Monday Poster Session
Category: Small Intestine
P4071 - Sex Differences in Cardiovascular Risk in Patients With Celiac Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Joy Zhao, MD
Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Joy Zhao, MD1, Jason Lin, MD2, John Lin, BS3, Stephanie Moleski, MD1
1Thomas Jefferson University, Philadelphia, PA; 2University of Texas at Houston, Houston, TX; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA
Introduction: Cardiovascular disease (CVD) is a leading cause of death in women, but female sex is protective against poor cardiovascular outcomes. Additionally, the atherosclerotic cardiovascular disease (ASCVD) calculator does not account for autoimmune disease in its assessment.
Although studies show that individuals with celiac disease (CeD) exhibit a modestly elevated risk of cardiovascular disease, no studies have specifically investigated the cardiovascular risk among females with celiac disease in comparison to both male and female control cohorts. This study seeks to address that gap.
Methods: Using TriNetX, a research database with millions of de-identified patient information, a multi-center retrospective cohort analysis was performed. Control cohorts were male or female patients >18 years old with hypertension (HTN), diabetes mellitus (DM), and hyperlipidemia (HLD). Autoimmune diseases like psoriasis, systemic lupus erythematosus (SLE), ulcerative colitis (UC), Crohn's disease (CD), and CeD were explicitly excluded. The study cohort was female patients with CeD and HTN, DM, and HLD. Cohorts were propensity score matched for age, race, ethnicity, tobacco use, hemoglobin A1c, and ASCVD risk factors (systolic and diastolic blood pressure, cholesterol levels, use of anti-hypertensives, amongst prior characteristics mentioned).
Outcomes of interest were summative and individual CVD outcomes from the following: percutaneous coronary intervention (PCI) and stenting, stroke, angina, myocardial infarction (MI), and coronary artery bypass graft (CABG). The CVD risk was calculated by risk difference through TriNetX’s statistical analysis.
Results: When comparing female control to female study CeD cohorts, there were no statistically significant differences in CVD outcomes other than angina. Females with CeD had significantly greater risk of angina pectoris or unstable angina than female control (6.5% vs. 5.6%, P=0.024).
In comparing male control to female CeD cohort, male control cohort had significantly greater summative CVD (30.8% vs. 23.4%, P< 0.0001), PCI (1.1% vs. 0.6%, P=0.0007), MI (11.6% vs. 9.8%, P=0.0004), and CABG risk (17.9% vs. 9.8%, P< 0.0001).
Discussion: While the female CeD only had greater risk of angina compared to the female control group, this study was limited by the ability to control for variability in adherence to a gluten-free diet. Ultimately, CeD demonstrated minimally increased CVD risk in females, adding to the mixed results in this field.
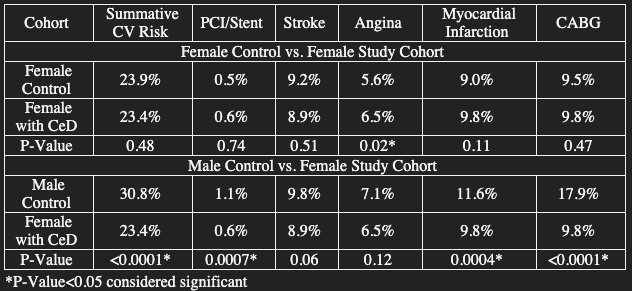
Figure: Table 1. Cardiovascular outcome comparisons in celiac disease cohorts
Disclosures:
Joy Zhao indicated no relevant financial relationships.
Jason Lin indicated no relevant financial relationships.
John Lin indicated no relevant financial relationships.
Stephanie Moleski indicated no relevant financial relationships.
Joy Zhao, MD1, Jason Lin, MD2, John Lin, BS3, Stephanie Moleski, MD1. P4071 - Sex Differences in Cardiovascular Risk in Patients With Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Thomas Jefferson University, Philadelphia, PA; 2University of Texas at Houston, Houston, TX; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA
Introduction: Cardiovascular disease (CVD) is a leading cause of death in women, but female sex is protective against poor cardiovascular outcomes. Additionally, the atherosclerotic cardiovascular disease (ASCVD) calculator does not account for autoimmune disease in its assessment.
Although studies show that individuals with celiac disease (CeD) exhibit a modestly elevated risk of cardiovascular disease, no studies have specifically investigated the cardiovascular risk among females with celiac disease in comparison to both male and female control cohorts. This study seeks to address that gap.
Methods: Using TriNetX, a research database with millions of de-identified patient information, a multi-center retrospective cohort analysis was performed. Control cohorts were male or female patients >18 years old with hypertension (HTN), diabetes mellitus (DM), and hyperlipidemia (HLD). Autoimmune diseases like psoriasis, systemic lupus erythematosus (SLE), ulcerative colitis (UC), Crohn's disease (CD), and CeD were explicitly excluded. The study cohort was female patients with CeD and HTN, DM, and HLD. Cohorts were propensity score matched for age, race, ethnicity, tobacco use, hemoglobin A1c, and ASCVD risk factors (systolic and diastolic blood pressure, cholesterol levels, use of anti-hypertensives, amongst prior characteristics mentioned).
Outcomes of interest were summative and individual CVD outcomes from the following: percutaneous coronary intervention (PCI) and stenting, stroke, angina, myocardial infarction (MI), and coronary artery bypass graft (CABG). The CVD risk was calculated by risk difference through TriNetX’s statistical analysis.
Results: When comparing female control to female study CeD cohorts, there were no statistically significant differences in CVD outcomes other than angina. Females with CeD had significantly greater risk of angina pectoris or unstable angina than female control (6.5% vs. 5.6%, P=0.024).
In comparing male control to female CeD cohort, male control cohort had significantly greater summative CVD (30.8% vs. 23.4%, P< 0.0001), PCI (1.1% vs. 0.6%, P=0.0007), MI (11.6% vs. 9.8%, P=0.0004), and CABG risk (17.9% vs. 9.8%, P< 0.0001).
Discussion: While the female CeD only had greater risk of angina compared to the female control group, this study was limited by the ability to control for variability in adherence to a gluten-free diet. Ultimately, CeD demonstrated minimally increased CVD risk in females, adding to the mixed results in this field.
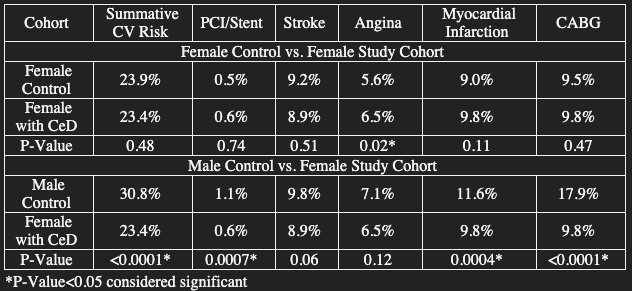
Figure: Table 1. Cardiovascular outcome comparisons in celiac disease cohorts
Disclosures:
Joy Zhao indicated no relevant financial relationships.
Jason Lin indicated no relevant financial relationships.
John Lin indicated no relevant financial relationships.
Stephanie Moleski indicated no relevant financial relationships.
Joy Zhao, MD1, Jason Lin, MD2, John Lin, BS3, Stephanie Moleski, MD1. P4071 - Sex Differences in Cardiovascular Risk in Patients With Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
