Monday Poster Session
Category: Small Intestine
P4083 - Beyond the Surface: Duodenal-Type Follicular Lymphoma Diagnosed Despite Normal Endoscopy and PET-CT
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Zach Vinton, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Zach Vinton, DO, Carter Schulz, MD, Sarah Malik, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Duodenal-type follicular lymphoma (DTFL) is a rare, localized variant of follicular lymphoma, accounting for 1-3.6% of follicular lymphoma cases and 4% of GI cancers. Due to its indolent course, a watch-and-wait strategy is often used. We describe a patient with fatigue and iron deficiency anemia, found to have biopsy-proven DTFL despite unremarkable endoscopic and positron emission tomography (PET)/computed tomography (CT) findings.
Case Description/
Methods: A 60-year-old male presented to his primary care physician with fatigue, shortness of breath, and restless leg symptoms. He had non-Hodgkin Lymphoma (NHL) 30 years earlier, treated with chemotherapy and since in remission. He reported acid reflux and hemorrhoidal bleeding but no melena, weight loss, or fever. He denied use of NSAIDs, alcohol, and tobacco. Colonoscopy from 10 years ago was normal.
Workup revealed low ferritin and a mild normocytic anemia, so he was started on iron supplementation and referred for endoscopic evaluation. Esophagogastroduodenoscopy (EGD) revealed a 15 mm gastric ulcer in the fundus, multiple small polyps in the body, patchy erythema throughout the stomach, and a grossly normal duodenum (Figure 1). The colonoscopy was unremarkable. Stomach biopsies showed focal iron deposition at the ulcer, suggestive of iron pill gastritis, and were negative for H. pylori. His duodenal biopsies in the first and second portions of the duodenum showed follicular lymphoma. He was referred to oncology, and PET-CT showed mildly prominent central mesenteric lymph nodes but no discrete metabolically active duodenal lesion to correspond to the lymphoma found on biopsy. He began treatment with rituximab monotherapy for stage IVA follicular lymphoma.
Discussion: This case highlights the diagnostic challenge DTFL poses, particularly the discordance between often unremarkable findings on endoscopy and PET imaging, but with evidence of malignancy histologically. It underscores the limitations of standard diagnostic modalities in low-burden mucosal lymphoma. Although the patient’s history of NHL was initially thought to be unrelated, it raises the question of if his malignancy represented a late relapse or metachronous lymphoproliferative process. Given its highly indolent features, clinicians should include gastrointestinal lymphoma in the differential with subtle symptoms such as fatigue with iron deficiency anemia, even with unrevealing imaging and endoscopy. This demonstrates the diagnostic value of random endoscopic biopsies.
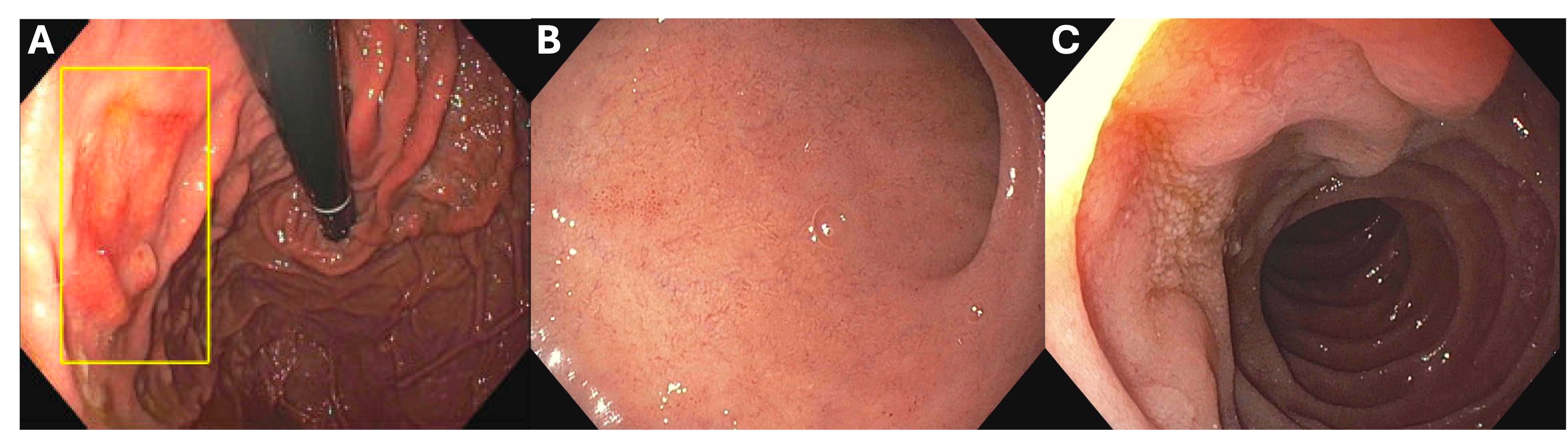
Figure: Figure 1: (A) 15 mm gastric body ulcer. (B) First portion of the duodenum. (C) Second portion of the duodenum.
Disclosures:
Zach Vinton indicated no relevant financial relationships.
Carter Schulz indicated no relevant financial relationships.
Sarah Malik indicated no relevant financial relationships.
Zach Vinton, DO, Carter Schulz, MD, Sarah Malik, MD. P4083 - Beyond the Surface: Duodenal-Type Follicular Lymphoma Diagnosed Despite Normal Endoscopy and PET-CT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Nebraska Medical Center, Omaha, NE
Introduction: Duodenal-type follicular lymphoma (DTFL) is a rare, localized variant of follicular lymphoma, accounting for 1-3.6% of follicular lymphoma cases and 4% of GI cancers. Due to its indolent course, a watch-and-wait strategy is often used. We describe a patient with fatigue and iron deficiency anemia, found to have biopsy-proven DTFL despite unremarkable endoscopic and positron emission tomography (PET)/computed tomography (CT) findings.
Case Description/
Methods: A 60-year-old male presented to his primary care physician with fatigue, shortness of breath, and restless leg symptoms. He had non-Hodgkin Lymphoma (NHL) 30 years earlier, treated with chemotherapy and since in remission. He reported acid reflux and hemorrhoidal bleeding but no melena, weight loss, or fever. He denied use of NSAIDs, alcohol, and tobacco. Colonoscopy from 10 years ago was normal.
Workup revealed low ferritin and a mild normocytic anemia, so he was started on iron supplementation and referred for endoscopic evaluation. Esophagogastroduodenoscopy (EGD) revealed a 15 mm gastric ulcer in the fundus, multiple small polyps in the body, patchy erythema throughout the stomach, and a grossly normal duodenum (Figure 1). The colonoscopy was unremarkable. Stomach biopsies showed focal iron deposition at the ulcer, suggestive of iron pill gastritis, and were negative for H. pylori. His duodenal biopsies in the first and second portions of the duodenum showed follicular lymphoma. He was referred to oncology, and PET-CT showed mildly prominent central mesenteric lymph nodes but no discrete metabolically active duodenal lesion to correspond to the lymphoma found on biopsy. He began treatment with rituximab monotherapy for stage IVA follicular lymphoma.
Discussion: This case highlights the diagnostic challenge DTFL poses, particularly the discordance between often unremarkable findings on endoscopy and PET imaging, but with evidence of malignancy histologically. It underscores the limitations of standard diagnostic modalities in low-burden mucosal lymphoma. Although the patient’s history of NHL was initially thought to be unrelated, it raises the question of if his malignancy represented a late relapse or metachronous lymphoproliferative process. Given its highly indolent features, clinicians should include gastrointestinal lymphoma in the differential with subtle symptoms such as fatigue with iron deficiency anemia, even with unrevealing imaging and endoscopy. This demonstrates the diagnostic value of random endoscopic biopsies.
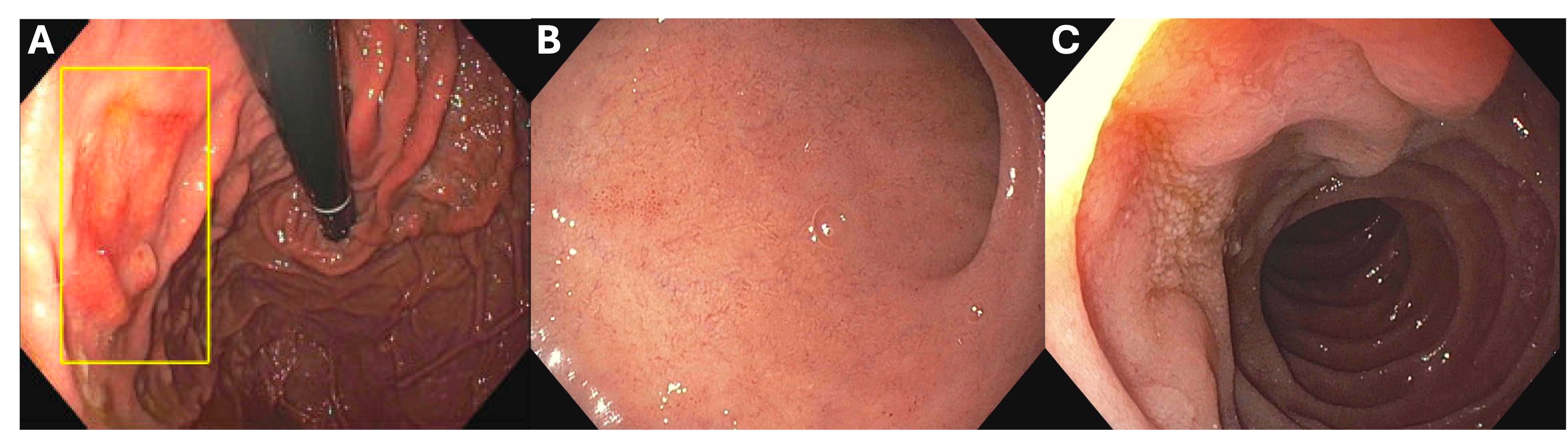
Figure: Figure 1: (A) 15 mm gastric body ulcer. (B) First portion of the duodenum. (C) Second portion of the duodenum.
Disclosures:
Zach Vinton indicated no relevant financial relationships.
Carter Schulz indicated no relevant financial relationships.
Sarah Malik indicated no relevant financial relationships.
Zach Vinton, DO, Carter Schulz, MD, Sarah Malik, MD. P4083 - Beyond the Surface: Duodenal-Type Follicular Lymphoma Diagnosed Despite Normal Endoscopy and PET-CT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
