Monday Poster Session
Category: Small Intestine
P4036 - Trends and Disparities in Small Intestinal Carcinoma Mortality in the United States Between 1999-2020
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SB
Siddidha Bokka, MD
Metropolitan University College of Medicine
Torrance, CA
Presenting Author(s)
Dhruv Gandhi, MD1, Siddidha Bokka, MD2, Wajdan Ahmad, MD3, Ayesha Cheema, MBBS3, Hareesha Rishab Bharadwaj, 4, Hassam Ali, MD5, Saqr Alsakarneh, MD, MSc6, Omar Al Ta’ani, MD7, Fariha Hasan, MD8, Sneh Sonaiya, MD, MPH, MBA9, Sheza Malik, MD10, Dushyant S. Dahiya, MD11, Syed Hasham Ali, MD12, Farhan Gohar, MD13
1St Francis Medical Center, Monroe, LA, Mumbai, Maharashtra, India; 2Metropolitan University College of Medicine, Torrance, CA; 3Al-Tibri Medical College, Karachi, Sindh, Pakistan; 4The University of Manchester, Manchester, England, United Kingdom; 5East Carolina University/Brody School of Medicine, Greenville, NC; 6Mayo Clinic, Rochester, MN; 7Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 8Cooper University Hospital, Camden, NJ; 9Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 10Emory University, Atlanta, GA; 11University of Kansas School of Medicine, Kansas City, KS; 12Dow University of Health Sciences, Karachi, Punjab, Pakistan; 13Royal Stoke University Hospital, Staffordshire, England, United Kingdom
Introduction: To determine the trends and disparities in small intestinal carcinoma mortality in American adults older than 45 years between 1999-2020.
Methods: Retrospective analysis of Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research database was performed. For small intestinal carcinoma, International Classification of Diseases-10 code C17 was employed. Age-adjusted mortality rates(AAMR) and crude death rates(CDR) per 100,000 persons were determined. Average annual percentage change(AAPC) was determined using Joinpoint regression. Temporal trends were analyzed in sex, race, geographical distribution and patient age-related mortality.
Results: A total of 27,320 deaths from small intestinal carcinoma were reported. AAMRs declined slightly from 1.02 to 0.96 between 1999-2013(AAPC:-0.08;p=0.75) followed by a steady increase from 0.96 to 1.21 between 2013-2020(AAPC:3.25;p< 0.001), resulting in overall AAMR of 1.05(AAPC:1.02;p< 0.001). Males had higher AAMR(1.28) as compared to females(0.85) and both showed a similar increase in mortality(male AAPC:0.73;p=0.019 and female AAPC:0.73;p=0.1). Among races, non-Hispanic(NH) Blacks had the highest AAMR(1.72), followed by NH Whites(1.05), NH American Indians/Alaskan Natives(0.81), Hispanics(0.75), NH Asian/Pacific Islanders(0.7). All races saw an increase in AAMR, with the greatest increase seen in NH Blacks(AAPC:1.49;p< 0.001). Geographically, AAMRs were highest in Midwest(1.12) followed by Northeast(1.07). All census regions saw an increase in AAMR, with the greatest increase seen for South(AAPC:1.12;p=0.015). Metropolitan areas showed disproportionately higher mortality(AAMR:1.07) in comparison to nonmetropolitan areas(AAMR:1.02). Additionally, they showed a greater increase in AAMR(AAPC:1.08;p=0.001) than nonmetropolitan areas(AAPC:0.57;p=0.29). Of the 10-year age groups, CDR was highest for 85+ years(3.61). All age groups saw an increase in CDR except 45-54 years which saw a decline(AAPC:-1.63;p=0.031). The greatest increase was seen for 85+ years(AAPC:1.73;p< 0.001).
Discussion: We found a significant increase in small intestinal carcinoma mortality, though persistent disparities exist. Males, NH Blacks, residents of Midwest and metropolitan areas experienced disproportionately higher mortality rates. While all demographics saw an increase in AAMR from 1999-2020, those aged 45-54 years saw a decline. These findings identify critical areas for targeted public health interventions.
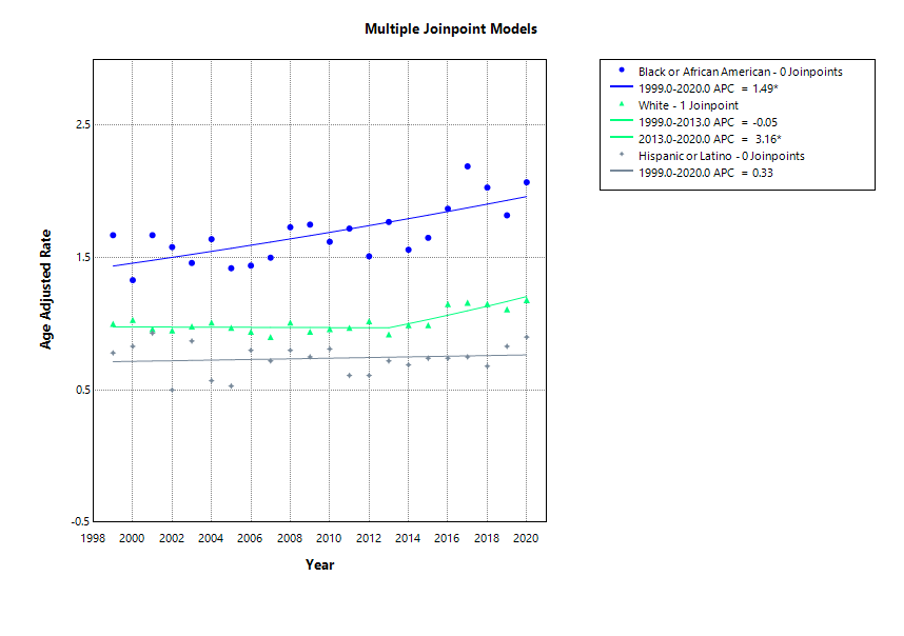
Figure: Trends based on Race
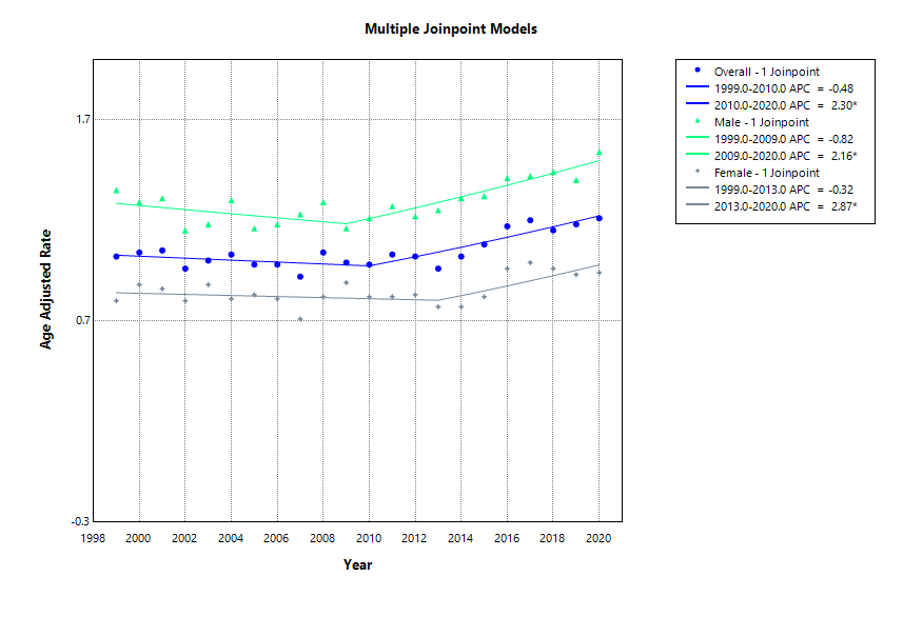
Figure: Trends based on Gender
Disclosures:
Dhruv Gandhi indicated no relevant financial relationships.
Siddidha Bokka indicated no relevant financial relationships.
Wajdan Ahmad indicated no relevant financial relationships.
Ayesha Cheema indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Fariha Hasan indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Sheza Malik indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Syed Hasham Ali indicated no relevant financial relationships.
Farhan Gohar indicated no relevant financial relationships.
Dhruv Gandhi, MD1, Siddidha Bokka, MD2, Wajdan Ahmad, MD3, Ayesha Cheema, MBBS3, Hareesha Rishab Bharadwaj, 4, Hassam Ali, MD5, Saqr Alsakarneh, MD, MSc6, Omar Al Ta’ani, MD7, Fariha Hasan, MD8, Sneh Sonaiya, MD, MPH, MBA9, Sheza Malik, MD10, Dushyant S. Dahiya, MD11, Syed Hasham Ali, MD12, Farhan Gohar, MD13. P4036 - Trends and Disparities in Small Intestinal Carcinoma Mortality in the United States Between 1999-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St Francis Medical Center, Monroe, LA, Mumbai, Maharashtra, India; 2Metropolitan University College of Medicine, Torrance, CA; 3Al-Tibri Medical College, Karachi, Sindh, Pakistan; 4The University of Manchester, Manchester, England, United Kingdom; 5East Carolina University/Brody School of Medicine, Greenville, NC; 6Mayo Clinic, Rochester, MN; 7Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 8Cooper University Hospital, Camden, NJ; 9Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 10Emory University, Atlanta, GA; 11University of Kansas School of Medicine, Kansas City, KS; 12Dow University of Health Sciences, Karachi, Punjab, Pakistan; 13Royal Stoke University Hospital, Staffordshire, England, United Kingdom
Introduction: To determine the trends and disparities in small intestinal carcinoma mortality in American adults older than 45 years between 1999-2020.
Methods: Retrospective analysis of Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research database was performed. For small intestinal carcinoma, International Classification of Diseases-10 code C17 was employed. Age-adjusted mortality rates(AAMR) and crude death rates(CDR) per 100,000 persons were determined. Average annual percentage change(AAPC) was determined using Joinpoint regression. Temporal trends were analyzed in sex, race, geographical distribution and patient age-related mortality.
Results: A total of 27,320 deaths from small intestinal carcinoma were reported. AAMRs declined slightly from 1.02 to 0.96 between 1999-2013(AAPC:-0.08;p=0.75) followed by a steady increase from 0.96 to 1.21 between 2013-2020(AAPC:3.25;p< 0.001), resulting in overall AAMR of 1.05(AAPC:1.02;p< 0.001). Males had higher AAMR(1.28) as compared to females(0.85) and both showed a similar increase in mortality(male AAPC:0.73;p=0.019 and female AAPC:0.73;p=0.1). Among races, non-Hispanic(NH) Blacks had the highest AAMR(1.72), followed by NH Whites(1.05), NH American Indians/Alaskan Natives(0.81), Hispanics(0.75), NH Asian/Pacific Islanders(0.7). All races saw an increase in AAMR, with the greatest increase seen in NH Blacks(AAPC:1.49;p< 0.001). Geographically, AAMRs were highest in Midwest(1.12) followed by Northeast(1.07). All census regions saw an increase in AAMR, with the greatest increase seen for South(AAPC:1.12;p=0.015). Metropolitan areas showed disproportionately higher mortality(AAMR:1.07) in comparison to nonmetropolitan areas(AAMR:1.02). Additionally, they showed a greater increase in AAMR(AAPC:1.08;p=0.001) than nonmetropolitan areas(AAPC:0.57;p=0.29). Of the 10-year age groups, CDR was highest for 85+ years(3.61). All age groups saw an increase in CDR except 45-54 years which saw a decline(AAPC:-1.63;p=0.031). The greatest increase was seen for 85+ years(AAPC:1.73;p< 0.001).
Discussion: We found a significant increase in small intestinal carcinoma mortality, though persistent disparities exist. Males, NH Blacks, residents of Midwest and metropolitan areas experienced disproportionately higher mortality rates. While all demographics saw an increase in AAMR from 1999-2020, those aged 45-54 years saw a decline. These findings identify critical areas for targeted public health interventions.
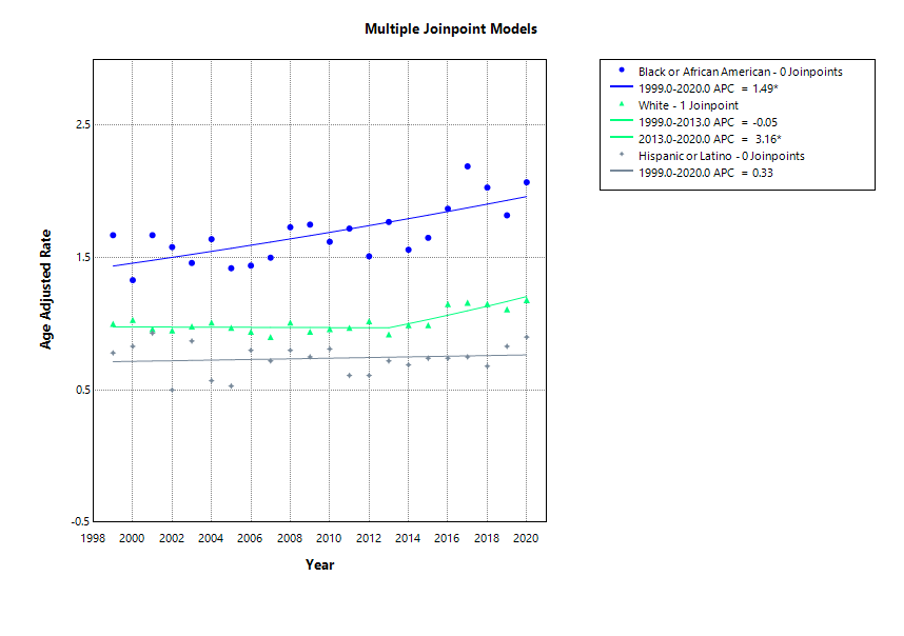
Figure: Trends based on Race
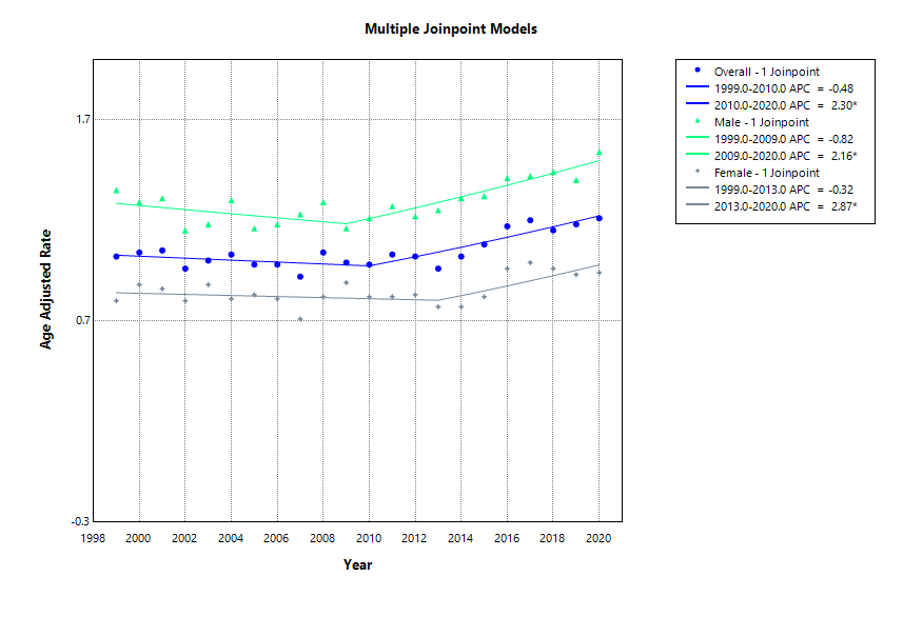
Figure: Trends based on Gender
Disclosures:
Dhruv Gandhi indicated no relevant financial relationships.
Siddidha Bokka indicated no relevant financial relationships.
Wajdan Ahmad indicated no relevant financial relationships.
Ayesha Cheema indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Fariha Hasan indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Sheza Malik indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Syed Hasham Ali indicated no relevant financial relationships.
Farhan Gohar indicated no relevant financial relationships.
Dhruv Gandhi, MD1, Siddidha Bokka, MD2, Wajdan Ahmad, MD3, Ayesha Cheema, MBBS3, Hareesha Rishab Bharadwaj, 4, Hassam Ali, MD5, Saqr Alsakarneh, MD, MSc6, Omar Al Ta’ani, MD7, Fariha Hasan, MD8, Sneh Sonaiya, MD, MPH, MBA9, Sheza Malik, MD10, Dushyant S. Dahiya, MD11, Syed Hasham Ali, MD12, Farhan Gohar, MD13. P4036 - Trends and Disparities in Small Intestinal Carcinoma Mortality in the United States Between 1999-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

