Monday Poster Session
Category: Liver
P3985 - Disguised Malignancy: Acute Myeloid Leukemia Presenting as Decompensated Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Wilfredo J. Javier-Rojas, MD
HCA Florida Blake Hospital
Bradenton, FL
Presenting Author(s)
Wilfredo J.. Javier-Rojas, MD, Alvin B.. Newman-Caro, DO, Yizhi Lin, DO, Carlos Montero, MD
HCA Florida Blake Hospital, Bradenton, FL
Introduction: Acute myeloid leukemia (AML) is a malignancy of immature myeloid cells, while cirrhosis is characterized by hepatic fibrosis. Both can present with anemia and thrombocytopenia, but hematologic abnormalities warrant further evaluation when gastrointestinal bleeding is absent. Although AML in cirrhotic patients has been reported, simultaneous new-onset AML and decompensated cirrhosis remains undocumented.
Case Description/
Methods: A 78-year-old female with iatrogenic hypothyroidism presented with lower extremity edema, fatigue, abdominal distension, low-grade fevers, and dyspnea. Labs revealed WBC 26.9 x10³/µL, Hb 5.5 g/dL, platelets 34 x10³/µL, MCV 123 fL, and 10% blasts. Peripheral smear showed macrocytosis, anisopoikilocytosis, and smudge cells. CMP showed total bilirubin 1.8 mg/dL, AST 49 U/L, and albumin 2.5 g/dL. Coagulation profile showed PT 17.1 sec, INR 1.6. CT abdomen/pelvis (Figure 1) showed a nodular liver, portal hypertension, large esophageal varices, and splenomegaly with infarct. EGD revealed grade 1 esophageal varices without high-risk stigmata and reactive gastropathy. Hematologic evaluation, including flow cytometry (Figure 2), confirmed AML. Iron studies showed elevated ferritin (1390 ng/mL), transferrin saturation (80%), and low TIBC—suggestive of hereditary hemochromatosis. Hepatitis panel, autoimmune workup, and metabolic risk factors were unremarkable. Given the absence of GI bleeding, hematologic malignancy was identified as the primary contributor to cytopenias. The patient was discharged to initiate AML treatment and outpatient follow-up was planned to include colonoscopy, capsule endoscopy if indicated and liver ultrasound elastography.
Discussion: This case highlights the diagnostic complexity when new-onset AML coexists with decompensated cirrhosis. Both conditions may present with fatigue, cytopenias, and organomegaly. In our patient, the absence of high-risk varices and GI bleeding necessitated further hematologic evaluation, ultimately confirming AML. Iron overload, suspected due to elevated ferritin and transferrin saturation, may be related to hereditary hemochromatosis and may have contributed to cirrhosis. Iron overload is associated with poor AML prognosis due to oxidative stress and genomic instability but has not been shown to increase AML incidence in hereditary hemochromatosis. This case underscores the importance of a thorough, multidisciplinary approach to evaluating overlapping hematologic and hepatic abnormalities.
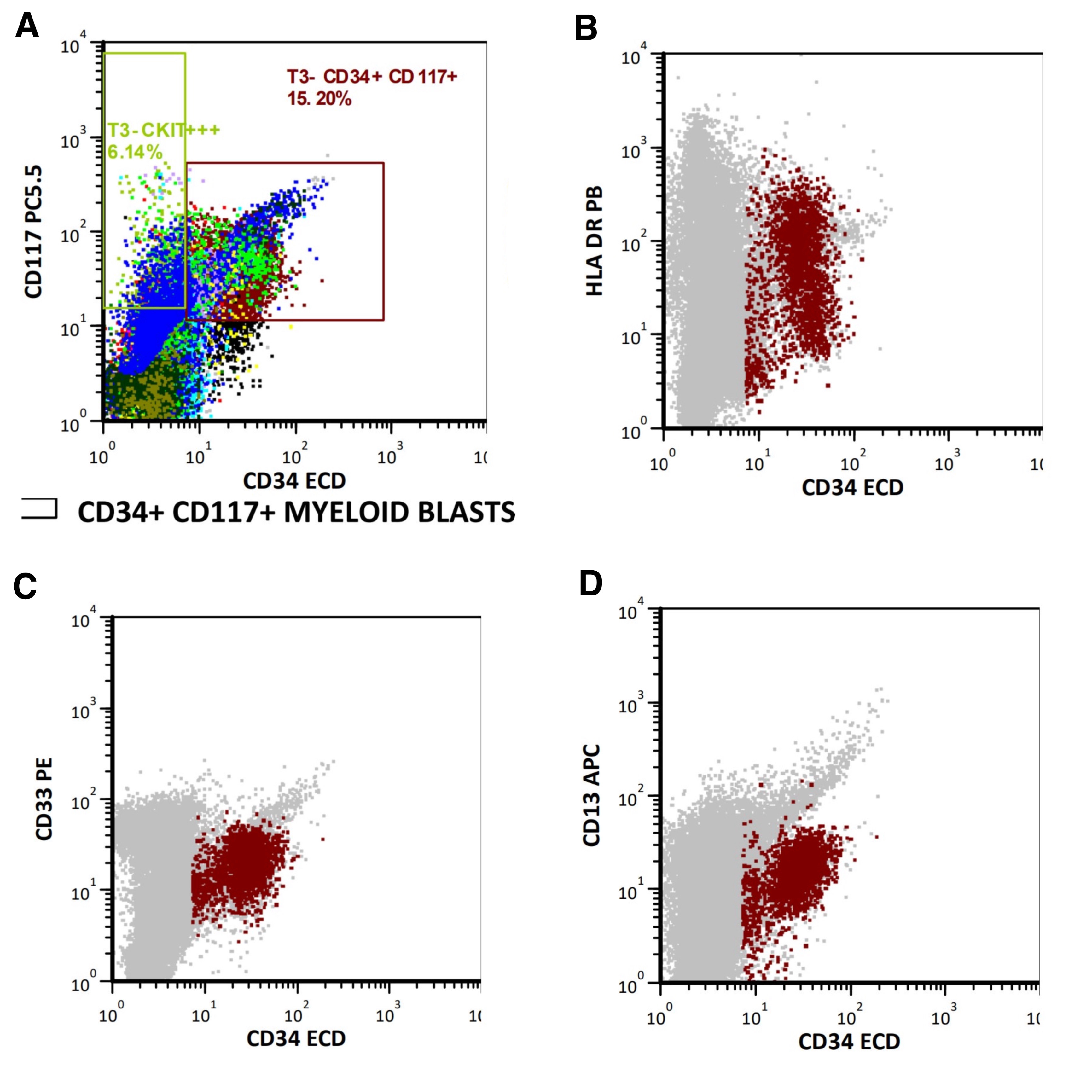
Figure: Figure 1. Contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis revealing a small, nodular liver consistent with cirrhosis, splenomegaly with a small infarct (red arrow), and minimal ascites. Additional findings included features of portal hypertension and large esophageal varices (not visualized in this image). Given the clinical context, the splenic infarction is more likely attributable to leukemic infiltration and compromised splenic blood flow from circulating AML cells, rather than portal hypertension.
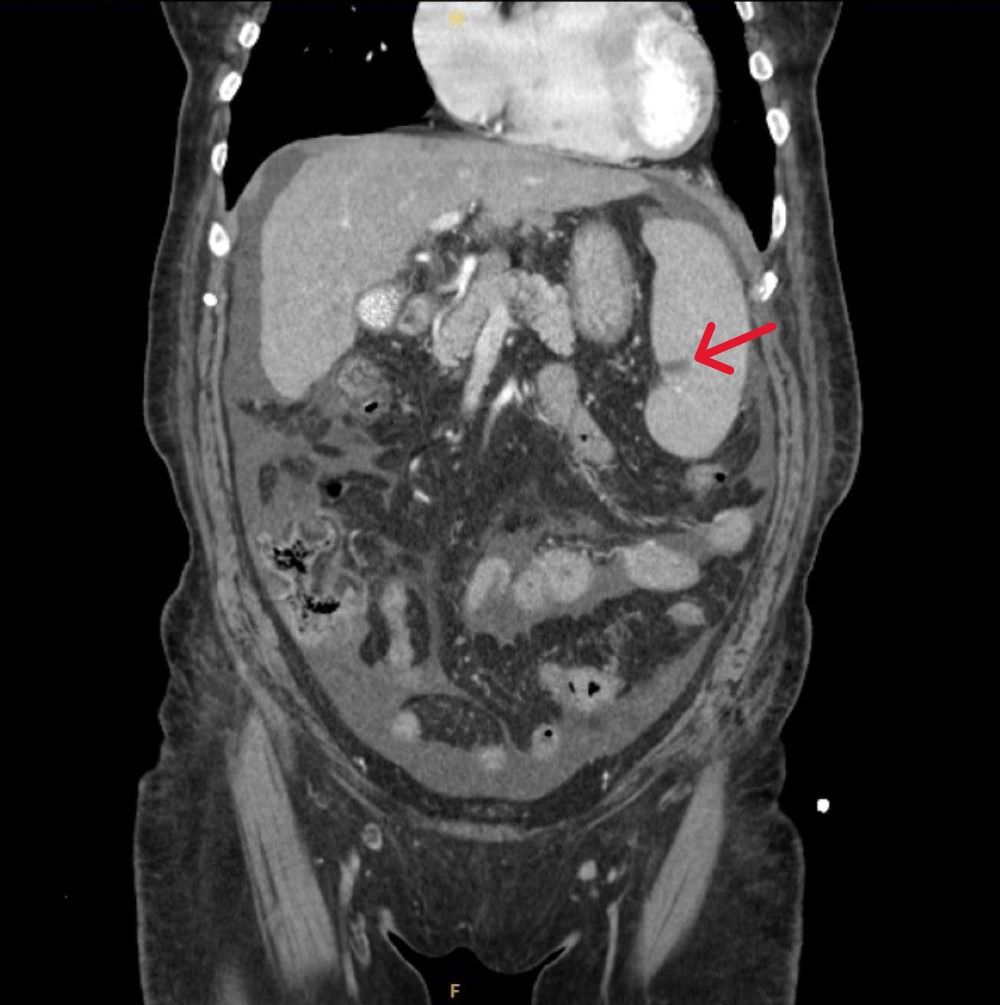
Figure: Figure 2. Dual fluorescence scatter plots from flow cytometry immunophenotyping obtained from peripheral blood demonstrating an increased population of circulating myeloid blasts (11.4% of cells), expressing CD34 (Image A), CD117 (Image A), HLA-DR (Image B), and subsets of CD33 (Image C) and CD13 (Image D), findings consistent with a diagnosis of acute myeloid leukemia (AML).
Disclosures:
Wilfredo Javier-Rojas indicated no relevant financial relationships.
Alvin Newman-Caro indicated no relevant financial relationships.
Yizhi Lin indicated no relevant financial relationships.
Carlos Montero indicated no relevant financial relationships.
Wilfredo J.. Javier-Rojas, MD, Alvin B.. Newman-Caro, DO, Yizhi Lin, DO, Carlos Montero, MD. P3985 - Disguised Malignancy: Acute Myeloid Leukemia Presenting as Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
HCA Florida Blake Hospital, Bradenton, FL
Introduction: Acute myeloid leukemia (AML) is a malignancy of immature myeloid cells, while cirrhosis is characterized by hepatic fibrosis. Both can present with anemia and thrombocytopenia, but hematologic abnormalities warrant further evaluation when gastrointestinal bleeding is absent. Although AML in cirrhotic patients has been reported, simultaneous new-onset AML and decompensated cirrhosis remains undocumented.
Case Description/
Methods: A 78-year-old female with iatrogenic hypothyroidism presented with lower extremity edema, fatigue, abdominal distension, low-grade fevers, and dyspnea. Labs revealed WBC 26.9 x10³/µL, Hb 5.5 g/dL, platelets 34 x10³/µL, MCV 123 fL, and 10% blasts. Peripheral smear showed macrocytosis, anisopoikilocytosis, and smudge cells. CMP showed total bilirubin 1.8 mg/dL, AST 49 U/L, and albumin 2.5 g/dL. Coagulation profile showed PT 17.1 sec, INR 1.6. CT abdomen/pelvis (Figure 1) showed a nodular liver, portal hypertension, large esophageal varices, and splenomegaly with infarct. EGD revealed grade 1 esophageal varices without high-risk stigmata and reactive gastropathy. Hematologic evaluation, including flow cytometry (Figure 2), confirmed AML. Iron studies showed elevated ferritin (1390 ng/mL), transferrin saturation (80%), and low TIBC—suggestive of hereditary hemochromatosis. Hepatitis panel, autoimmune workup, and metabolic risk factors were unremarkable. Given the absence of GI bleeding, hematologic malignancy was identified as the primary contributor to cytopenias. The patient was discharged to initiate AML treatment and outpatient follow-up was planned to include colonoscopy, capsule endoscopy if indicated and liver ultrasound elastography.
Discussion: This case highlights the diagnostic complexity when new-onset AML coexists with decompensated cirrhosis. Both conditions may present with fatigue, cytopenias, and organomegaly. In our patient, the absence of high-risk varices and GI bleeding necessitated further hematologic evaluation, ultimately confirming AML. Iron overload, suspected due to elevated ferritin and transferrin saturation, may be related to hereditary hemochromatosis and may have contributed to cirrhosis. Iron overload is associated with poor AML prognosis due to oxidative stress and genomic instability but has not been shown to increase AML incidence in hereditary hemochromatosis. This case underscores the importance of a thorough, multidisciplinary approach to evaluating overlapping hematologic and hepatic abnormalities.
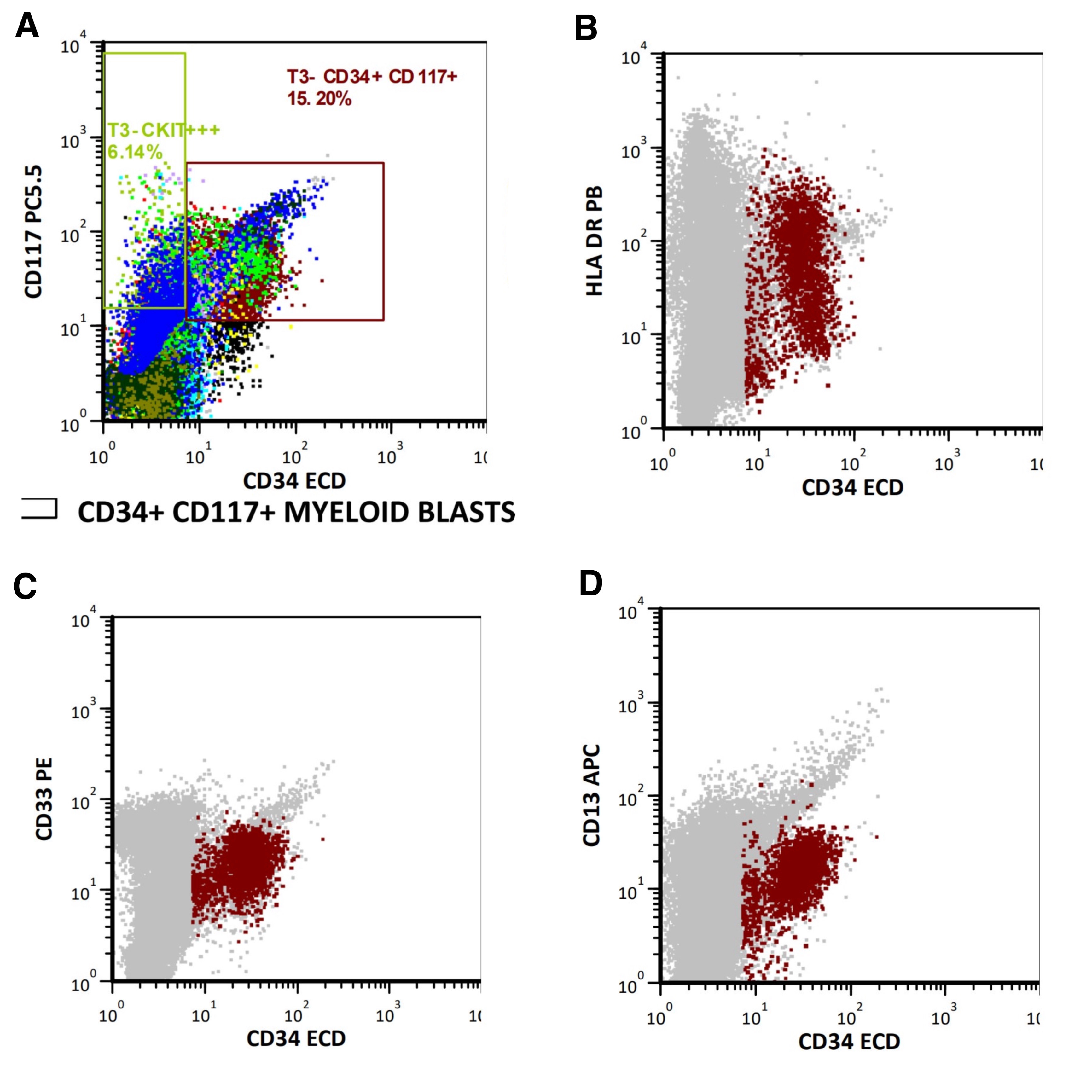
Figure: Figure 1. Contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis revealing a small, nodular liver consistent with cirrhosis, splenomegaly with a small infarct (red arrow), and minimal ascites. Additional findings included features of portal hypertension and large esophageal varices (not visualized in this image). Given the clinical context, the splenic infarction is more likely attributable to leukemic infiltration and compromised splenic blood flow from circulating AML cells, rather than portal hypertension.
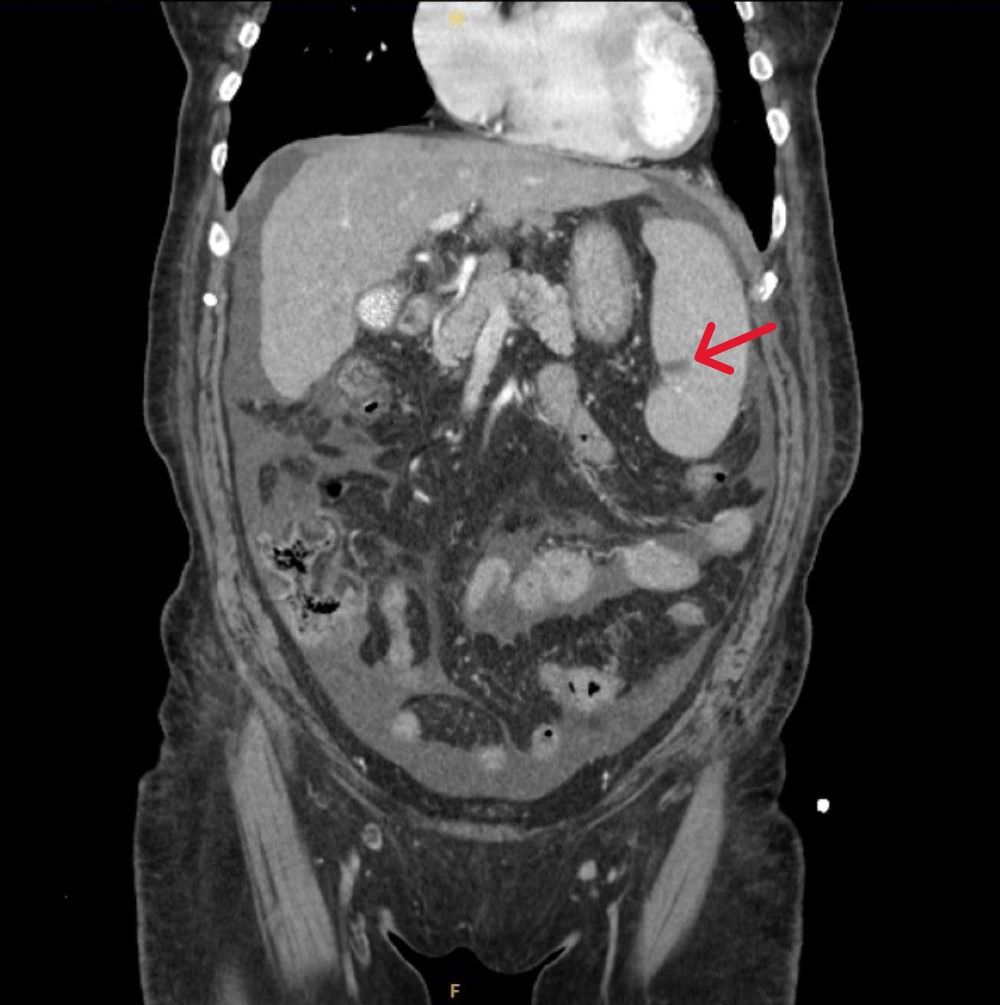
Figure: Figure 2. Dual fluorescence scatter plots from flow cytometry immunophenotyping obtained from peripheral blood demonstrating an increased population of circulating myeloid blasts (11.4% of cells), expressing CD34 (Image A), CD117 (Image A), HLA-DR (Image B), and subsets of CD33 (Image C) and CD13 (Image D), findings consistent with a diagnosis of acute myeloid leukemia (AML).
Disclosures:
Wilfredo Javier-Rojas indicated no relevant financial relationships.
Alvin Newman-Caro indicated no relevant financial relationships.
Yizhi Lin indicated no relevant financial relationships.
Carlos Montero indicated no relevant financial relationships.
Wilfredo J.. Javier-Rojas, MD, Alvin B.. Newman-Caro, DO, Yizhi Lin, DO, Carlos Montero, MD. P3985 - Disguised Malignancy: Acute Myeloid Leukemia Presenting as Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
