Monday Poster Session
Category: Liver
P3999 - Polycystic Kidney and Liver Disease—A Rare Cause of Portal Hypertension
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Anthony Quiej, BA
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Anthony Quiej, BA1, Dalorie Wilson, ARNP2, Yamile Blain, MD2, Patricia D. Jones, MD, MSCR1
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Portal Hypertension (PHT), elevated pressure in the portal venous system, is primarily attributed to cirrhosis. Other pre- and post-hepatic causes of PHT include thrombosis, granulomas, Budd-Chiari syndrome, and congestive heart failure (CHF). There is sparse data on PHT secondary to Polycystic Kidney (PKD) and Liver disease (PLD). Still, advanced cases can cause post-hepatic PHT through hepatic venous outflow obstruction, portal vein obstruction, and/or inferior vena cava syndrome. The prevalence of PHT was estimated at 6% in PLD in a retrospective study of 125 patients but poorly defined in concurrent PKD/PLD. We present a case of PHT in a patient with PKD/PLD and CHF, highlighting unique diagnostic challenges.
Case Description/
Methods: A 56 y.o man with autosomal dominant PKD, PLD, CHF, and ESRD on hemodialysis (6 days per week due to hypotension) presented to the hospital with recurrent abdominal distention requiring semimonthly paracentesis. Abdominal US revealed ascites and hepatic and renal cysts; Hepatology was consulted and recommended a CT scan that demonstrated compression of the hepatic veins and intrahepatic IVC with dilated main portal vein to 1.5 cm. Serologic workup ruled out other intrinsic liver diseases. Serum-Ascites Albumin gradients (SAAG) was 1.54 g/dL and total protein was 2.8 g/dL (Figure 2), consistent with PHT. Treatment options were discussed with the patient; he was not interested in evaluation for transplant and opted to continue serial paracentesis. Given the diffuse nature of the cysts, aspiration would not have improved symptoms. We discussed Pleurx for ascites, but this was not pursued due to the risk of leaking and infection.
Discussion: Mechanical obstruction of portal flow and fluid retention as hepatic cysts expand and exert pressure on vessels may lead to PHT. Ascites is often multifactorial, encompassing cirrhosis, PHT, and other conditions, occurring in 40% of PKD/PLD-associated cases. This patient has multiple potential causes for ascites, including heart failure and ESRD. Elucidating the underlying cause of ascites was essential in forming a treatment plan. A liver biopsy was considered to rule out cirrhosis however, targeting hepatic parenchyma was challenging due to extensive PLD (Figure 1). In cases with a large dominant cyst causing compression, aspiration may ameliorate PHT and ascites. This case contributes to the limited reported instances of PKD/PLD-induced PHT, presenting a diagnostic dilemma and complicated PHT-induced ascites management.
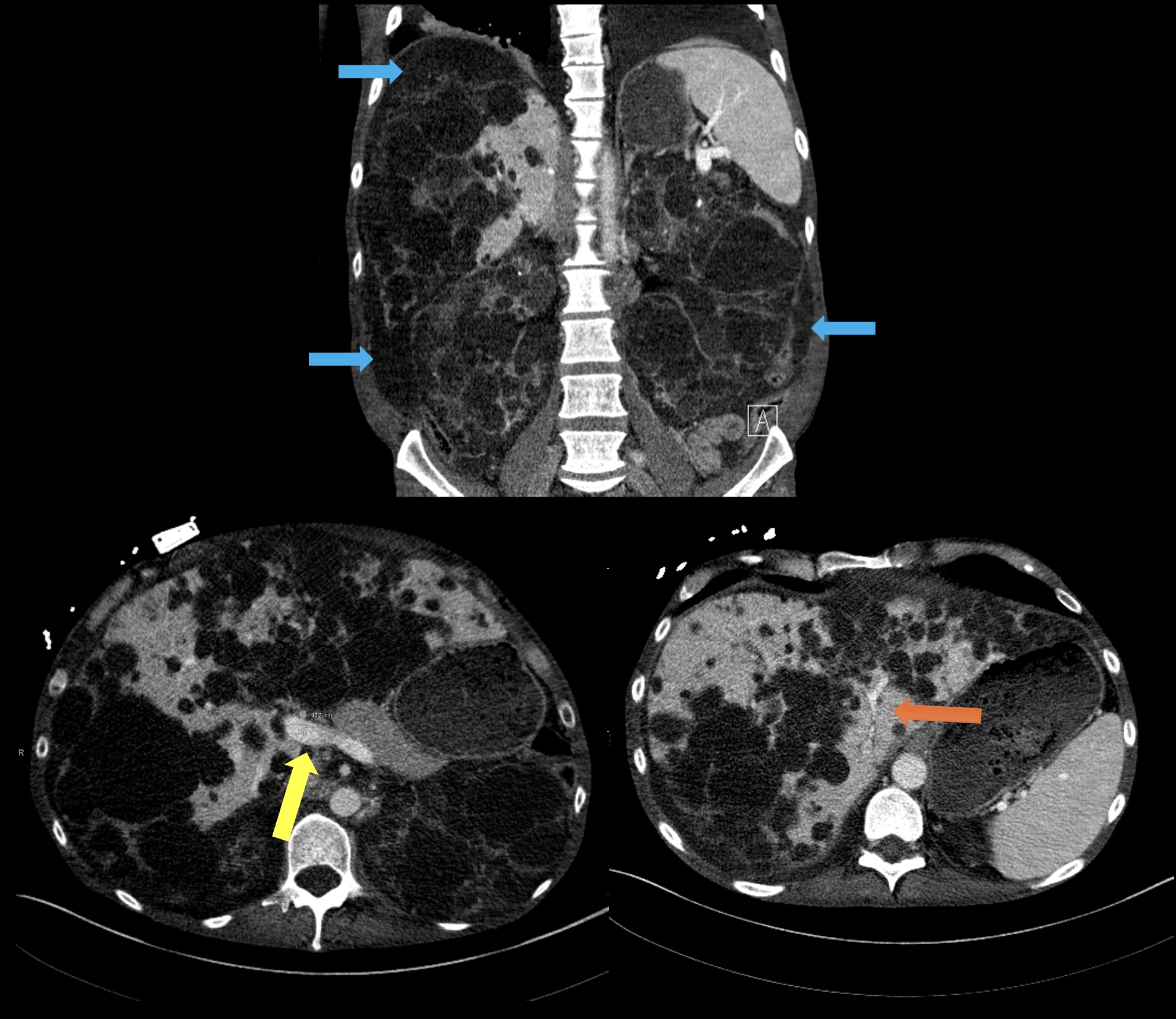
Figure: Figure 1: Triple-phase CT scan with venography. Coronal portal venous (PV) phase CT image shows innumerable cystic lesions throughout the liver and kidneys. Also seen: ascites in bilateral colic gutters and perihepatic region (blue arrows), and bilateral pleural effusions. Axial PV phase CT images show mild dilatation of the main portal vein measuring 15 mm (yellow arrow) and severe compression of the intrahepatic IVC and hepatic veins (orange arrow).

Figure: Figure 2: Laboratory Values. Serologic workup ordered to rule out intrinsic liver diseases. Fluid analysis of ascitic fluid with high SAAG and low total protein, consistent with portal hypertension. Clinically significant labs highlighted in orange.
Disclosures:
Anthony Quiej indicated no relevant financial relationships.
Dalorie Wilson indicated no relevant financial relationships.
Yamile Blain indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Anthony Quiej, BA1, Dalorie Wilson, ARNP2, Yamile Blain, MD2, Patricia D. Jones, MD, MSCR1. P3999 - Polycystic Kidney and Liver Disease—A Rare Cause of Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Portal Hypertension (PHT), elevated pressure in the portal venous system, is primarily attributed to cirrhosis. Other pre- and post-hepatic causes of PHT include thrombosis, granulomas, Budd-Chiari syndrome, and congestive heart failure (CHF). There is sparse data on PHT secondary to Polycystic Kidney (PKD) and Liver disease (PLD). Still, advanced cases can cause post-hepatic PHT through hepatic venous outflow obstruction, portal vein obstruction, and/or inferior vena cava syndrome. The prevalence of PHT was estimated at 6% in PLD in a retrospective study of 125 patients but poorly defined in concurrent PKD/PLD. We present a case of PHT in a patient with PKD/PLD and CHF, highlighting unique diagnostic challenges.
Case Description/
Methods: A 56 y.o man with autosomal dominant PKD, PLD, CHF, and ESRD on hemodialysis (6 days per week due to hypotension) presented to the hospital with recurrent abdominal distention requiring semimonthly paracentesis. Abdominal US revealed ascites and hepatic and renal cysts; Hepatology was consulted and recommended a CT scan that demonstrated compression of the hepatic veins and intrahepatic IVC with dilated main portal vein to 1.5 cm. Serologic workup ruled out other intrinsic liver diseases. Serum-Ascites Albumin gradients (SAAG) was 1.54 g/dL and total protein was 2.8 g/dL (Figure 2), consistent with PHT. Treatment options were discussed with the patient; he was not interested in evaluation for transplant and opted to continue serial paracentesis. Given the diffuse nature of the cysts, aspiration would not have improved symptoms. We discussed Pleurx for ascites, but this was not pursued due to the risk of leaking and infection.
Discussion: Mechanical obstruction of portal flow and fluid retention as hepatic cysts expand and exert pressure on vessels may lead to PHT. Ascites is often multifactorial, encompassing cirrhosis, PHT, and other conditions, occurring in 40% of PKD/PLD-associated cases. This patient has multiple potential causes for ascites, including heart failure and ESRD. Elucidating the underlying cause of ascites was essential in forming a treatment plan. A liver biopsy was considered to rule out cirrhosis however, targeting hepatic parenchyma was challenging due to extensive PLD (Figure 1). In cases with a large dominant cyst causing compression, aspiration may ameliorate PHT and ascites. This case contributes to the limited reported instances of PKD/PLD-induced PHT, presenting a diagnostic dilemma and complicated PHT-induced ascites management.
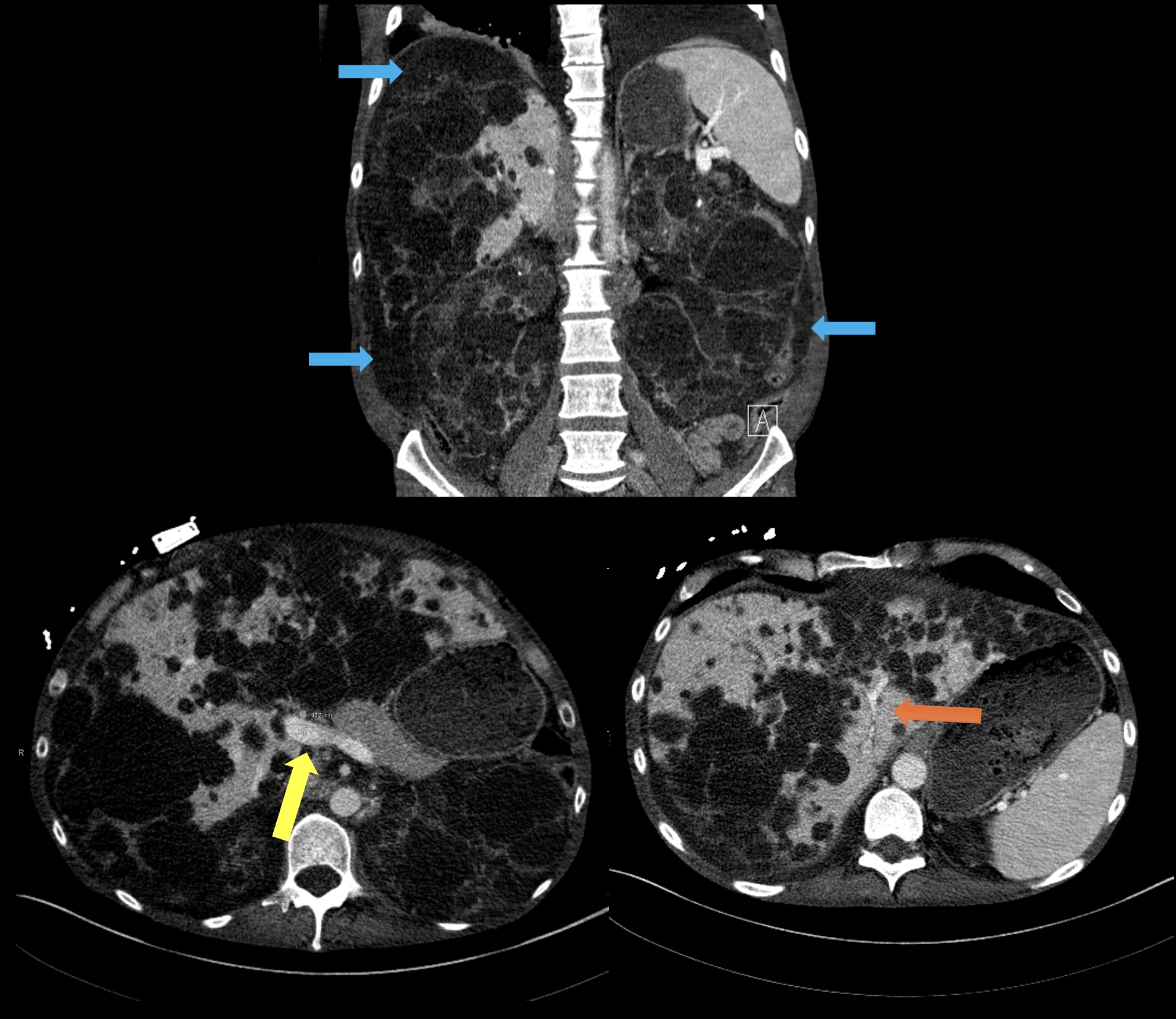
Figure: Figure 1: Triple-phase CT scan with venography. Coronal portal venous (PV) phase CT image shows innumerable cystic lesions throughout the liver and kidneys. Also seen: ascites in bilateral colic gutters and perihepatic region (blue arrows), and bilateral pleural effusions. Axial PV phase CT images show mild dilatation of the main portal vein measuring 15 mm (yellow arrow) and severe compression of the intrahepatic IVC and hepatic veins (orange arrow).

Figure: Figure 2: Laboratory Values. Serologic workup ordered to rule out intrinsic liver diseases. Fluid analysis of ascitic fluid with high SAAG and low total protein, consistent with portal hypertension. Clinically significant labs highlighted in orange.
Disclosures:
Anthony Quiej indicated no relevant financial relationships.
Dalorie Wilson indicated no relevant financial relationships.
Yamile Blain indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Anthony Quiej, BA1, Dalorie Wilson, ARNP2, Yamile Blain, MD2, Patricia D. Jones, MD, MSCR1. P3999 - Polycystic Kidney and Liver Disease—A Rare Cause of Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
