Monday Poster Session
Category: Small Intestine
P4107 - When TTG-IgA Fails: Diagnostic Insights from an IgG-Dominant Presentation of Celiac Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sandra Elmasry, MD
Mayo Clinic
Scottsdale, AZ
Presenting Author(s)
Sandra Elmasry, MD1, Stacey Rolak, MD, MPH2, Rosita Frazier, MD1, Amy S.. Oxentenko, MD3, Lucinda Harris, MD1
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic Arizona, Phoenix, AZ; 3Mayo Clinic, Rochester, MN
Introduction: Celiac disease (CD) is an autoimmune disorder affecting ~1% of the population. Diagnosis involves serologic testing and histologic confirmation. The ACG recommends initial screening with tissue transglutaminase IgA antibodies (TTG-IgA) and total IgA while on a gluten-containing diet. If TTG-IgA is elevated, diagnosis is confirmed via esophagogastroduodenoscopy (EGD) with duodenal biopsies. Here, we present a diagnostically challenging case of CD with an atypical serologic profile
Case Description/
Methods: A 25-year-old woman presented with three months of epigastric and left lower quadrant pain radiating to the chest, bloating, intermittent loose stools, heartburn, arthralgias, and a pruritic hand rash. She also experienced a 50–60 lb unintentional weight loss over six months. Initial serologies revealed normal total IgA (84), markedly elevated TTG-IgG, and minimally elevated TTG-IgA (Table). She was positive for HLA-DQA105 and HLA-DQB102, consistent with celiac disease susceptibility.
Despite the atypical serology—mildly elevated TTG-IgA and markedly elevated TTG-IgG in an IgA-sufficient patient—an EGD and colonoscopy were performed in March 2024. Colonoscopy was unremarkable, but the EGD showed blunted villi in the bulb and second portion of the duodenum. Biopsies revealed patchy villous atrophy, crypt hyperplasia, and increased intraepithelial lymphocytes, consistent with celiac disease. Other causes of enteropathy were ruled out. Repeat serology in August 2024, after six months on a gluten-free diet, showed overall improvement (Table), paralleled by symptom resolution
Discussion: This case highlights the diagnostic dilemma of CD in IgA-sufficient patients with isolated TTG-IgG elevations and only mild TTG-IgA elevation. Traditionally, TTG-IgG is reserved for those with IgA deficiency, and its utility in IgA-sufficient individuals remains poorly defined. Data suggest that isolated TTG-IgG positivity in IgA-sufficient patients has limited diagnostic yield (with one study showing only a 3% diagnostic rate), TTG-IgA demonstrates high diagnostic accuracy (with a sensitivity of 90.7% and specificity of 87.4% in adults), and endomysial antibody (EMA) testing offers near-perfect specificity and is often used as a confirmatory test. While these data support current guidelines for celiac disease screening and diagnosis, this case highlights that, especially in atypical scenarios, it is crucial to integrate serologic, endoscopic, histologic, and clinical findings to ensure an accurate diagnosis of CD
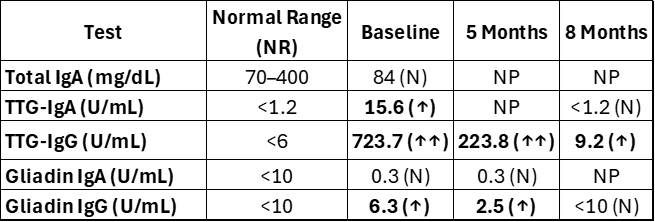
Figure: Table: All serological testing performed showing TTG-IgG markedly elevation and decrease with gluten free diet while TTG-IgA is slightly elevated becoming normal with diet.
Disclosures:
Sandra Elmasry indicated no relevant financial relationships.
Stacey Rolak indicated no relevant financial relationships.
Rosita Frazier indicated no relevant financial relationships.
Amy Oxentenko indicated no relevant financial relationships.
Lucinda Harris: Anyx – Grant/Research Support. Ardelyx – Consultant, Educational video. Gemelli Biotech – Advisory Committee/Board Member, Consultant. GI Health Foundation – Advisor or Review Panel Member. Rome – Member. Salix Pharmaceuticals – Consultant. Takeda – Grant/Research Support.
Sandra Elmasry, MD1, Stacey Rolak, MD, MPH2, Rosita Frazier, MD1, Amy S.. Oxentenko, MD3, Lucinda Harris, MD1. P4107 - When TTG-IgA Fails: Diagnostic Insights from an IgG-Dominant Presentation of Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic Arizona, Phoenix, AZ; 3Mayo Clinic, Rochester, MN
Introduction: Celiac disease (CD) is an autoimmune disorder affecting ~1% of the population. Diagnosis involves serologic testing and histologic confirmation. The ACG recommends initial screening with tissue transglutaminase IgA antibodies (TTG-IgA) and total IgA while on a gluten-containing diet. If TTG-IgA is elevated, diagnosis is confirmed via esophagogastroduodenoscopy (EGD) with duodenal biopsies. Here, we present a diagnostically challenging case of CD with an atypical serologic profile
Case Description/
Methods: A 25-year-old woman presented with three months of epigastric and left lower quadrant pain radiating to the chest, bloating, intermittent loose stools, heartburn, arthralgias, and a pruritic hand rash. She also experienced a 50–60 lb unintentional weight loss over six months. Initial serologies revealed normal total IgA (84), markedly elevated TTG-IgG, and minimally elevated TTG-IgA (Table). She was positive for HLA-DQA105 and HLA-DQB102, consistent with celiac disease susceptibility.
Despite the atypical serology—mildly elevated TTG-IgA and markedly elevated TTG-IgG in an IgA-sufficient patient—an EGD and colonoscopy were performed in March 2024. Colonoscopy was unremarkable, but the EGD showed blunted villi in the bulb and second portion of the duodenum. Biopsies revealed patchy villous atrophy, crypt hyperplasia, and increased intraepithelial lymphocytes, consistent with celiac disease. Other causes of enteropathy were ruled out. Repeat serology in August 2024, after six months on a gluten-free diet, showed overall improvement (Table), paralleled by symptom resolution
Discussion: This case highlights the diagnostic dilemma of CD in IgA-sufficient patients with isolated TTG-IgG elevations and only mild TTG-IgA elevation. Traditionally, TTG-IgG is reserved for those with IgA deficiency, and its utility in IgA-sufficient individuals remains poorly defined. Data suggest that isolated TTG-IgG positivity in IgA-sufficient patients has limited diagnostic yield (with one study showing only a 3% diagnostic rate), TTG-IgA demonstrates high diagnostic accuracy (with a sensitivity of 90.7% and specificity of 87.4% in adults), and endomysial antibody (EMA) testing offers near-perfect specificity and is often used as a confirmatory test. While these data support current guidelines for celiac disease screening and diagnosis, this case highlights that, especially in atypical scenarios, it is crucial to integrate serologic, endoscopic, histologic, and clinical findings to ensure an accurate diagnosis of CD
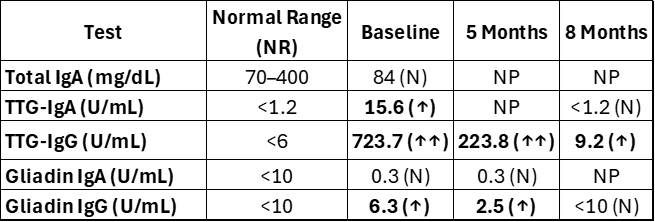
Figure: Table: All serological testing performed showing TTG-IgG markedly elevation and decrease with gluten free diet while TTG-IgA is slightly elevated becoming normal with diet.
Disclosures:
Sandra Elmasry indicated no relevant financial relationships.
Stacey Rolak indicated no relevant financial relationships.
Rosita Frazier indicated no relevant financial relationships.
Amy Oxentenko indicated no relevant financial relationships.
Lucinda Harris: Anyx – Grant/Research Support. Ardelyx – Consultant, Educational video. Gemelli Biotech – Advisory Committee/Board Member, Consultant. GI Health Foundation – Advisor or Review Panel Member. Rome – Member. Salix Pharmaceuticals – Consultant. Takeda – Grant/Research Support.
Sandra Elmasry, MD1, Stacey Rolak, MD, MPH2, Rosita Frazier, MD1, Amy S.. Oxentenko, MD3, Lucinda Harris, MD1. P4107 - When TTG-IgA Fails: Diagnostic Insights from an IgG-Dominant Presentation of Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

