Monday Poster Session
Category: Small Intestine
P4140 - Disseminated Histoplasmosis Presenting With Duodenal Outlet Obstruction and Pancreatitis in an Immunocompetent Host
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ridhima Kaul, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Ridhima Kaul, MD1, Arjun Chatterjee, MD1, Roma Patel, MD2, Ari Garber, MD1, Manuel Braga Neto, MD, PhD3
1Cleveland Clinic Foundation, Cleveland, OH; 2Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Histoplasmosis is a systemic fungal infection caused by Histoplasma capsulatum, acquired via spore inhalation in endemic regions. While pulmonary disease is the most common presentation, disseminated histoplasmosis can involve multiple organ systems and is usually seen in immunocompromised individuals. Gastrointestinal (GI) involvement is rare, often underrecognized, and usually presents with vague symptoms such as abdominal pain or diarrhea. Severe complications like ulceration, obstruction, bleeding, or pancreatitis are exceedingly uncommon.
Case Description/
Methods: We report a rare case of disseminated histoplasmosis in a 76-year-old immunocompetent male with type 2 diabetes, BPH, and GERD who presented with 2 months of progressive nausea, vomiting, 50 lb weight loss, and coffee ground emesis. CT abdomen showed fat stranding around the pancreatic head and duodenum, consistent with acute pancreatitis. Upper endoscopy revealed an ulcerated, infiltrative-appearing mass with a stricture at the junction of the first and second portions of the duodenum, raising concern for malignancy and duodenal outlet obstruction . (Fig 1A) Biopsies demonstrated severe active duodenitis with ulceration and budding yeast forms within histiocytes.
He was transferred to our facility due to worsening respiratory failure, and recurrent vomiting. CT imaging showed innumerable pulmonary nodules and mediastinal lymphadenopathy. Urine histoplasma antigen (titer 1:128) and serum antibody testing were positive, and fungal stains confirmed H. capsulatum. He improved initially with itraconazole, but was readmitted for nausea and vomiting with eventual hematemesis 8 weeks later. Repeat EGD now revealed a Mallory-Weiss tear, LA Grade D esophagitis, a large duodenal ulcer, and a non-traversable ulcerated stricture in D1. (Fig 1B) MRI indicated duodenal wall thickening and groove pancreatitis. (Fig 2) Due to recalcitrant symptoms, he underwent exploratory laparotomy and Roux-en-Y gastric bypass; biopsies were benign. His post-operative course was complicated by pulmonary embolism requiring anticoagulation, chronic nausea with poor weight gain, and failure to thrive.
Discussion: This case highlights an uncommon, disseminated presentation of histoplasmosis involving the GI tract. Clinicians should maintain a high index of suspicion for fungal infections in patients with unexplained GI pathology, especially those from endemic areas.
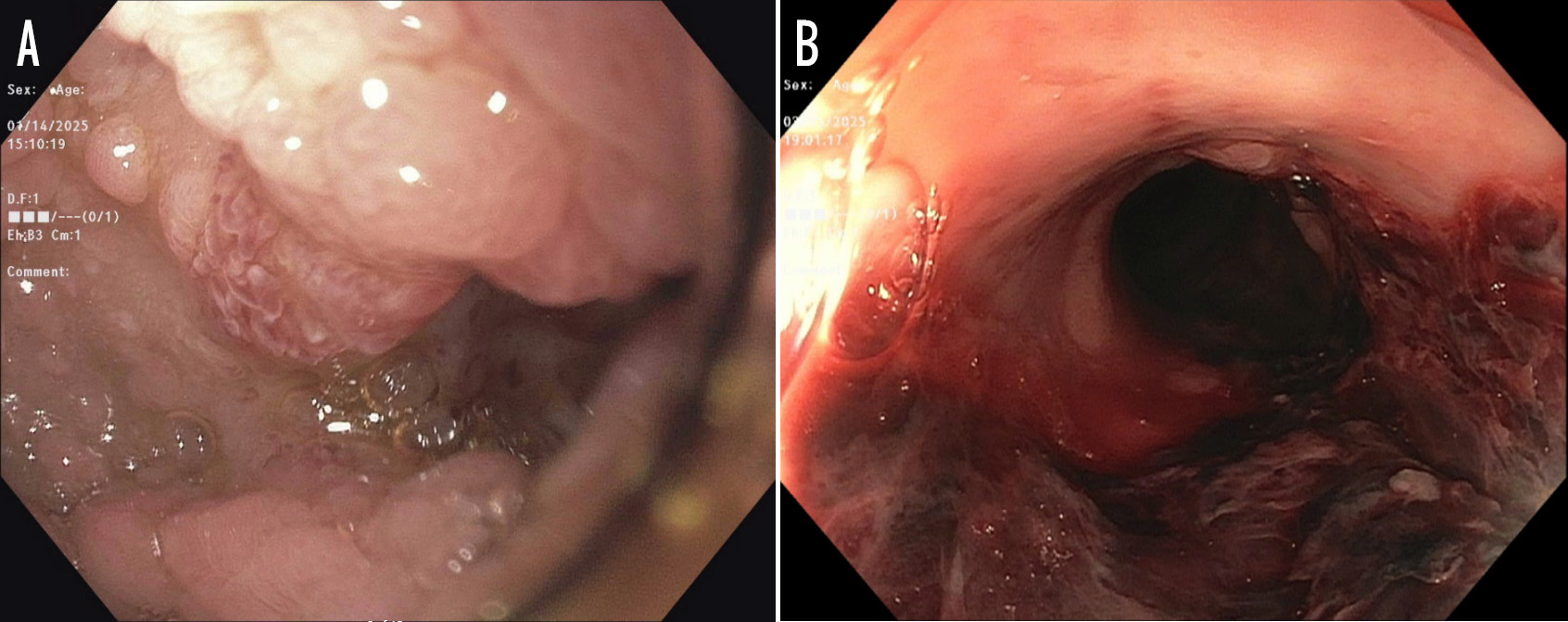
Figure: Figure 1. (A) Initial upper endoscopy revealing an ulcerated, infiltrative, appearing mass with a stricture at the junction of the first and second part of the duodenum. (B) Suspected Esophageal Mallory-Weiss tear

Figure: Figure 2. MRI revealing focal asymmetric wall thickening in the duodenal bulb represents a duodenal mass versus reactive thickening related to the ulcer. Peripancreatic fat stranding suggestive of acute interstitial pancreatitis.
Disclosures:
Ridhima Kaul indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Roma Patel indicated no relevant financial relationships.
Ari Garber indicated no relevant financial relationships.
Manuel Braga Neto indicated no relevant financial relationships.
Ridhima Kaul, MD1, Arjun Chatterjee, MD1, Roma Patel, MD2, Ari Garber, MD1, Manuel Braga Neto, MD, PhD3. P4140 - Disseminated Histoplasmosis Presenting With Duodenal Outlet Obstruction and Pancreatitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Histoplasmosis is a systemic fungal infection caused by Histoplasma capsulatum, acquired via spore inhalation in endemic regions. While pulmonary disease is the most common presentation, disseminated histoplasmosis can involve multiple organ systems and is usually seen in immunocompromised individuals. Gastrointestinal (GI) involvement is rare, often underrecognized, and usually presents with vague symptoms such as abdominal pain or diarrhea. Severe complications like ulceration, obstruction, bleeding, or pancreatitis are exceedingly uncommon.
Case Description/
Methods: We report a rare case of disseminated histoplasmosis in a 76-year-old immunocompetent male with type 2 diabetes, BPH, and GERD who presented with 2 months of progressive nausea, vomiting, 50 lb weight loss, and coffee ground emesis. CT abdomen showed fat stranding around the pancreatic head and duodenum, consistent with acute pancreatitis. Upper endoscopy revealed an ulcerated, infiltrative-appearing mass with a stricture at the junction of the first and second portions of the duodenum, raising concern for malignancy and duodenal outlet obstruction . (Fig 1A) Biopsies demonstrated severe active duodenitis with ulceration and budding yeast forms within histiocytes.
He was transferred to our facility due to worsening respiratory failure, and recurrent vomiting. CT imaging showed innumerable pulmonary nodules and mediastinal lymphadenopathy. Urine histoplasma antigen (titer 1:128) and serum antibody testing were positive, and fungal stains confirmed H. capsulatum. He improved initially with itraconazole, but was readmitted for nausea and vomiting with eventual hematemesis 8 weeks later. Repeat EGD now revealed a Mallory-Weiss tear, LA Grade D esophagitis, a large duodenal ulcer, and a non-traversable ulcerated stricture in D1. (Fig 1B) MRI indicated duodenal wall thickening and groove pancreatitis. (Fig 2) Due to recalcitrant symptoms, he underwent exploratory laparotomy and Roux-en-Y gastric bypass; biopsies were benign. His post-operative course was complicated by pulmonary embolism requiring anticoagulation, chronic nausea with poor weight gain, and failure to thrive.
Discussion: This case highlights an uncommon, disseminated presentation of histoplasmosis involving the GI tract. Clinicians should maintain a high index of suspicion for fungal infections in patients with unexplained GI pathology, especially those from endemic areas.
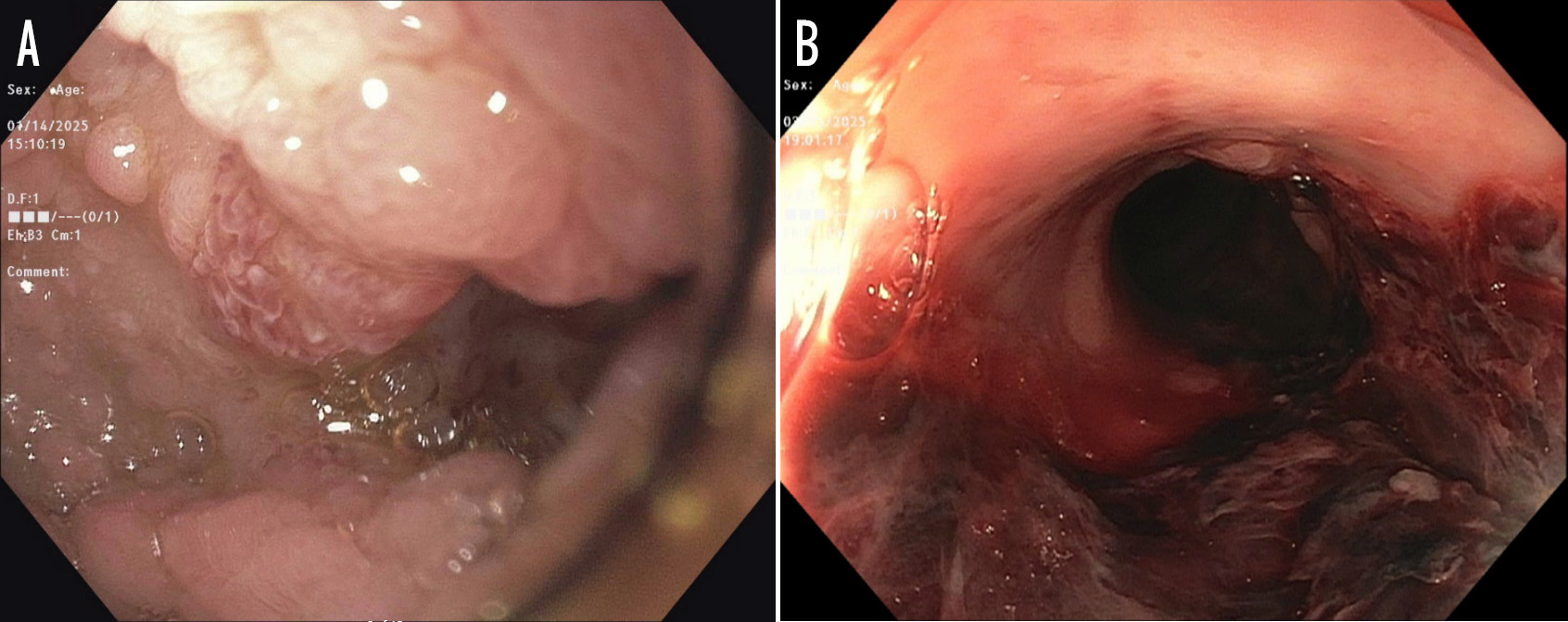
Figure: Figure 1. (A) Initial upper endoscopy revealing an ulcerated, infiltrative, appearing mass with a stricture at the junction of the first and second part of the duodenum. (B) Suspected Esophageal Mallory-Weiss tear

Figure: Figure 2. MRI revealing focal asymmetric wall thickening in the duodenal bulb represents a duodenal mass versus reactive thickening related to the ulcer. Peripancreatic fat stranding suggestive of acute interstitial pancreatitis.
Disclosures:
Ridhima Kaul indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Roma Patel indicated no relevant financial relationships.
Ari Garber indicated no relevant financial relationships.
Manuel Braga Neto indicated no relevant financial relationships.
Ridhima Kaul, MD1, Arjun Chatterjee, MD1, Roma Patel, MD2, Ari Garber, MD1, Manuel Braga Neto, MD, PhD3. P4140 - Disseminated Histoplasmosis Presenting With Duodenal Outlet Obstruction and Pancreatitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
