Monday Poster Session
Category: Liver
P3986 - Tacrolimus-Induced Psychosis: A Rare but Morbid Adverse Effect
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anas Aljabi, MD
Virginia Commonwealth University Health System
Richmond, VA
Presenting Author(s)
Anas Aljabi, MD1, Vinay Jahagirdar, MBBS2, Alsiddig Elmahdi, MD1, Brian Davis, MD3
1Virginia Commonwealth University Health System, Richmond, VA; 2Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University Health System, Richmond, VA; 3Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Tacrolimus (Tac) is the first line immune suppressive agent used after liver transplantation (LT). The primary mechanism of action involves inhibition of T-cells via intracellular blockage of calcineurin (CNI), which leads to decrease T-cell synthesis and reduced activation of the adaptive immune system pathways. Tac easily crosses the blood-brain barrier due to its lipophilic structure and common side effects include tremors, headache, blurred vision, paresthesia, insomnia, nausea, vomiting and rare but severe neurological side effects may include encephalopathy, seizure, reversible posterior leukoencephalopathy syndrome (RPLS), or psychosis.
Case Description/
Methods: A 58-year-old man with history of liver transplant secondary to decompensated alcohol-related liver disease 6 months prior to presentation presented to the hospital after a fall. Collateral via family described abnormal behaviors such as paranoia, agitation, and altered mental status. Transplant hepatology, neurology, infectious disease, and psychiatry teams were consulted. The patient underwent Brain Magnetic Resonance Imaging (MRI), electroencephalogram (EEG) and lumbar puncture. Liver function tests were normal and tacrolimus trough levels were at goal level between 4-6 ng/mL. The patient was started on broad spectrum antibiotics without improvement. After a few days of admission, Tacrolimus was switched to Sirolimus per the hepatology team. Each day during the admission, patient neurological status was closely evaluated.
Magnetic Resonance Imaging (MRI) of the brain ruled out RPLS or anatomical disease. Electroencephalogram (EEG) showed slowing brain activity, but no evidence of seizure-like activity. Lumbar puncture was normal. Tacrolimus was discontinued and the patient was switched to a CNI-free regimen of sirolimus and mycophenolate mofetil. The patient’s mental status improved with resolution of visual and auditory hallucinations.
Discussion: Tacrolimus neurotoxicity is common but rare adverse effects such as psychosis should be considered once other etiologies are ruled out. Tacrolimus-related psychosis is idiosyncratic and not necessarily related to serum trough levels. Treatment involves stopping the drug and switching to a CNI-free regimen to maintain intact liver graft synthetic function.
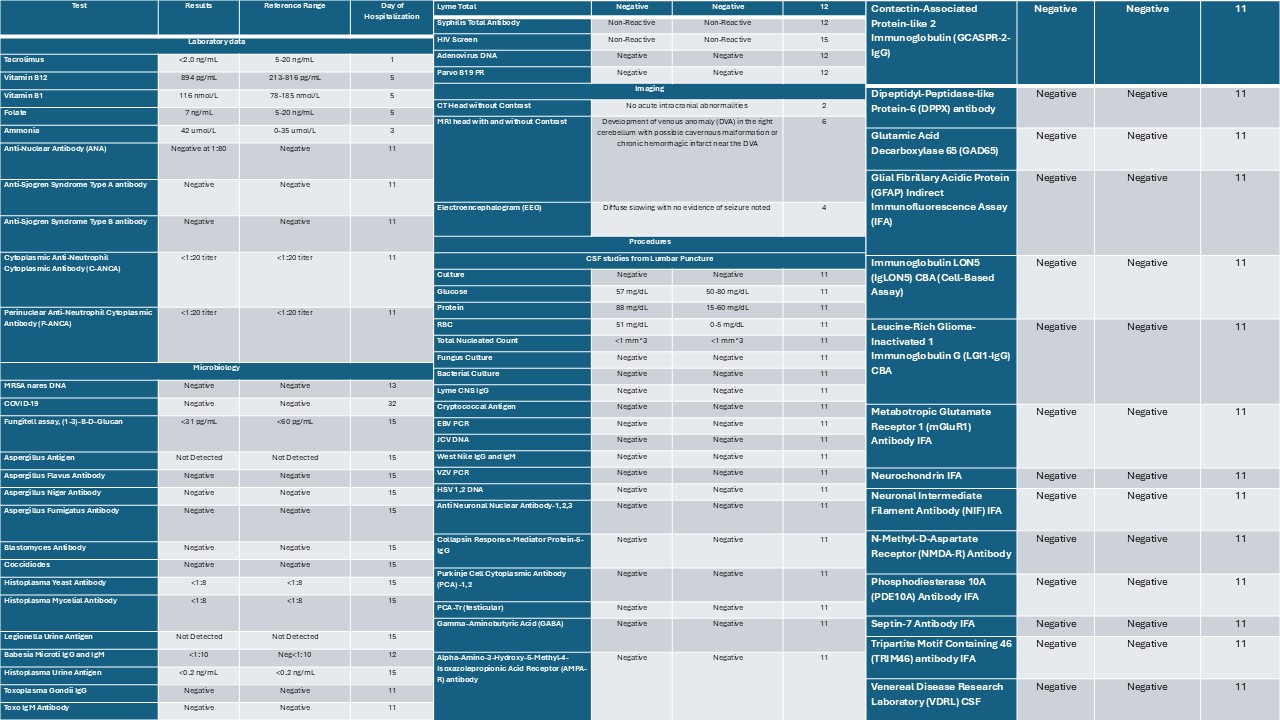
Figure: Table 1. Summary for laboratory, microbiology, imaging and procedural data obtained throughout hospital course
Disclosures:
Anas Aljabi indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Alsiddig Elmahdi indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Anas Aljabi, MD1, Vinay Jahagirdar, MBBS2, Alsiddig Elmahdi, MD1, Brian Davis, MD3. P3986 - Tacrolimus-Induced Psychosis: A Rare but Morbid Adverse Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Richmond, VA; 2Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University Health System, Richmond, VA; 3Medical Director of Liver Transplantation, Hunter Holmes McGuire VA Medical Center, Richmond, VA
Introduction: Tacrolimus (Tac) is the first line immune suppressive agent used after liver transplantation (LT). The primary mechanism of action involves inhibition of T-cells via intracellular blockage of calcineurin (CNI), which leads to decrease T-cell synthesis and reduced activation of the adaptive immune system pathways. Tac easily crosses the blood-brain barrier due to its lipophilic structure and common side effects include tremors, headache, blurred vision, paresthesia, insomnia, nausea, vomiting and rare but severe neurological side effects may include encephalopathy, seizure, reversible posterior leukoencephalopathy syndrome (RPLS), or psychosis.
Case Description/
Methods: A 58-year-old man with history of liver transplant secondary to decompensated alcohol-related liver disease 6 months prior to presentation presented to the hospital after a fall. Collateral via family described abnormal behaviors such as paranoia, agitation, and altered mental status. Transplant hepatology, neurology, infectious disease, and psychiatry teams were consulted. The patient underwent Brain Magnetic Resonance Imaging (MRI), electroencephalogram (EEG) and lumbar puncture. Liver function tests were normal and tacrolimus trough levels were at goal level between 4-6 ng/mL. The patient was started on broad spectrum antibiotics without improvement. After a few days of admission, Tacrolimus was switched to Sirolimus per the hepatology team. Each day during the admission, patient neurological status was closely evaluated.
Magnetic Resonance Imaging (MRI) of the brain ruled out RPLS or anatomical disease. Electroencephalogram (EEG) showed slowing brain activity, but no evidence of seizure-like activity. Lumbar puncture was normal. Tacrolimus was discontinued and the patient was switched to a CNI-free regimen of sirolimus and mycophenolate mofetil. The patient’s mental status improved with resolution of visual and auditory hallucinations.
Discussion: Tacrolimus neurotoxicity is common but rare adverse effects such as psychosis should be considered once other etiologies are ruled out. Tacrolimus-related psychosis is idiosyncratic and not necessarily related to serum trough levels. Treatment involves stopping the drug and switching to a CNI-free regimen to maintain intact liver graft synthetic function.
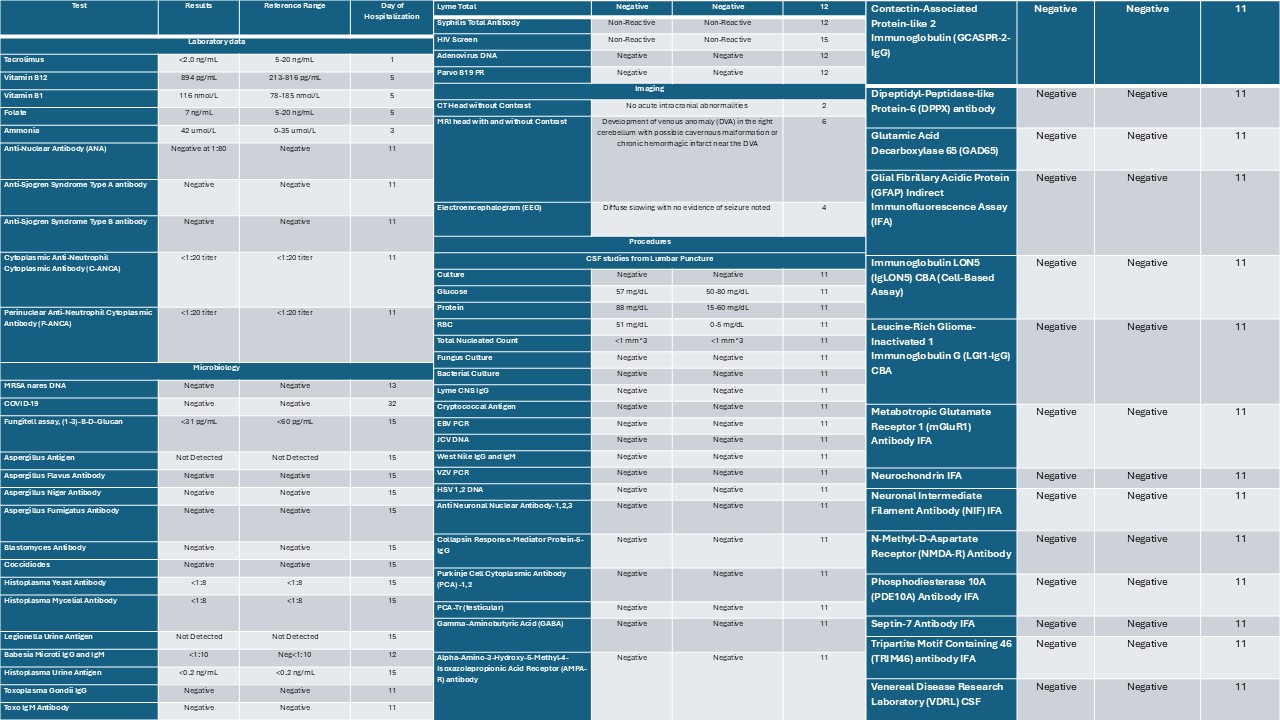
Figure: Table 1. Summary for laboratory, microbiology, imaging and procedural data obtained throughout hospital course
Disclosures:
Anas Aljabi indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Alsiddig Elmahdi indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Anas Aljabi, MD1, Vinay Jahagirdar, MBBS2, Alsiddig Elmahdi, MD1, Brian Davis, MD3. P3986 - Tacrolimus-Induced Psychosis: A Rare but Morbid Adverse Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
