Monday Poster Session
Category: Small Intestine
P4056 - Under-Recognized and Underdiagnosed: Isolated Enteritis in Immune Checkpoint Inhibitor Therapy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SW
Sharada Wali, MBBS, MPH (she/her/hers)
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Sharada Wali, MBBS, MPH1, Rohan Ahuja, MD2, Maria Julia M. N.. Santos, MD3, Sean Ngo, 4, Tanvi Gupta, MD5, Carolina Cruz, MD1, Kian Abdul-Baki, DO6, Yinghong Wang, MD, PhD, MS1
1University of Texas MD Anderson Cancer Center, Houston, TX; 2University of Texas at Houston, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4University of Texas Health, Houston, TX; 5University of Texas Health Science Center, Houston, TX; 6University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Immune check point inhibitors (ICI) have marked a breakthrough in cancer treatment by harnessing the immune system to target tumors. While ICI-induced colitis is well studied, isolated enteritis (IME) without colonic involvement remains underrecognized. This study aims to define the clinical, endoscopic, and histologic features of isolated enteritis and assess its diagnostic patterns, risk factors, and outcomes.
Methods: The study analyzed adult patients with malignancies treated with ICIs who developed IME confirmed through symptoms, endoscopy, and histology during or after ICI therapy were included. Duodenitis and ileitis subgroups were compared.
Results: Of 20,991 ICI-treated patients, only 30 (0.143%) developed IME. Median age at ICI start was 69.5 years (IQR: 51–73.7); Symptoms include nausea (66.7%), and vomiting (46.7%) and diarrhea (53.3%). Among those with diarrhea (n=16), 62.5% had CTCAE grade ≥2. Diarrhea occurred in 100% of ileitis vs 50% of duodenitis cases. Jejunitis was rare but could be undetected due to less routine practice for jejunal biopsy. Median calprotectin was highest in duodenitis + ileitis (median: 1335.5 μg/g), followed by ileitis alone (319 μg/g), and duodenitis alone (78 μg/g). Endoscopy showed non-ulcerative inflammation (62.1%), ulcers (20%), or was normal (20%). Hospitalization was longer in ileitis+dudenitis (median: 13.5 days) vs duodenitis alone (6.5 days). Isolated Ileitis and combined cases more often required steroids and additional immunosuppressants, while duodenitis alone responded to supportive care (PPI’s, H2 blockers, ondansetron) without immunosuppressants. Remission was higher in ileitis+ duodenitis about 100%, ileitis (66.7%) than duodenitis (58.4%), and ICI therapy was resumed in 12.5%, only among those with isolated duodenitis. Complications (fistula formation) occurred in 10%; all-cause mortality was 36.7% as last follow up.
Discussion: Isolated enteritis is rare, most frequently found in the duodenum, followed by the ileum, although this could be confounded by the sampling error and discretion of endoscopists for small bowel biopsy. Calprotectin can be more reliably reflect ileitis severity, but not duodenitis. Duodenal, jejunal and ileal exam during EGD and colonoscopy is essential when evaluating general GI symptoms. Expanding the knowledge on IME will help to achieve early recognition, better management, and improved outcomes of this under-recognized irAE.
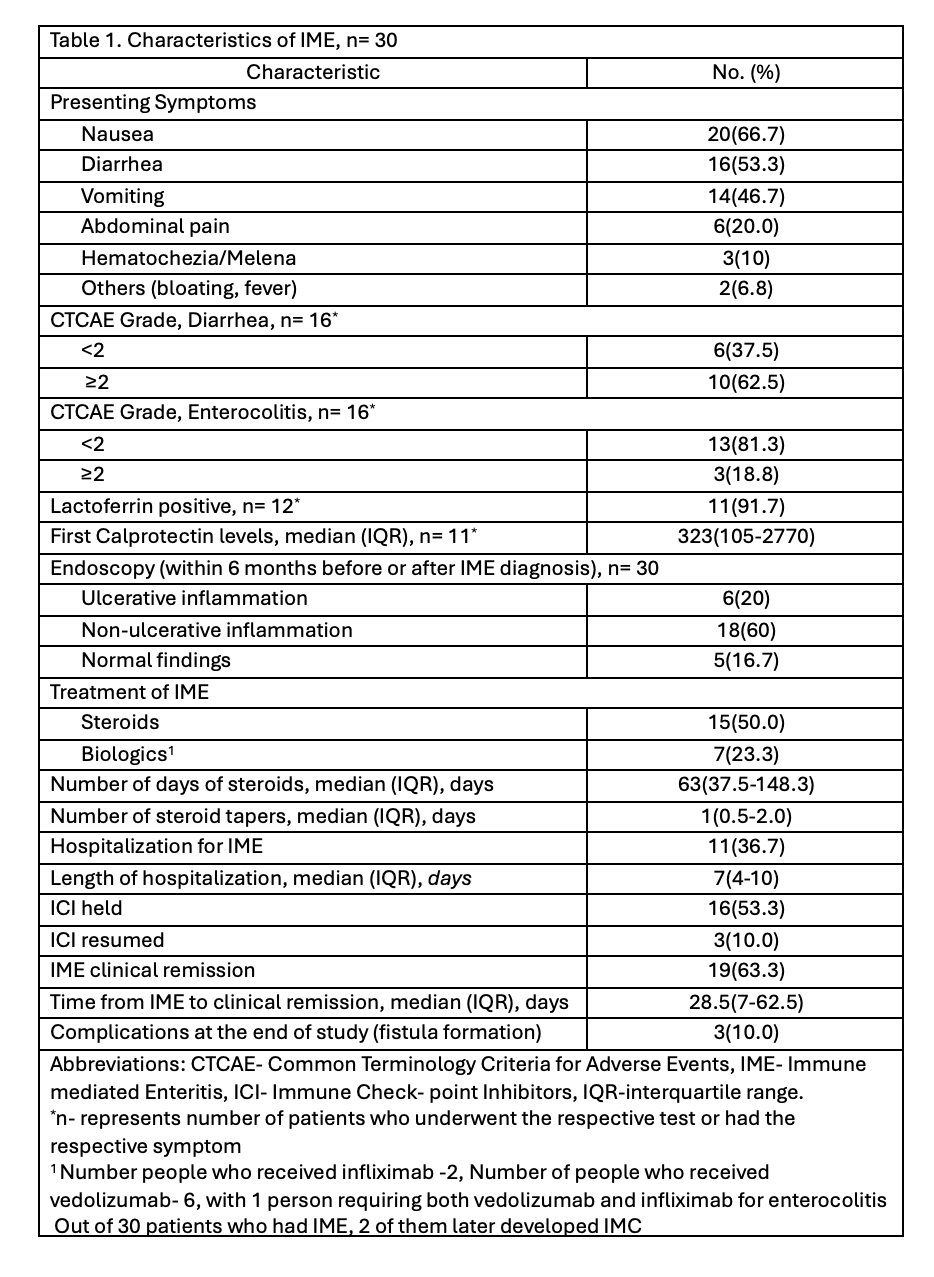
Figure: Table 1. Characteristics of IME, n= 30
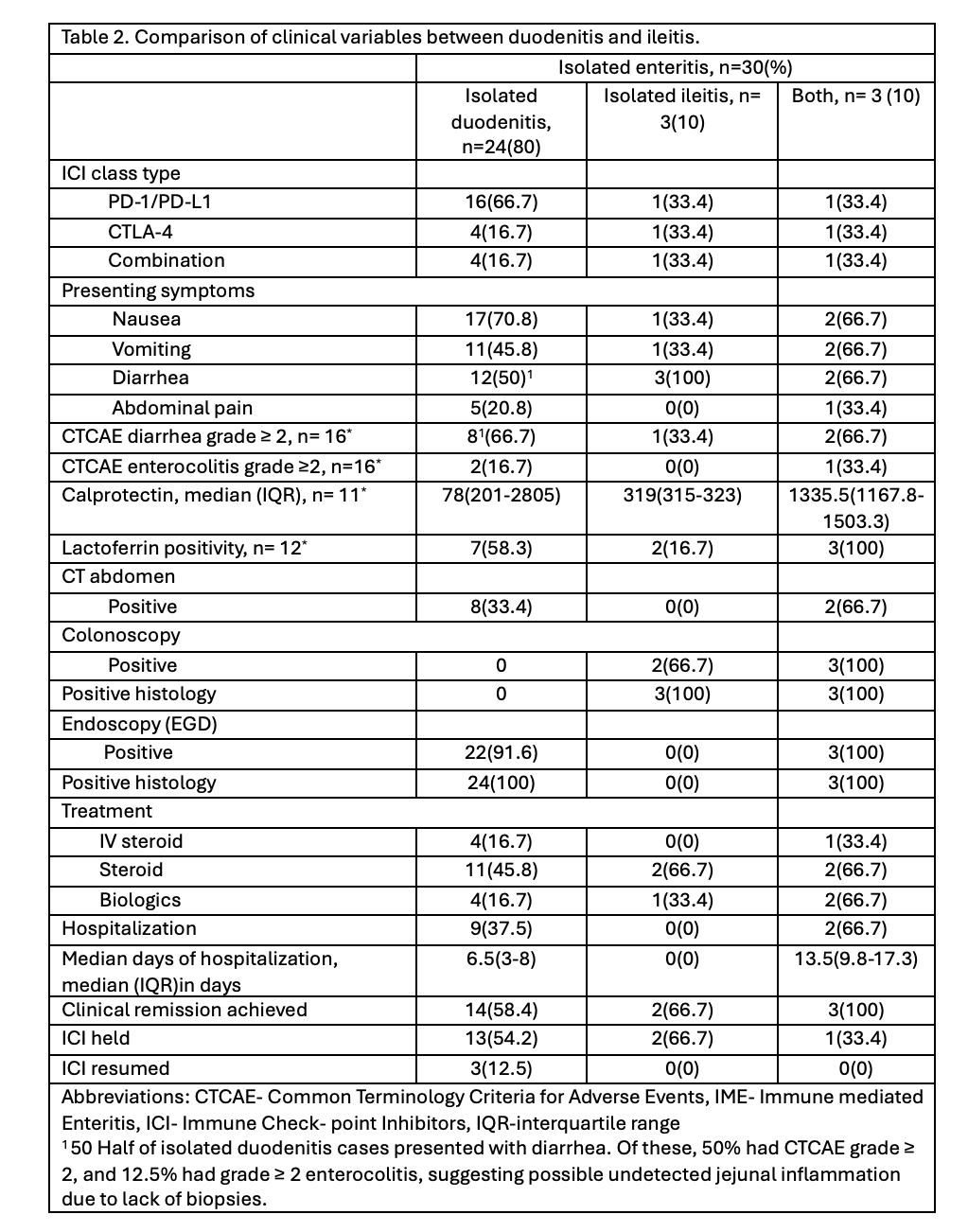
Figure: Table 2. Comparison of clinical variables between duodenitis and ileitis.
Disclosures:
Sharada Wali indicated no relevant financial relationships.
Rohan Ahuja indicated no relevant financial relationships.
Maria Julia Santos indicated no relevant financial relationships.
Sean Ngo indicated no relevant financial relationships.
Tanvi Gupta indicated no relevant financial relationships.
Carolina Cruz indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Yinghong Wang indicated no relevant financial relationships.
Sharada Wali, MBBS, MPH1, Rohan Ahuja, MD2, Maria Julia M. N.. Santos, MD3, Sean Ngo, 4, Tanvi Gupta, MD5, Carolina Cruz, MD1, Kian Abdul-Baki, DO6, Yinghong Wang, MD, PhD, MS1. P4056 - Under-Recognized and Underdiagnosed: Isolated Enteritis in Immune Checkpoint Inhibitor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2University of Texas at Houston, Houston, TX; 3MD Anderson Cancer Center, Houston, TX; 4University of Texas Health, Houston, TX; 5University of Texas Health Science Center, Houston, TX; 6University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Immune check point inhibitors (ICI) have marked a breakthrough in cancer treatment by harnessing the immune system to target tumors. While ICI-induced colitis is well studied, isolated enteritis (IME) without colonic involvement remains underrecognized. This study aims to define the clinical, endoscopic, and histologic features of isolated enteritis and assess its diagnostic patterns, risk factors, and outcomes.
Methods: The study analyzed adult patients with malignancies treated with ICIs who developed IME confirmed through symptoms, endoscopy, and histology during or after ICI therapy were included. Duodenitis and ileitis subgroups were compared.
Results: Of 20,991 ICI-treated patients, only 30 (0.143%) developed IME. Median age at ICI start was 69.5 years (IQR: 51–73.7); Symptoms include nausea (66.7%), and vomiting (46.7%) and diarrhea (53.3%). Among those with diarrhea (n=16), 62.5% had CTCAE grade ≥2. Diarrhea occurred in 100% of ileitis vs 50% of duodenitis cases. Jejunitis was rare but could be undetected due to less routine practice for jejunal biopsy. Median calprotectin was highest in duodenitis + ileitis (median: 1335.5 μg/g), followed by ileitis alone (319 μg/g), and duodenitis alone (78 μg/g). Endoscopy showed non-ulcerative inflammation (62.1%), ulcers (20%), or was normal (20%). Hospitalization was longer in ileitis+dudenitis (median: 13.5 days) vs duodenitis alone (6.5 days). Isolated Ileitis and combined cases more often required steroids and additional immunosuppressants, while duodenitis alone responded to supportive care (PPI’s, H2 blockers, ondansetron) without immunosuppressants. Remission was higher in ileitis+ duodenitis about 100%, ileitis (66.7%) than duodenitis (58.4%), and ICI therapy was resumed in 12.5%, only among those with isolated duodenitis. Complications (fistula formation) occurred in 10%; all-cause mortality was 36.7% as last follow up.
Discussion: Isolated enteritis is rare, most frequently found in the duodenum, followed by the ileum, although this could be confounded by the sampling error and discretion of endoscopists for small bowel biopsy. Calprotectin can be more reliably reflect ileitis severity, but not duodenitis. Duodenal, jejunal and ileal exam during EGD and colonoscopy is essential when evaluating general GI symptoms. Expanding the knowledge on IME will help to achieve early recognition, better management, and improved outcomes of this under-recognized irAE.
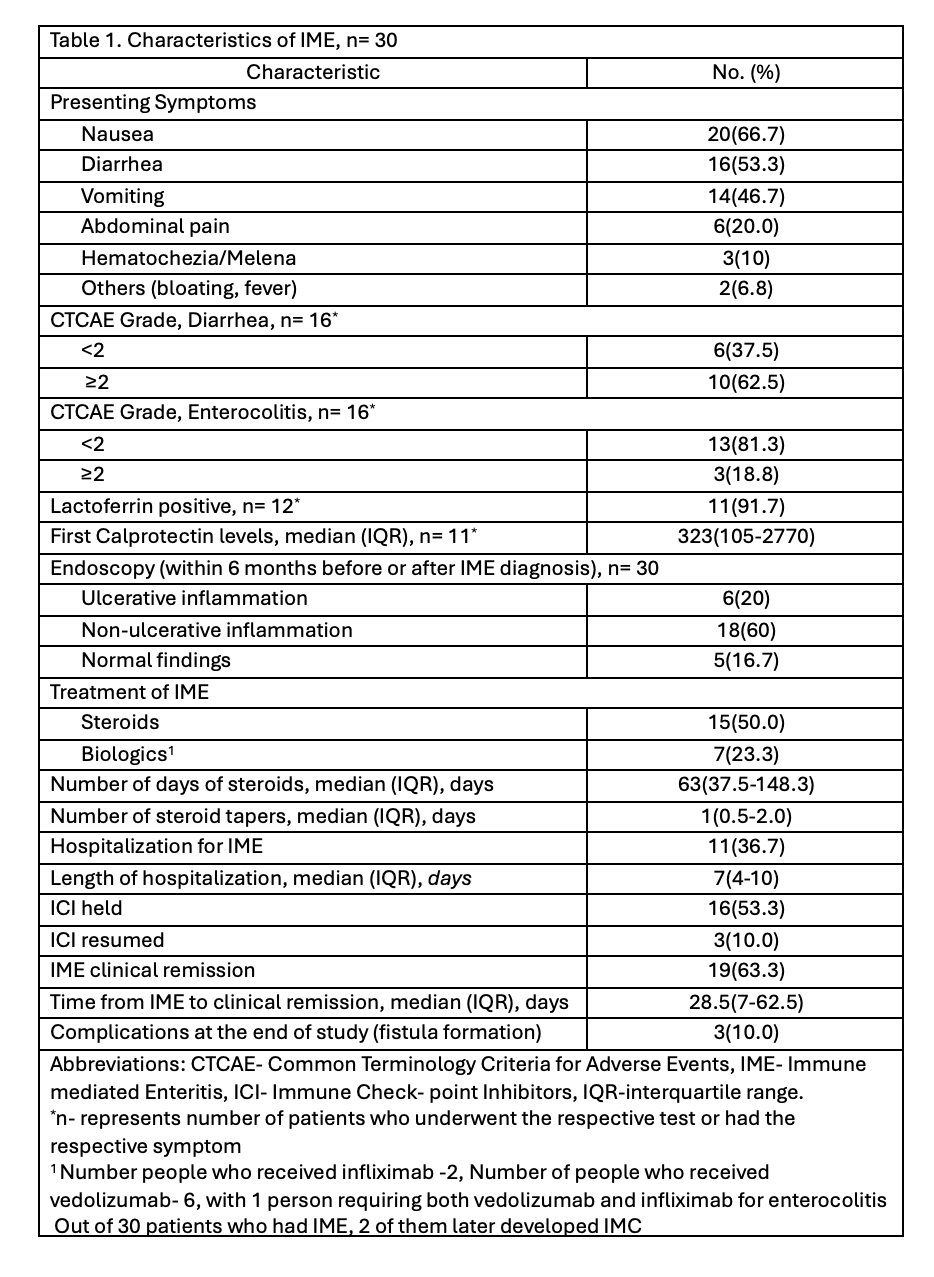
Figure: Table 1. Characteristics of IME, n= 30
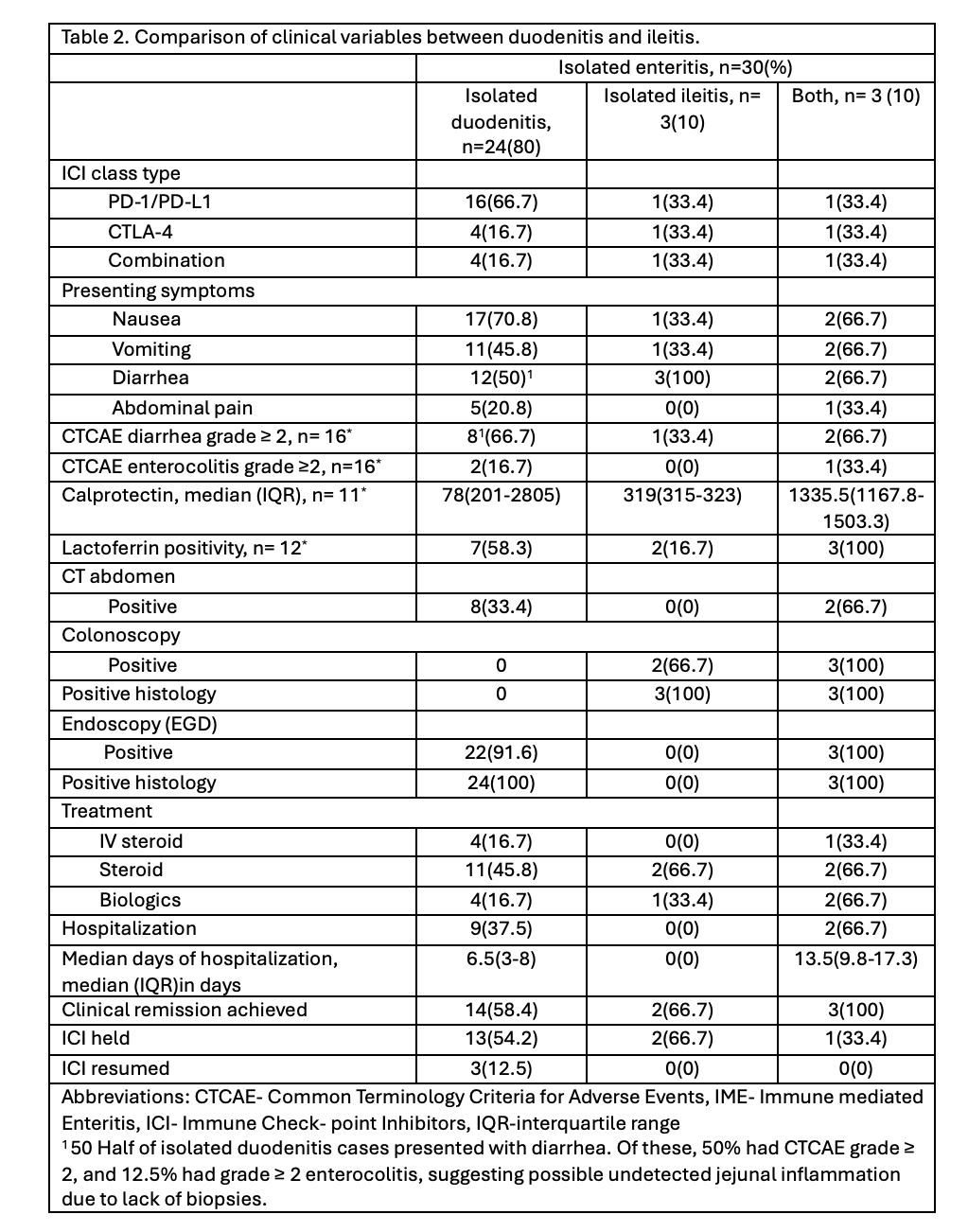
Figure: Table 2. Comparison of clinical variables between duodenitis and ileitis.
Disclosures:
Sharada Wali indicated no relevant financial relationships.
Rohan Ahuja indicated no relevant financial relationships.
Maria Julia Santos indicated no relevant financial relationships.
Sean Ngo indicated no relevant financial relationships.
Tanvi Gupta indicated no relevant financial relationships.
Carolina Cruz indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Yinghong Wang indicated no relevant financial relationships.
Sharada Wali, MBBS, MPH1, Rohan Ahuja, MD2, Maria Julia M. N.. Santos, MD3, Sean Ngo, 4, Tanvi Gupta, MD5, Carolina Cruz, MD1, Kian Abdul-Baki, DO6, Yinghong Wang, MD, PhD, MS1. P4056 - Under-Recognized and Underdiagnosed: Isolated Enteritis in Immune Checkpoint Inhibitor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
