Monday Poster Session
Category: Small Intestine
P4068 - Risk of Cardiovascular Disease in Patients With Celiac Disease: A Retrospective Propensity-Matched Analysis of Subgroup Populations
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Swapnil Patel, DO
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Swapnil Patel, DO, Shannon Dalessio, MA, Kofi Clarke, MD
Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy triggered by gluten ingestion in genetically susceptible individuals. Previous reports indicate a potential association between CD and cardiovascular disease (CVD). However, the data is limited and lacks detail on subgroup populations and additional risk factors. This study aims to evaluate subgroup risks and additional metabolic risk factors.
Methods: A retrospective cohort study utilizing the TriNetX US Collaborative Network, comprising de-identified data from over 129 million patients across 71 U.S. healthcare organizations. Patients with CD (ICD-10 K90.0) diagnosed from 2006 to 2014 were included if the diagnosis appeared at least twice with additional criteria of endoscopy with biopsy, dermatitis herpetiformis, and/or positive celiac-specific serologies/genetic markers. Patients with prior CVD were excluded. Two cohorts were defined: Group 1 comprising patients identified as Hispanic/Latino, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, Asian, or Black/African American, and Group 2 consisting of non-Hispanic White patients. Propensity score matching (PSM) was performed for age, sex, and risk factors for CVD (hypertension, hyperlipidemia (HLD), diabetes mellitus (DM), tobacco use, chronic kidney disease, and obesity (BMI >30)). To allow for any confounding factors for lead in time, CVD outcomes (Table 1) were assessed 5 –10 years following initial CD diagnosis. Analyses were conducted using TriNetX’s integrated analytics platform.
Results: A total of 362 patients were identified in each group after PSM. There were no differences in CVD outcomes between the two groups (Table 2). There was a higher risk for Type II DM and HLD in Group 1 (Table 2).
Discussion: Our study did not show any significant differences in major CVD outcomes in different population subgroups 5–10 years after CD diagnosis. However, minority patients had higher rates of key CVD risk factors, including Type II DM and HLD. While short and intermediate term follow up indicate no differences, the differences in metabolic risk factors for CVD may contribute to long-term risk. These findings highlight the importance of metabolic screening and culturally targeted dietary strategies for CD management. Further research is needed to determine best approaches to early risk factor management and gluten free dietary adherence in culturally diverse populations with CD to help reduce risk of longer-term CVD.
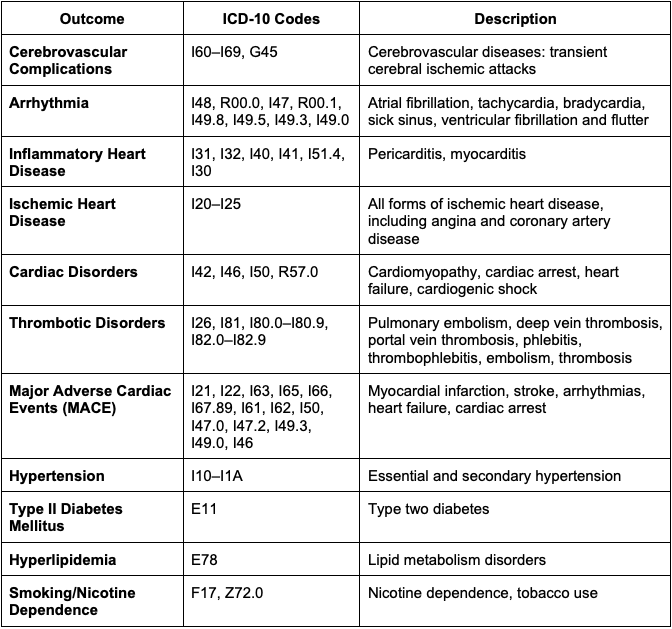
Figure: Table 1. Cardiovascular Outcome Definitions and ICD-10 Codes
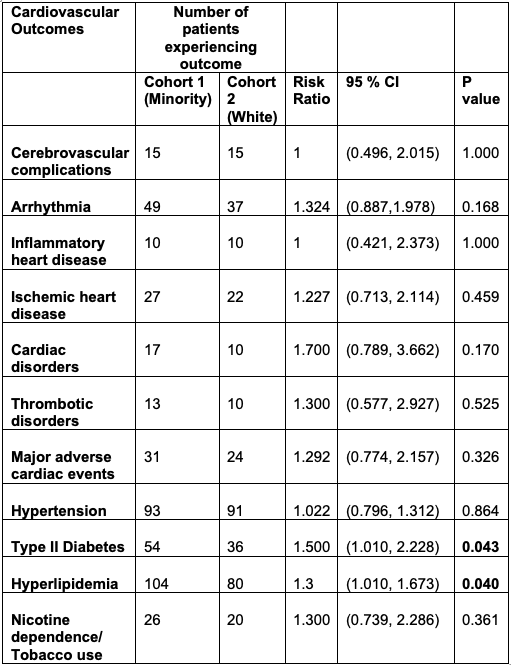
Figure: Table 2. Cardiovascular Outcomes by Population Group in Patients with Celiac Disease (5–10 Years Post-Diagnosis)
Disclosures:
Swapnil Patel indicated no relevant financial relationships.
Shannon Dalessio indicated no relevant financial relationships.
Kofi Clarke: Takeda – Clinical Trial Support.
Swapnil Patel, DO, Shannon Dalessio, MA, Kofi Clarke, MD. P4068 - Risk of Cardiovascular Disease in Patients With Celiac Disease: A Retrospective Propensity-Matched Analysis of Subgroup Populations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy triggered by gluten ingestion in genetically susceptible individuals. Previous reports indicate a potential association between CD and cardiovascular disease (CVD). However, the data is limited and lacks detail on subgroup populations and additional risk factors. This study aims to evaluate subgroup risks and additional metabolic risk factors.
Methods: A retrospective cohort study utilizing the TriNetX US Collaborative Network, comprising de-identified data from over 129 million patients across 71 U.S. healthcare organizations. Patients with CD (ICD-10 K90.0) diagnosed from 2006 to 2014 were included if the diagnosis appeared at least twice with additional criteria of endoscopy with biopsy, dermatitis herpetiformis, and/or positive celiac-specific serologies/genetic markers. Patients with prior CVD were excluded. Two cohorts were defined: Group 1 comprising patients identified as Hispanic/Latino, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, Asian, or Black/African American, and Group 2 consisting of non-Hispanic White patients. Propensity score matching (PSM) was performed for age, sex, and risk factors for CVD (hypertension, hyperlipidemia (HLD), diabetes mellitus (DM), tobacco use, chronic kidney disease, and obesity (BMI >30)). To allow for any confounding factors for lead in time, CVD outcomes (Table 1) were assessed 5 –10 years following initial CD diagnosis. Analyses were conducted using TriNetX’s integrated analytics platform.
Results: A total of 362 patients were identified in each group after PSM. There were no differences in CVD outcomes between the two groups (Table 2). There was a higher risk for Type II DM and HLD in Group 1 (Table 2).
Discussion: Our study did not show any significant differences in major CVD outcomes in different population subgroups 5–10 years after CD diagnosis. However, minority patients had higher rates of key CVD risk factors, including Type II DM and HLD. While short and intermediate term follow up indicate no differences, the differences in metabolic risk factors for CVD may contribute to long-term risk. These findings highlight the importance of metabolic screening and culturally targeted dietary strategies for CD management. Further research is needed to determine best approaches to early risk factor management and gluten free dietary adherence in culturally diverse populations with CD to help reduce risk of longer-term CVD.
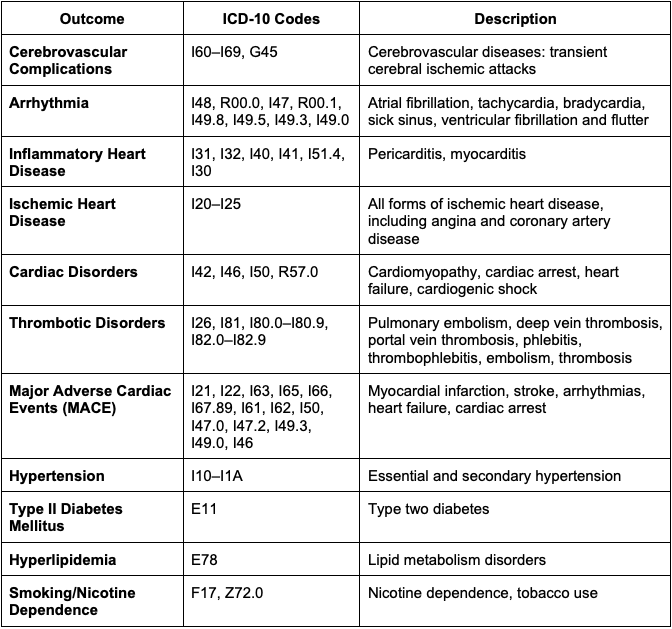
Figure: Table 1. Cardiovascular Outcome Definitions and ICD-10 Codes
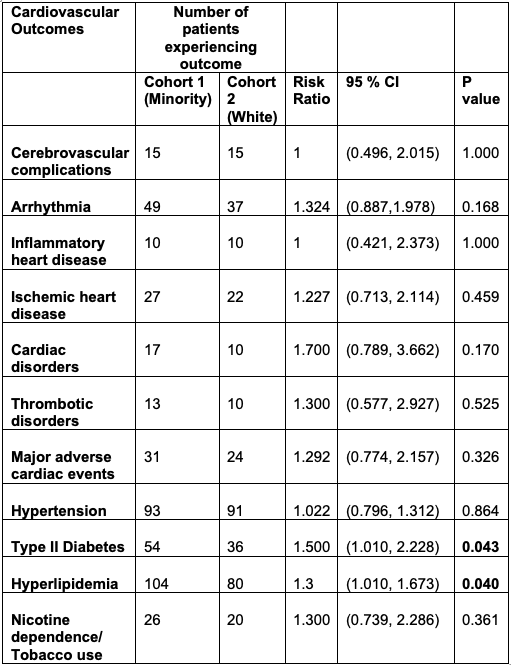
Figure: Table 2. Cardiovascular Outcomes by Population Group in Patients with Celiac Disease (5–10 Years Post-Diagnosis)
Disclosures:
Swapnil Patel indicated no relevant financial relationships.
Shannon Dalessio indicated no relevant financial relationships.
Kofi Clarke: Takeda – Clinical Trial Support.
Swapnil Patel, DO, Shannon Dalessio, MA, Kofi Clarke, MD. P4068 - Risk of Cardiovascular Disease in Patients With Celiac Disease: A Retrospective Propensity-Matched Analysis of Subgroup Populations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

