Monday Poster Session
Category: Small Intestine
P4069 - Osteoporosis Screening in Patients with Celiac Disease, Inflammatory Bowel Disease, and Dual Diagnosis: A Retrospective Chart Review
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexandria Markley, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Alexandria Markley, MD1, Luis Rendon Rodriguez, MD2, Swati Patel, MD2, Carlos G. Diola, MD3, Yontan Israel, MD3, Christopher Cao, MD3
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Patients with celiac disease (CeD) and inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are at increased risk for low bone mineral density (BMD) and osteoporosis due to chronic inflammation, malabsorption, and corticosteroid use. Current guidelines recommend BMD screening in celiac patients and certain IBD patients, but adherence to screening practices remains suboptimal. It is unclear whether a dual diagnosis of CeD+IBD further compounds osteoporosis risk, and screening practices in this subgroup are not well characterized.
Methods: We conducted a retrospective chart review of patients with CeD, IBD (CD or UC), or both, who received care at a tertiary care center. Collected data included demographics, diagnosis type, and dual-energy X-ray absorptiometry (DEXA) scan history. The primary outcomes were DEXA screening rates and prevalence of osteoporosis and osteopenia among those screened.
Results: A total of 336 patients were included (n = 84 per group). Mean age differed significantly (p = 0.0004), with UC patients being the oldest (mean 43.3 years) and those with a dual diagnosis of CeD+IBD being the youngest (mean 32.2 years). Sex distribution also varied (p = 0.005), with CD and UC groups having more males (56% and 54%), and CeD and CeD+IBD groups having more females (68% and 60%). Racial distribution had a predominance of white individuals in all groups. BMI differed by group (p = 0.0008), CeD group had the highest mean BMI (24.3) and the CD group the lowest (21.1). Overall, DEXA screening rates were low, ranging from 14% to 32%, with significant differences between groups (p = 0.0038). Patients with CeD were more likely to have screening compared to those with IBD or a dual diagnosis. Among those screened, rates of decreased bone mineral density were comparable between the CeD cohort (48%) and dual diagnosis CeD+IBD cohort (46%) (p=.92).
Discussion: Rates of osteoporosis screening were low in all cohorts. While DEXA is recommended in certain IBD patients with specific risk factors, corticosteroid use, chronic active inflammation, or malnutrition, bone density scanning is recommended for all patients with celiac disease. Patients with a dual diagnosis of CeD+IBD have similar rates of decreased BMD compared to patients with a sole diagnosis of CeD. Given the high prevalence of low bone mineral density in these populations, timely screening and intervention are essential to reduce fracture risk and improve long-term outcomes.
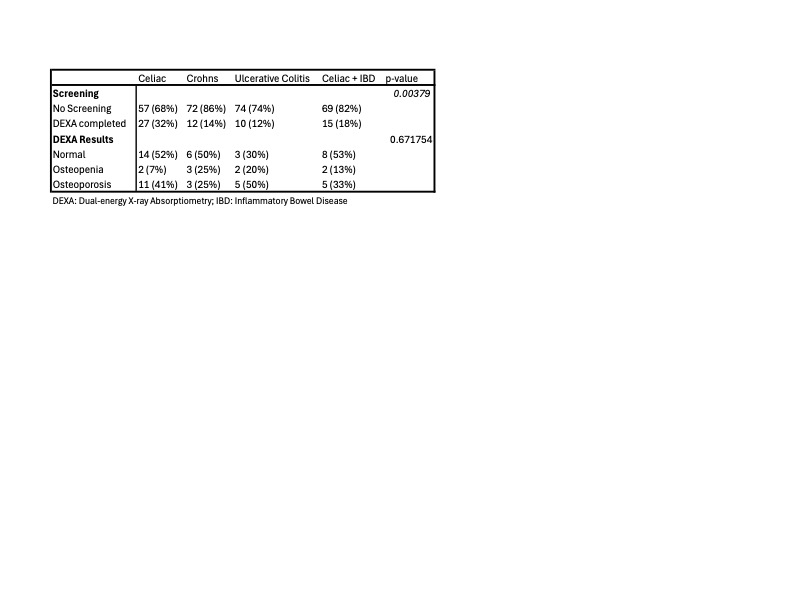
Figure: Table 1. Demographic and Clinical Characteristics of Patients with CeD, CD, UC, and CeD+IBD
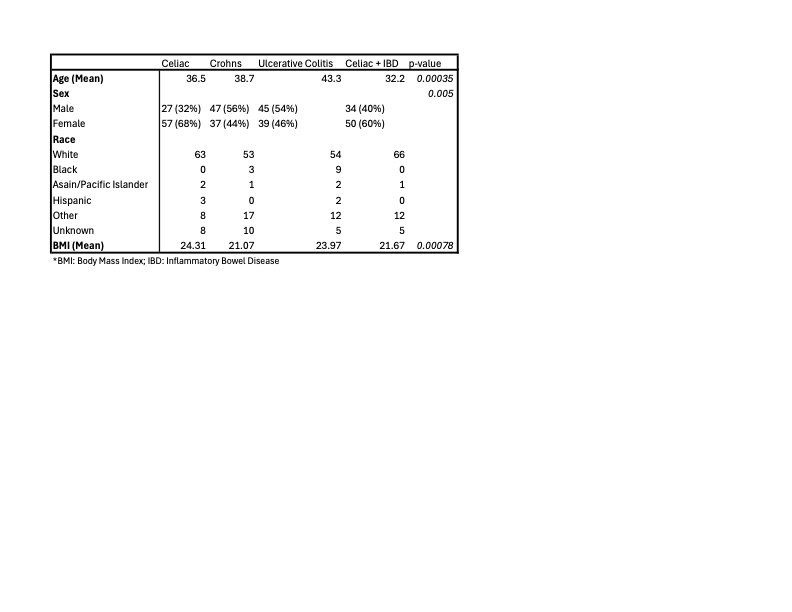
Figure: Table 2. Comparison of Osteoporosis Screening and Bone Density Findings Among Patients with CeD, IBD, and Dual Diagnosis
Disclosures:
Alexandria Markley indicated no relevant financial relationships.
Luis Rendon Rodriguez indicated no relevant financial relationships.
Swati Patel indicated no relevant financial relationships.
Carlos Diola indicated no relevant financial relationships.
Yontan Israel indicated no relevant financial relationships.
Christopher Cao indicated no relevant financial relationships.
Alexandria Markley, MD1, Luis Rendon Rodriguez, MD2, Swati Patel, MD2, Carlos G. Diola, MD3, Yontan Israel, MD3, Christopher Cao, MD3. P4069 - Osteoporosis Screening in Patients with Celiac Disease, Inflammatory Bowel Disease, and Dual Diagnosis: A Retrospective Chart Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Patients with celiac disease (CeD) and inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are at increased risk for low bone mineral density (BMD) and osteoporosis due to chronic inflammation, malabsorption, and corticosteroid use. Current guidelines recommend BMD screening in celiac patients and certain IBD patients, but adherence to screening practices remains suboptimal. It is unclear whether a dual diagnosis of CeD+IBD further compounds osteoporosis risk, and screening practices in this subgroup are not well characterized.
Methods: We conducted a retrospective chart review of patients with CeD, IBD (CD or UC), or both, who received care at a tertiary care center. Collected data included demographics, diagnosis type, and dual-energy X-ray absorptiometry (DEXA) scan history. The primary outcomes were DEXA screening rates and prevalence of osteoporosis and osteopenia among those screened.
Results: A total of 336 patients were included (n = 84 per group). Mean age differed significantly (p = 0.0004), with UC patients being the oldest (mean 43.3 years) and those with a dual diagnosis of CeD+IBD being the youngest (mean 32.2 years). Sex distribution also varied (p = 0.005), with CD and UC groups having more males (56% and 54%), and CeD and CeD+IBD groups having more females (68% and 60%). Racial distribution had a predominance of white individuals in all groups. BMI differed by group (p = 0.0008), CeD group had the highest mean BMI (24.3) and the CD group the lowest (21.1). Overall, DEXA screening rates were low, ranging from 14% to 32%, with significant differences between groups (p = 0.0038). Patients with CeD were more likely to have screening compared to those with IBD or a dual diagnosis. Among those screened, rates of decreased bone mineral density were comparable between the CeD cohort (48%) and dual diagnosis CeD+IBD cohort (46%) (p=.92).
Discussion: Rates of osteoporosis screening were low in all cohorts. While DEXA is recommended in certain IBD patients with specific risk factors, corticosteroid use, chronic active inflammation, or malnutrition, bone density scanning is recommended for all patients with celiac disease. Patients with a dual diagnosis of CeD+IBD have similar rates of decreased BMD compared to patients with a sole diagnosis of CeD. Given the high prevalence of low bone mineral density in these populations, timely screening and intervention are essential to reduce fracture risk and improve long-term outcomes.
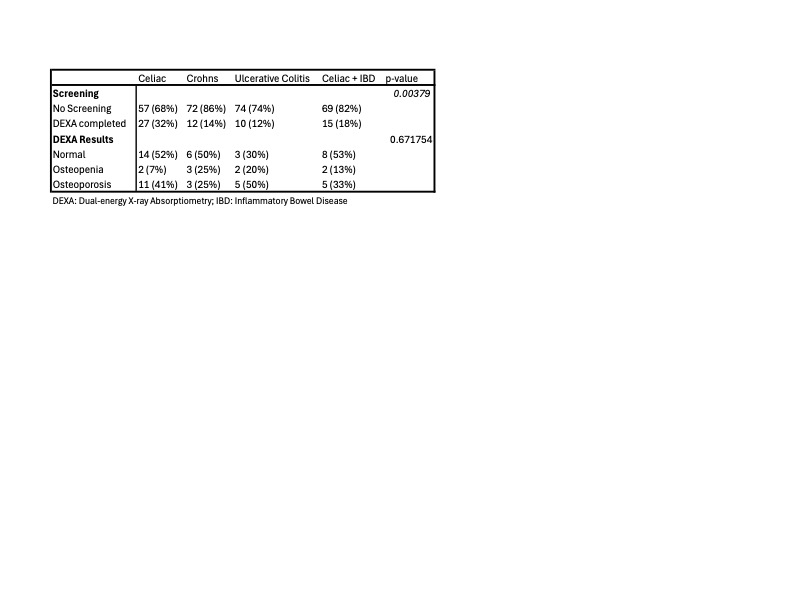
Figure: Table 1. Demographic and Clinical Characteristics of Patients with CeD, CD, UC, and CeD+IBD
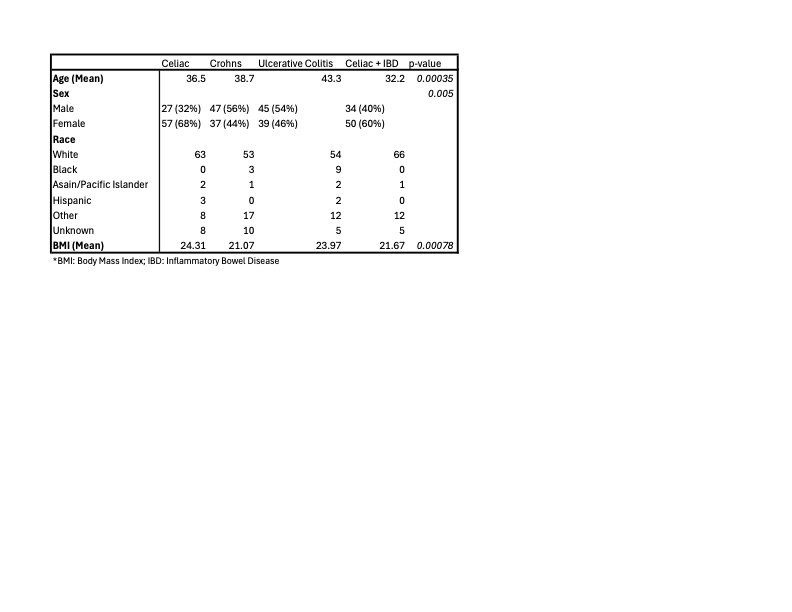
Figure: Table 2. Comparison of Osteoporosis Screening and Bone Density Findings Among Patients with CeD, IBD, and Dual Diagnosis
Disclosures:
Alexandria Markley indicated no relevant financial relationships.
Luis Rendon Rodriguez indicated no relevant financial relationships.
Swati Patel indicated no relevant financial relationships.
Carlos Diola indicated no relevant financial relationships.
Yontan Israel indicated no relevant financial relationships.
Christopher Cao indicated no relevant financial relationships.
Alexandria Markley, MD1, Luis Rendon Rodriguez, MD2, Swati Patel, MD2, Carlos G. Diola, MD3, Yontan Israel, MD3, Christopher Cao, MD3. P4069 - Osteoporosis Screening in Patients with Celiac Disease, Inflammatory Bowel Disease, and Dual Diagnosis: A Retrospective Chart Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
