Monday Poster Session
Category: Liver
P4013 - Hepatic Epithelioid Hemangioendothelioma With Multisystem Involvement: Diagnostic and Therapeutic Insights From a Rare Case
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MR
Mawra Rehman, MD
University of Massachusetts Chan Medical School-Baystate Medical Center
Broad Brook, CT
Presenting Author(s)
Mawra Rehman, MD1, Aizaz Khan, MD2, Cristian Garcia-Bardina, MD3, Kathryn Jobbins, DO, MS3
1University of Massachusetts Chan Medical School-Baystate Medical Center, Broad Brook, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3UMass Chan Baystate, Springfield, MA
Introduction: Hepatic epithelioid hemangioendothelioma (HEHE) is a rare vascular malignancy with an estimated incidence of less than 1 per million. Its pathogenesis remains poorly understood, with most cases arising sporadically and in patients without identifiable risk factors. Due to its rarity, optimal management is not well-defined and is largely based on case reports and small series. We present a case of diffuse metastatic HEHE in a previously healthy individual, successfully managed with systemic chemotherapy.
Case Description/
Methods: A 48-year-old woman with no significant medical history presented with acute epigastric pain radiating to the right chest following a recent viral upper respiratory infection. She denied alcohol use, medication exposure, toxic ingestion, or autoimmune symptoms. Labs showed elevated alkaline phosphatase (567 U/L), AST (93 U/L), ALT (93 U/L), and total bilirubin (4.5 mg/dL). Abdominal CT revealed hepatomegaly with multiple large hypodense lesions in both hepatic lobes (largest 10 cm), mass effect on the right portal vein, and a vague 8 mm pancreatic head lesion. Numerous bilateral pulmonary nodules were also identified.
CT chest confirmed widespread peripheral nodular opacities, raising concern for metastatic disease. Ultrasound-guided liver biopsy of a right hepatic lesion revealed sinusoidal infiltration by atypical epithelioid cells within fibromyxoid stroma. Immunohistochemistry was positive for CD31 and ERG, consistent with a malignant vascular neoplasm. CAMTA1 nuclear immunopositivity confirmed the diagnosis of HEHE.
Due to worsening hepatic function and rising bilirubin, systemic chemotherapy with doxorubicin and ifosfamide was initiated. After four cycles, liver enzymes and bilirubin normalized. The case was discussed in a multidisciplinary tumor board, where embolization and transplantation were considered, but the decision was made to continue chemotherapy given clinical improvement.
Discussion: This case underscores the diagnostic and therapeutic challenges of HEHE, particularly in patients without identifiable risk factors. It also demonstrates the potential for systemic chemotherapy to induce meaningful clinical response in multifocal, metastatic disease. As HEHE remains poorly understood, continued case reporting is essential to refine management strategies.
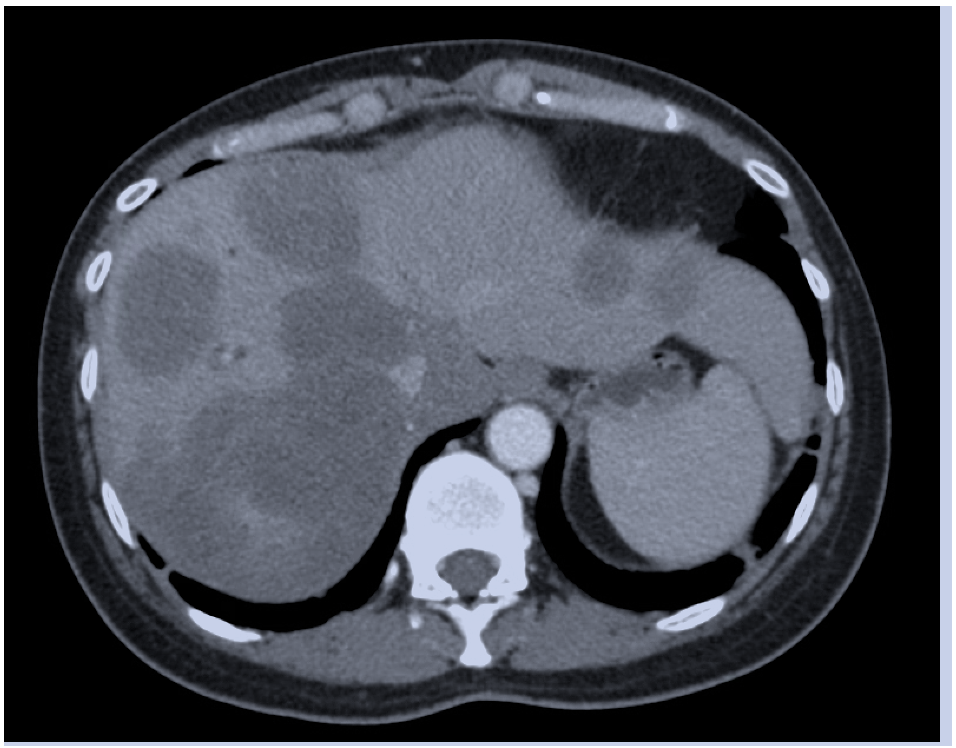
Figure: CT Abdomen axial cut showing multiple hypodense liver lesions
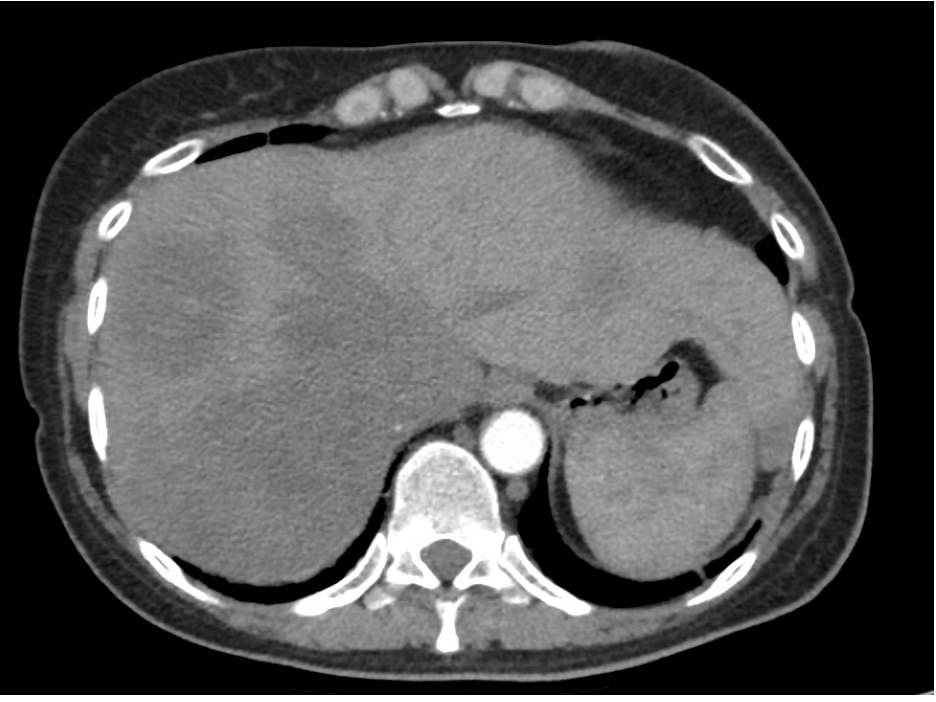
Figure: CT Abdomen axial cut taken post 4 cycles of systemic chemotherapy demonstrating improvement in size and number of liver lesions
Disclosures:
Mawra Rehman indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Cristian Garcia-Bardina indicated no relevant financial relationships.
Kathryn Jobbins indicated no relevant financial relationships.
Mawra Rehman, MD1, Aizaz Khan, MD2, Cristian Garcia-Bardina, MD3, Kathryn Jobbins, DO, MS3. P4013 - Hepatic Epithelioid Hemangioendothelioma With Multisystem Involvement: Diagnostic and Therapeutic Insights From a Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Broad Brook, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3UMass Chan Baystate, Springfield, MA
Introduction: Hepatic epithelioid hemangioendothelioma (HEHE) is a rare vascular malignancy with an estimated incidence of less than 1 per million. Its pathogenesis remains poorly understood, with most cases arising sporadically and in patients without identifiable risk factors. Due to its rarity, optimal management is not well-defined and is largely based on case reports and small series. We present a case of diffuse metastatic HEHE in a previously healthy individual, successfully managed with systemic chemotherapy.
Case Description/
Methods: A 48-year-old woman with no significant medical history presented with acute epigastric pain radiating to the right chest following a recent viral upper respiratory infection. She denied alcohol use, medication exposure, toxic ingestion, or autoimmune symptoms. Labs showed elevated alkaline phosphatase (567 U/L), AST (93 U/L), ALT (93 U/L), and total bilirubin (4.5 mg/dL). Abdominal CT revealed hepatomegaly with multiple large hypodense lesions in both hepatic lobes (largest 10 cm), mass effect on the right portal vein, and a vague 8 mm pancreatic head lesion. Numerous bilateral pulmonary nodules were also identified.
CT chest confirmed widespread peripheral nodular opacities, raising concern for metastatic disease. Ultrasound-guided liver biopsy of a right hepatic lesion revealed sinusoidal infiltration by atypical epithelioid cells within fibromyxoid stroma. Immunohistochemistry was positive for CD31 and ERG, consistent with a malignant vascular neoplasm. CAMTA1 nuclear immunopositivity confirmed the diagnosis of HEHE.
Due to worsening hepatic function and rising bilirubin, systemic chemotherapy with doxorubicin and ifosfamide was initiated. After four cycles, liver enzymes and bilirubin normalized. The case was discussed in a multidisciplinary tumor board, where embolization and transplantation were considered, but the decision was made to continue chemotherapy given clinical improvement.
Discussion: This case underscores the diagnostic and therapeutic challenges of HEHE, particularly in patients without identifiable risk factors. It also demonstrates the potential for systemic chemotherapy to induce meaningful clinical response in multifocal, metastatic disease. As HEHE remains poorly understood, continued case reporting is essential to refine management strategies.
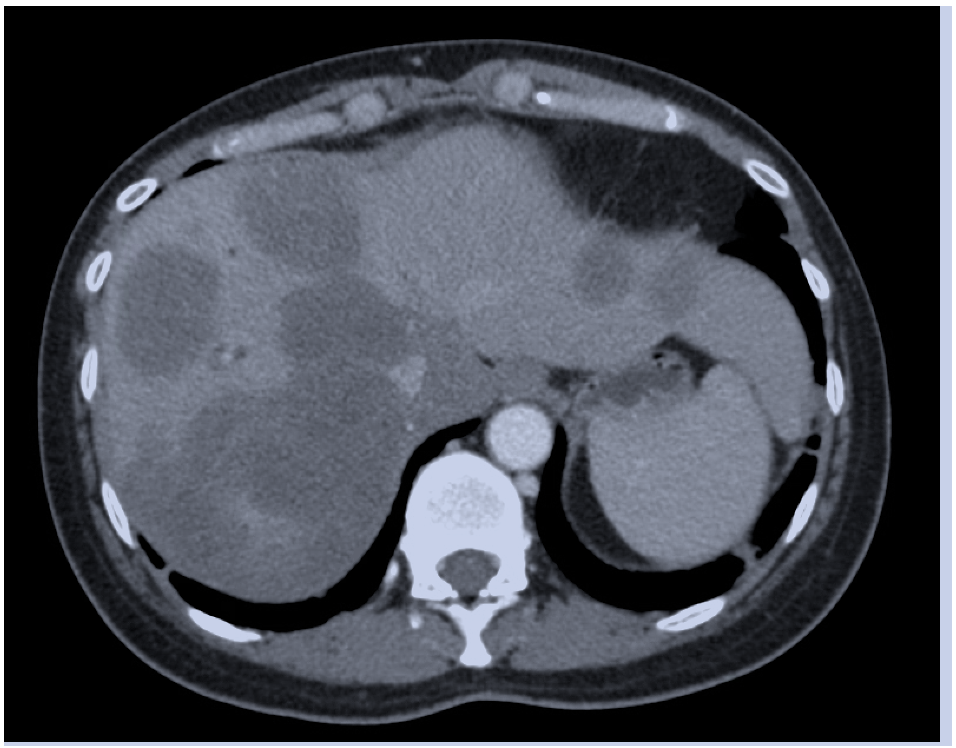
Figure: CT Abdomen axial cut showing multiple hypodense liver lesions
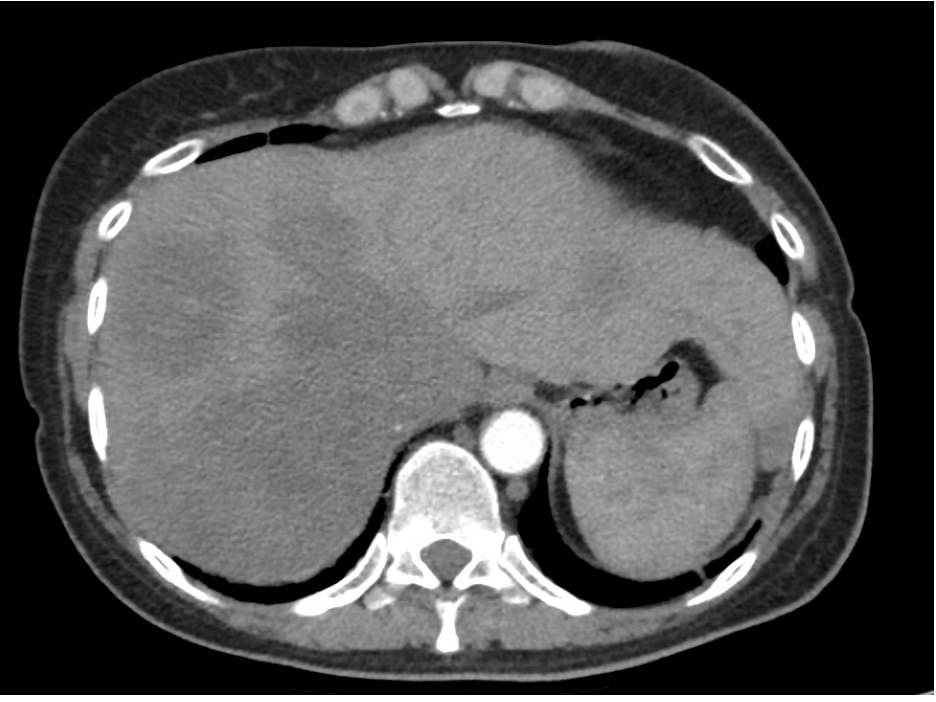
Figure: CT Abdomen axial cut taken post 4 cycles of systemic chemotherapy demonstrating improvement in size and number of liver lesions
Disclosures:
Mawra Rehman indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Cristian Garcia-Bardina indicated no relevant financial relationships.
Kathryn Jobbins indicated no relevant financial relationships.
Mawra Rehman, MD1, Aizaz Khan, MD2, Cristian Garcia-Bardina, MD3, Kathryn Jobbins, DO, MS3. P4013 - Hepatic Epithelioid Hemangioendothelioma With Multisystem Involvement: Diagnostic and Therapeutic Insights From a Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
