Monday Poster Session
Category: Small Intestine
P4109 - Beyond the Pancreas: Two Atypical Presentations of VIPoma Requiring Multidisciplinary Care
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FA
Fatima Ahson, MD (she/her/hers)
University of Illinois College of Medicine Peoria
Peoria, Illinois
Presenting Author(s)
Yusuf Kagzi, MD1, Fatima Ahson, MD2, Eugene Annor, MD2, Imran Balouch, MD1
1University of Illinois College of Medicine, Peoria, IL; 2University of Illinois College of Medicine Peoria, Peoria, IL
Introduction: VIPomas are rare neuroendocrine tumors, typically originating in the pancreas, secrete vasoactive intestinal peptide (VIP), causing profound secretory diarrhea. Atypical presentation like extra-pancreatic and malignant VIPomas are exceedingly rare. We present two diagnostically and therapeutically challenging cases of VIPomas illustrating role of multidisciplinary management in complex neuroendocrine disorders.
Case Description/
Methods: Case 1: A 40-year-old male with asymptomatic HIV was admitted for hypertensive urgency and found to have a large left adrenal mass (9.8 × 7.5 × 7.4 cm). Lab work revealed elevated serum metanephrines, consistent with pheochromocytoma. Concurrently, he developed severe, high-output secretory diarrhea ( >3L/day) with severe electrolyte abnormalities. Extensive gastrointestinal evaluation excluded infectious and pancreatic causes. Elevated serum VIP level (954 pg/mL) confirmed VIPoma physiology. Imaging showed no pancreatic lesion, suggesting an extra-pancreatic adrenal VIPoma (Figure 1). Immunostaining of the adrenal lesion was positive for synaptophysin and chromogranin. Associated hypercalcemia and suspected parathyroid adenoma raised concern for MEN2; however, RET mutation testing was negative. He underwent preoperative alpha- and beta-blockade followed by adrenalectomy. Postoperatively, diarrhea and electrolyte disturbances resolved, allowing discontinuation of octreotide and antidiarrheals.
Case 2: A 54-year-old male with a well-differentiated small intestinal VIPoma metastatic to lymph nodes and mesentery underwent partial small bowel resection and lymph node debulking, with the dominant mesenteric mass left unresected to avoid short gut syndrome (Figure 2). Postoperative persistent diarrhea was managed with lanreotide and telotristat ethyl. Chronic diarrhea caused significant mucosal trauma, forming a transsphincteric perianal fistula and broad-based anal fissures with internal sphincter exposure. These painful anorectal complications required multidisciplinary intervention, including surgery evaluation, botulinum toxin injection to the internal sphincter, and bilateral pudendal nerve blocks. Persistent pelvic pain necessitated CT-guided pudendal nerve ablation, resulting in symptom improvement.
Discussion: These cases highlight complications of VIPoma syndromes, requiring comprehensive management with multidisciplinary care to address the multifaceted challenges, improving quality of life in this complex population.
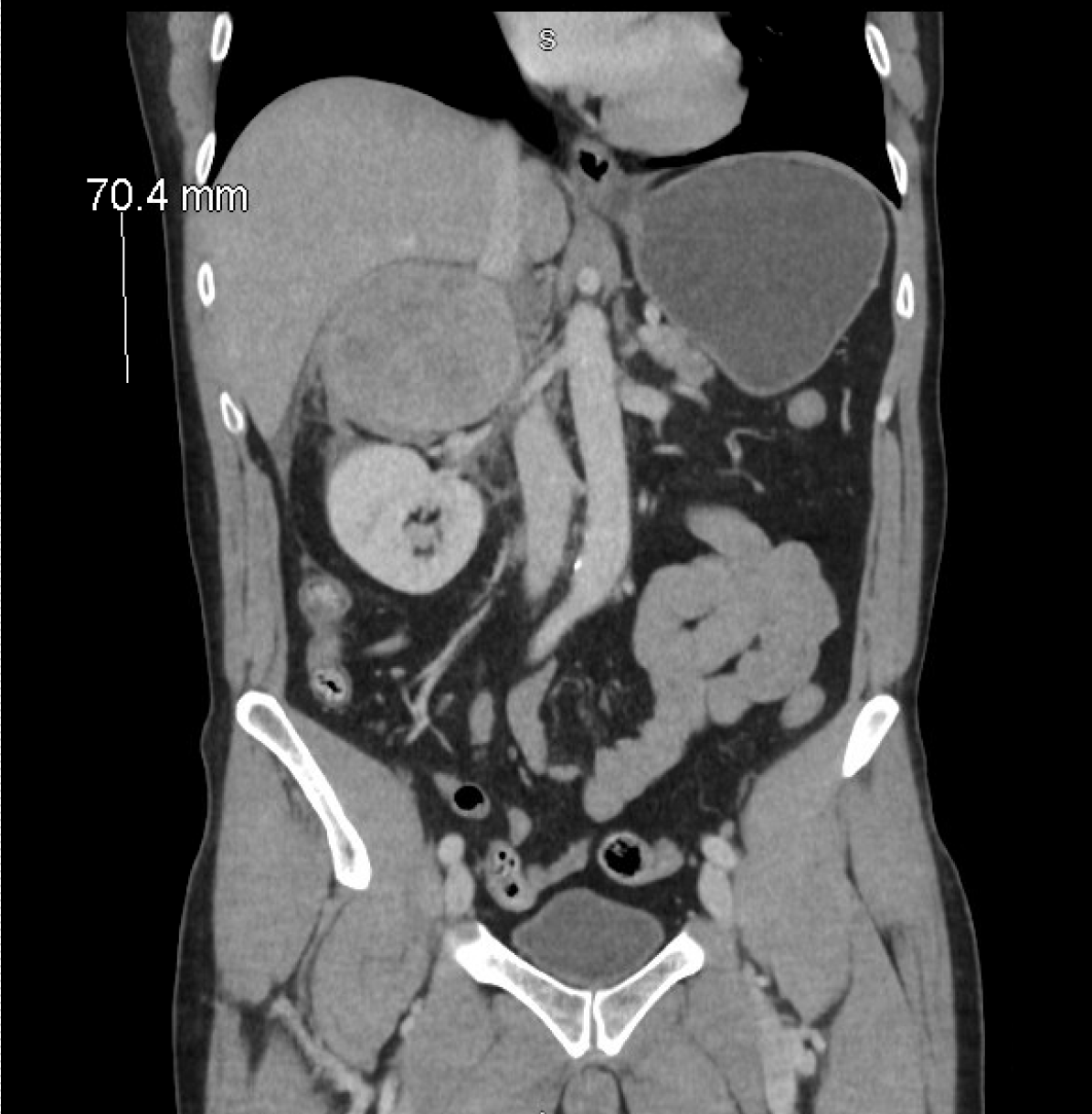
Figure: Figure 1: Large heterogeneous mass centered on the right adrenal gland measures 9.3 x 7.8 x 7.0 cm concerning for pheochromocytoma
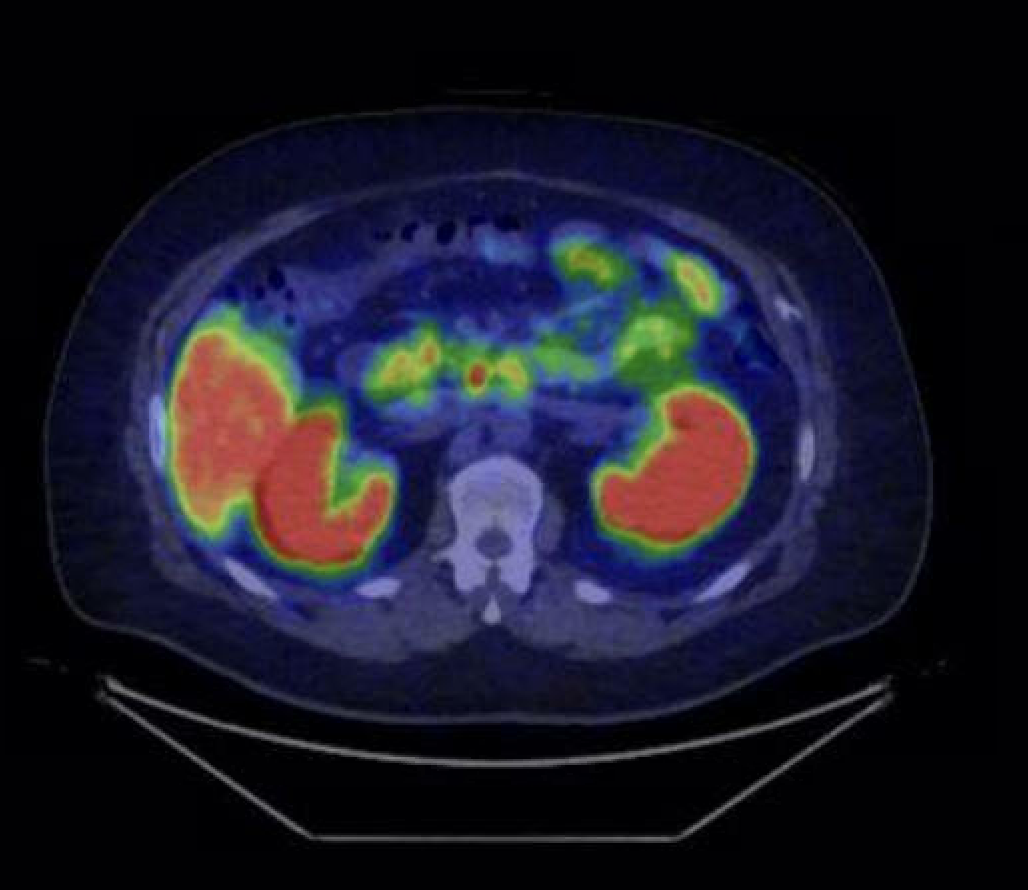
Figure: Figure 2: Positron emission tomography (PET) scan showing right-sided mesenteric soft tissue mass near the prior small bowel resection site, measuring 2.6 cm and adjacent metastatic lesions with radiotracer uptake.
Disclosures:
Yusuf Kagzi indicated no relevant financial relationships.
Fatima Ahson indicated no relevant financial relationships.
Eugene Annor indicated no relevant financial relationships.
Imran Balouch indicated no relevant financial relationships.
Yusuf Kagzi, MD1, Fatima Ahson, MD2, Eugene Annor, MD2, Imran Balouch, MD1. P4109 - Beyond the Pancreas: Two Atypical Presentations of VIPoma Requiring Multidisciplinary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Peoria, IL; 2University of Illinois College of Medicine Peoria, Peoria, IL
Introduction: VIPomas are rare neuroendocrine tumors, typically originating in the pancreas, secrete vasoactive intestinal peptide (VIP), causing profound secretory diarrhea. Atypical presentation like extra-pancreatic and malignant VIPomas are exceedingly rare. We present two diagnostically and therapeutically challenging cases of VIPomas illustrating role of multidisciplinary management in complex neuroendocrine disorders.
Case Description/
Methods: Case 1: A 40-year-old male with asymptomatic HIV was admitted for hypertensive urgency and found to have a large left adrenal mass (9.8 × 7.5 × 7.4 cm). Lab work revealed elevated serum metanephrines, consistent with pheochromocytoma. Concurrently, he developed severe, high-output secretory diarrhea ( >3L/day) with severe electrolyte abnormalities. Extensive gastrointestinal evaluation excluded infectious and pancreatic causes. Elevated serum VIP level (954 pg/mL) confirmed VIPoma physiology. Imaging showed no pancreatic lesion, suggesting an extra-pancreatic adrenal VIPoma (Figure 1). Immunostaining of the adrenal lesion was positive for synaptophysin and chromogranin. Associated hypercalcemia and suspected parathyroid adenoma raised concern for MEN2; however, RET mutation testing was negative. He underwent preoperative alpha- and beta-blockade followed by adrenalectomy. Postoperatively, diarrhea and electrolyte disturbances resolved, allowing discontinuation of octreotide and antidiarrheals.
Case 2: A 54-year-old male with a well-differentiated small intestinal VIPoma metastatic to lymph nodes and mesentery underwent partial small bowel resection and lymph node debulking, with the dominant mesenteric mass left unresected to avoid short gut syndrome (Figure 2). Postoperative persistent diarrhea was managed with lanreotide and telotristat ethyl. Chronic diarrhea caused significant mucosal trauma, forming a transsphincteric perianal fistula and broad-based anal fissures with internal sphincter exposure. These painful anorectal complications required multidisciplinary intervention, including surgery evaluation, botulinum toxin injection to the internal sphincter, and bilateral pudendal nerve blocks. Persistent pelvic pain necessitated CT-guided pudendal nerve ablation, resulting in symptom improvement.
Discussion: These cases highlight complications of VIPoma syndromes, requiring comprehensive management with multidisciplinary care to address the multifaceted challenges, improving quality of life in this complex population.
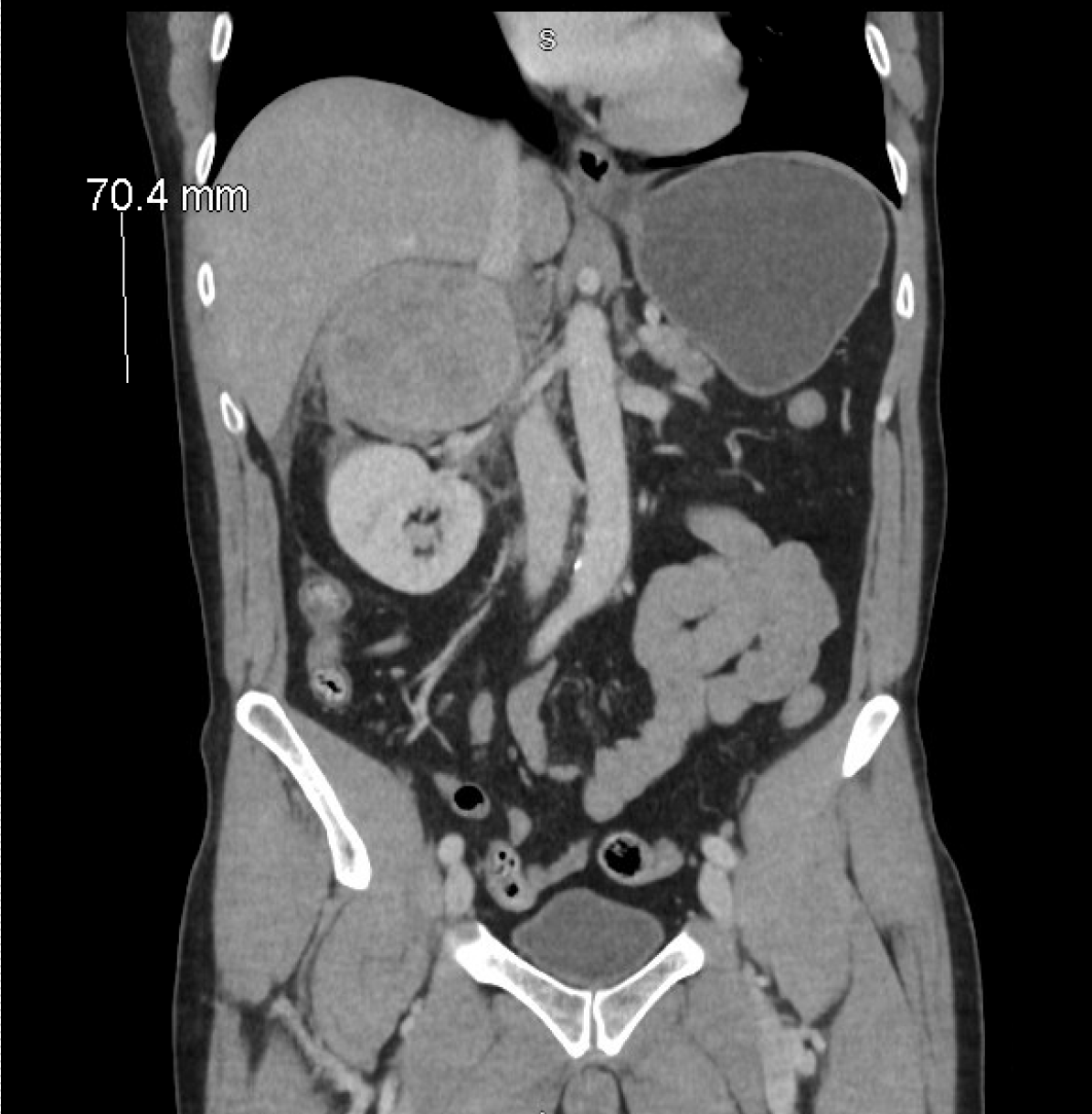
Figure: Figure 1: Large heterogeneous mass centered on the right adrenal gland measures 9.3 x 7.8 x 7.0 cm concerning for pheochromocytoma
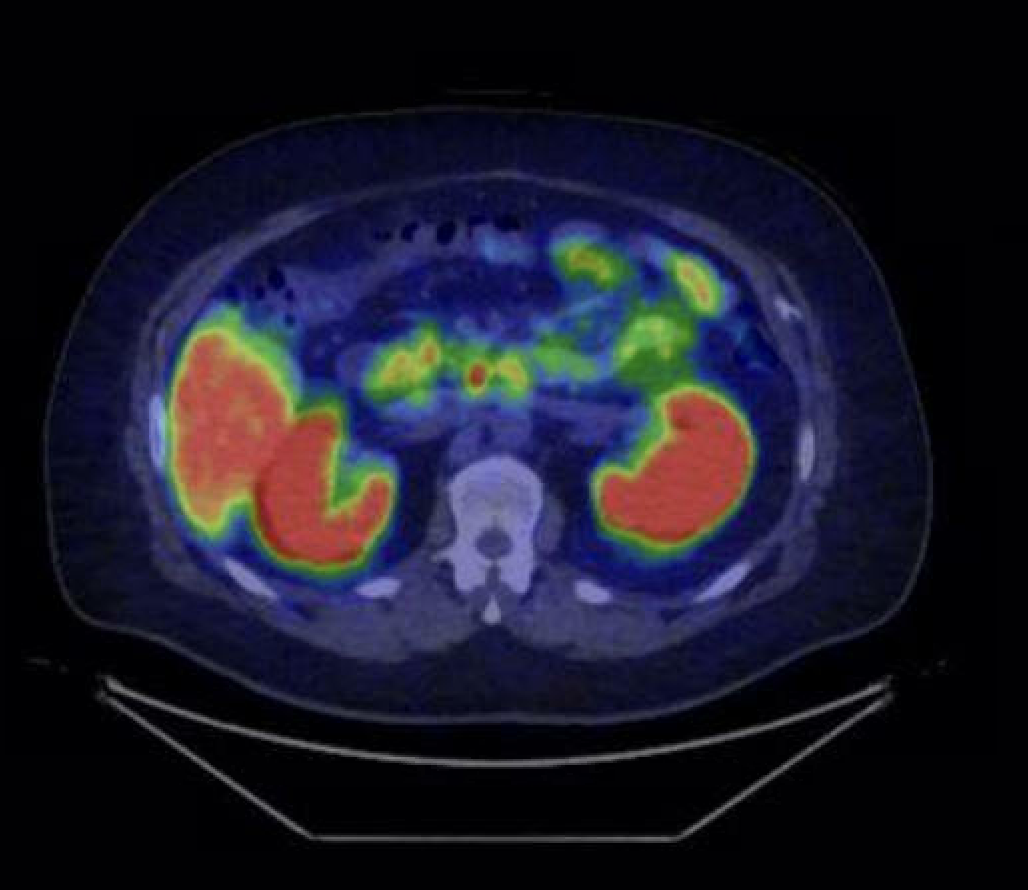
Figure: Figure 2: Positron emission tomography (PET) scan showing right-sided mesenteric soft tissue mass near the prior small bowel resection site, measuring 2.6 cm and adjacent metastatic lesions with radiotracer uptake.
Disclosures:
Yusuf Kagzi indicated no relevant financial relationships.
Fatima Ahson indicated no relevant financial relationships.
Eugene Annor indicated no relevant financial relationships.
Imran Balouch indicated no relevant financial relationships.
Yusuf Kagzi, MD1, Fatima Ahson, MD2, Eugene Annor, MD2, Imran Balouch, MD1. P4109 - Beyond the Pancreas: Two Atypical Presentations of VIPoma Requiring Multidisciplinary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
