Rachakonda, MD1
1University of California Davis Medical Center, Sacramento, CA; 2Sacramento VA Medical Center, Veterans Affairs Northern California Health Care System, Mather, CA
Introduction: Duodenal ulcer perforation is a life-threatening complication of peptic ulcer disease (PUD), with increased incidence and mortality in patients with cirrhosis. Surgical repair remains the standard of care, but operative risk is significantly higher in decompensated cirrhotics. Endoscopic stenting offers a potential alternative in non-operative candidates.
Case Description/
Methods: A 69-year-old man with alcohol-related decompensated cirrhosis underwent screening EGD, which revealed a 2 cm duodenal bulb ulcer. The following day, he developed acute abdominal pain and altered mental status. CT imaging revealed free intraperitoneal air consistent with duodenal perforation. Ascitic fluid analysis confirmed spontaneous bacterial peritonitis (19,000 WBC, 90% neutrophils). Due to his decompensated cirrhosis, he was deemed unfit for surgery and managed conservatively with IV antibiotics, bowel rest, and high-dose PPI.
Despite conservative management, he had persistent leukocytosis and imaging identified a loculated abscess. Interventional radiology placed two percutaneous drains. Repeat EGD revealed a 9 mm ulcer at the anterior duodenal bulb. Due to fibrosis and ulcer location, through-the-scope (TTS) clip closure was unsuccessful. Over-the-scope clip and suturing were considered technically unfeasible. A 20 × 80 mm fully covered self-expandable metal stent (fcSEMS) was deployed, spanning the ulcer and anchored proximally in the antrum with TTS clips. The patient improved clinically with no further signs of leak or abscess on follow-up imaging. Six weeks later, EGD confirmed ulcer healing and the stent was removed. Drains were subsequently withdrawn, and the patient was discharged in stable condition.
Discussion: This case demonstrates successful delayed endoscopic stent placement for duodenal perforation in a cirrhotic patient after failed conservative therapy. Reports of fcSEMS for duodenal perforations are limited to early management in non-cirrhotic or postoperative leak scenarios. Although early endoscopic closure is ideal, fibrosis and defect location may preclude clip-based repair. Securely anchored fcSEMS can effectively seal perforations and facilitate healing in high-risk patients. Further studies are needed to establish guidelines for endoscopic management of perforations in cirrhotic populations.
Figure: Follow-up endoscopy with placement of fcSEMS across site of duodenal ulcer perforation
Figure: Visualization of fully expanded fcSEMS
Disclosures:
James Vu indicated no relevant financial relationships.
Robert Pecha indicated no relevant financial relationships.
Andrew Yen indicated no relevant financial relationships.
Vikrant Rachakonda indicated no relevant financial relationships.
James Vu, MD1, Robert Pecha, MD1, Andrew Yen, MD2, Vikrant Rachakonda, MD1. P4142 - Endoscopic Management of a Duodenal Ulcer Perforation in a Decompensated Cirrhotic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

