Monday Poster Session
Category: Small Intestine
P4128 - Triple Threat: A Rare Combination of Collagenous Gastritis, Sprue and Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FK
Fatima Kamal, MD
Connecticut Institute for the Communities
Danbury, CT
Presenting Author(s)
Fatima Kamal, MD1, Lucas Fernet, MBBS2, Faiza Kamal, MBBS2, Spandana Palisetti, MD3, Ramapriya Vidhun, MD3, Neal Patel, MD3
1Connecticut Institute for the Communities, Danbury, CT; 2University of Nottingham, Edmonton, AB, Canada; 3Danbury Hospital, Danbury, CT
Introduction: Collagenous sprue is a rare small bowel enteropathy first described in 1947, with only a few hundred cases reported. It presents with diarrhea, weight loss, and malabsorption, and should be considered in patients with negative celiac serology. We present a case of an 83-year-old female diagnosed with collagenous sprue, collagenous colitis and collagenous gastritis.
Case Description/
Methods: An 83-year-old female presented with postprandial watery diarrhea and a 22kg unintentional weight loss over one year, unresponsive to dietary changes, including BRAT diet. Her physical examination was unremarkable. Celiac serologies were negative, and CRP and fecal calprotectin were normal. Upper endoscopy and colonoscopy showed erythematous gastric body and antrum with diffusely scalloped duodenal mucosa. Duodenal biopsies revealed villous atrophy, inflammatory infiltrates in the lamina propria, and subepithelial collagen deposition consistent with collagenous sprue. Similar subepithelial collagenous thickening was seen in the gastric antrum and colon, consistent with concurrent collagenous gastritis and collagenous colitis. The patient was started on a tapering 9mg budesonide regimen. Diarrhea improved but frequent bowel movements persisted with ongoing weight loss despite a good appetite. Open-capsule budesonide was resumed at 9mg, and a gluten-free diet was initiated despite negative celiac markers. The patient reported improvement upon follow up 3 months later, with reduced stool frequency, formed stools and stabilized weight.
Discussion: Collagenous sprue, colitis and gastritis are diagnosed histologically by subepithelial collagen proliferation of >10mm with entrapment of cellular elements. While they may co-occur, all three are simultaneously present in only ~13% of patients with collagenous sprue. Once considered a severe subtype of celiac disease, collagenous sprue is now regarded as a distinct entity, likely with an inflammatory etiology given its association with autoimmune conditions. There are no clear guidelines for management, with conflicting evidence derived from case reports. Some success has been noted with gluten-free diets and budesonide, while other options include thiopurines, TNF-a inhibitors, and tacrolimus. Though historically associated with poor outcomes, recent reports suggest up to 80% of patients may respond to treatment. Collagenous sprue should be considered in patients with malabsorption and negative celiac serologies, or in those who fail to respond to a gluten-free diet.
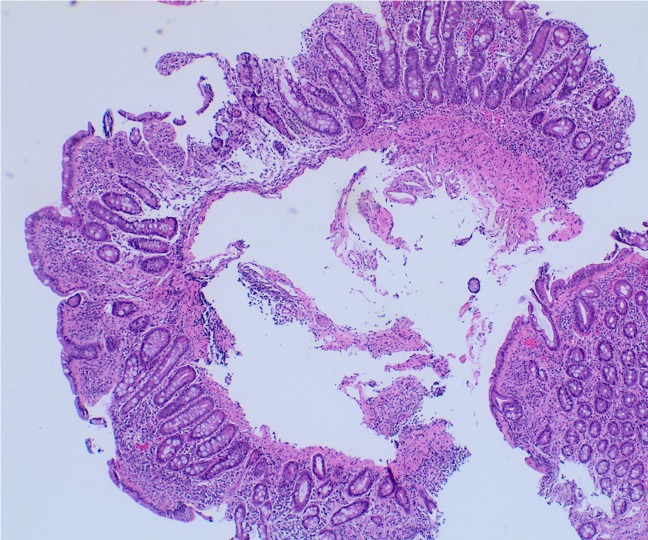
Figure: Duodenal biopsy showing near-total villous blunting, partially denuded surface epithelium with crypt hyperplasia and lymphoplasmacytic infiltrate in the lamina propria. Pathological increase in thickness of the sub-epithelial collagen is also noted. (hematoxylin and eosin stain, 40x).
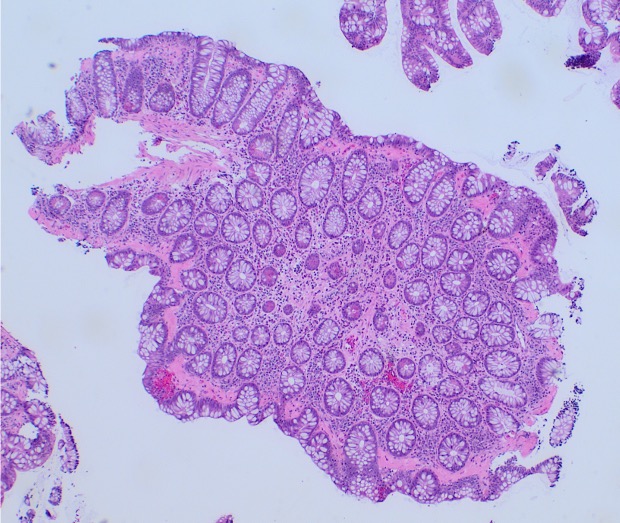
Figure: Colon biopsy showing a thick, hyalinized sub-epithelial collagen deposition, focal sloughing of the surface epithelium. The architecture appears well-preserved. (H&E stain, 40x).
Disclosures:
Fatima Kamal indicated no relevant financial relationships.
Lucas Fernet indicated no relevant financial relationships.
Faiza Kamal indicated no relevant financial relationships.
Spandana Palisetti indicated no relevant financial relationships.
Ramapriya Vidhun indicated no relevant financial relationships.
Neal Patel indicated no relevant financial relationships.
Fatima Kamal, MD1, Lucas Fernet, MBBS2, Faiza Kamal, MBBS2, Spandana Palisetti, MD3, Ramapriya Vidhun, MD3, Neal Patel, MD3. P4128 - Triple Threat: A Rare Combination of Collagenous Gastritis, Sprue and Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Connecticut Institute for the Communities, Danbury, CT; 2University of Nottingham, Edmonton, AB, Canada; 3Danbury Hospital, Danbury, CT
Introduction: Collagenous sprue is a rare small bowel enteropathy first described in 1947, with only a few hundred cases reported. It presents with diarrhea, weight loss, and malabsorption, and should be considered in patients with negative celiac serology. We present a case of an 83-year-old female diagnosed with collagenous sprue, collagenous colitis and collagenous gastritis.
Case Description/
Methods: An 83-year-old female presented with postprandial watery diarrhea and a 22kg unintentional weight loss over one year, unresponsive to dietary changes, including BRAT diet. Her physical examination was unremarkable. Celiac serologies were negative, and CRP and fecal calprotectin were normal. Upper endoscopy and colonoscopy showed erythematous gastric body and antrum with diffusely scalloped duodenal mucosa. Duodenal biopsies revealed villous atrophy, inflammatory infiltrates in the lamina propria, and subepithelial collagen deposition consistent with collagenous sprue. Similar subepithelial collagenous thickening was seen in the gastric antrum and colon, consistent with concurrent collagenous gastritis and collagenous colitis. The patient was started on a tapering 9mg budesonide regimen. Diarrhea improved but frequent bowel movements persisted with ongoing weight loss despite a good appetite. Open-capsule budesonide was resumed at 9mg, and a gluten-free diet was initiated despite negative celiac markers. The patient reported improvement upon follow up 3 months later, with reduced stool frequency, formed stools and stabilized weight.
Discussion: Collagenous sprue, colitis and gastritis are diagnosed histologically by subepithelial collagen proliferation of >10mm with entrapment of cellular elements. While they may co-occur, all three are simultaneously present in only ~13% of patients with collagenous sprue. Once considered a severe subtype of celiac disease, collagenous sprue is now regarded as a distinct entity, likely with an inflammatory etiology given its association with autoimmune conditions. There are no clear guidelines for management, with conflicting evidence derived from case reports. Some success has been noted with gluten-free diets and budesonide, while other options include thiopurines, TNF-a inhibitors, and tacrolimus. Though historically associated with poor outcomes, recent reports suggest up to 80% of patients may respond to treatment. Collagenous sprue should be considered in patients with malabsorption and negative celiac serologies, or in those who fail to respond to a gluten-free diet.
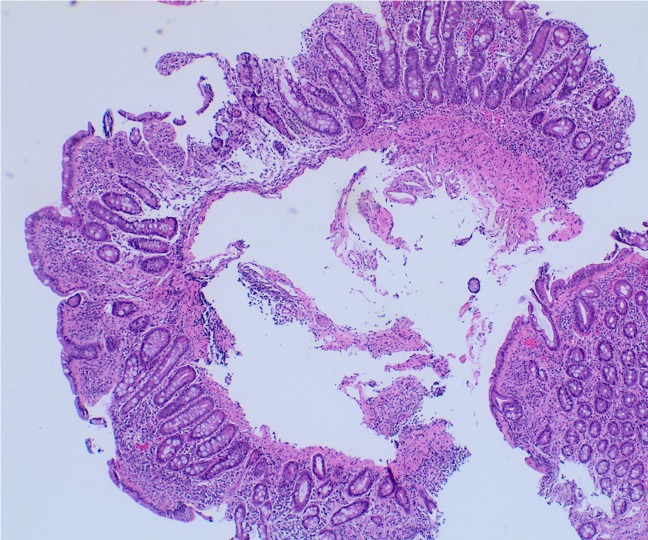
Figure: Duodenal biopsy showing near-total villous blunting, partially denuded surface epithelium with crypt hyperplasia and lymphoplasmacytic infiltrate in the lamina propria. Pathological increase in thickness of the sub-epithelial collagen is also noted. (hematoxylin and eosin stain, 40x).
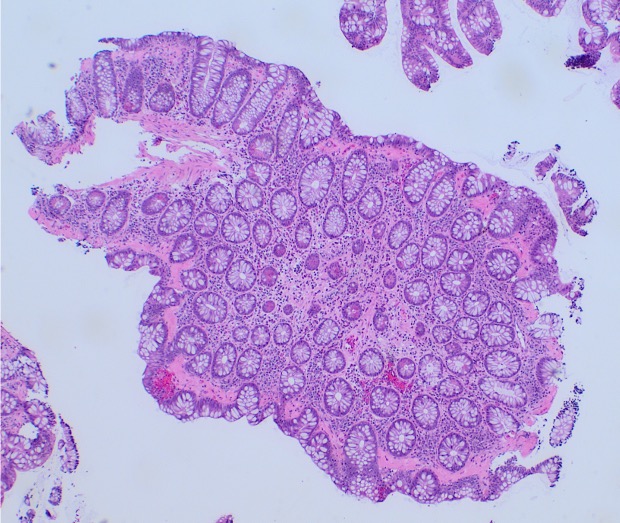
Figure: Colon biopsy showing a thick, hyalinized sub-epithelial collagen deposition, focal sloughing of the surface epithelium. The architecture appears well-preserved. (H&E stain, 40x).
Disclosures:
Fatima Kamal indicated no relevant financial relationships.
Lucas Fernet indicated no relevant financial relationships.
Faiza Kamal indicated no relevant financial relationships.
Spandana Palisetti indicated no relevant financial relationships.
Ramapriya Vidhun indicated no relevant financial relationships.
Neal Patel indicated no relevant financial relationships.
Fatima Kamal, MD1, Lucas Fernet, MBBS2, Faiza Kamal, MBBS2, Spandana Palisetti, MD3, Ramapriya Vidhun, MD3, Neal Patel, MD3. P4128 - Triple Threat: A Rare Combination of Collagenous Gastritis, Sprue and Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
