Monday Poster Session
Category: Liver
P3980 - Under Pressure: Granulomatous Liver Disease and Portal Hypertension in Disseminated MAC
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Emilio Fernandez, III, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Emilio Fernandez, MD1, Grecia Dominguez Rivera, MD1, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2, Fabian Rodas, MD2
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Mycobacterium avium complex (MAC), an environmental pathogen acquired via inhalation or ingestion, frequently causes disseminated disease in immunocompromised patients, notably those with AIDS. Hepatic involvement occurs in over 50% of disseminated cases, often manifesting as granulomatous liver disease. We present a case of a patient who developed transaminitis and new-onset ascites in the setting of granulomatous liver disease secondary to disseminated MAC.
Case Description/
Methods: A 27-year-old male with a past medical history of AIDS and disseminated MAC was directly admitted due to chronic diarrhea and MAC bacteremia. The patient was initially diagnosed with disseminated MAC in February 2024 and closely followed by ID with outpatient antibiotic management (rifabutin, ethambutol, and azithromycin). In late December 2024, the patient was admitted for esophageal candidiasis. Blood cultures at that time were positive for MAC with new resistances. The patient was admitted and began treatment with IV amikacin. During admission, the patient developed elevated liver-associated enzymes, AST 160 U/L, ALT 142 U/L, and ALP 518 U/L with new-onset ascites. A CT liver 4 phase was only significant for mild hepatomegaly. Paracentesis was performed with studies showing a serum-ascites albumin gradient of 1.3. An IR-guided transjugular liver biopsy was consistent with portal hypertension (portal gradient=22 mm Hg). Histology showed hepatic parenchyma with multiple non-necrotizing poorly formed granulomatous containing acid-fast bacilli, consistent with MAC. The patient was discharged on ethambutol, rifabutin, azithromycin, and IV amikacin. At a recent follow-up, the patient reports resolution of diarrhea, though he has still required 3 paracenteses in the 3 months following discharge. His liver-associated enzymes have since down trended and are now near or within normal limits: AST 19 U/L, ALT 16 U/L and ALP 179 U/L.
Discussion: Hepatic granulomas are observed in 2% to 10% of all liver biopsy specimens and are a hallmark of disseminated Mycobacterium avium complex infection, particularly in immunocompromised patients. Non-cirrhotic portal hypertension, as seen in this case, is a rare complication of granulomatous liver disease. Clinically, patients may present with ascites and other sequelae of portal hypertension. Pathophysiology involves granulomatous inflammation compressing intrahepatic venous lumina, coupled with fibrosis from resolving granulomas, which leads to elevated portal pressures.
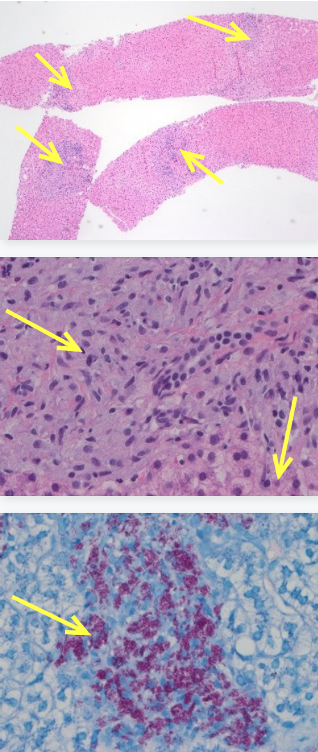
Figure: Fig 1. Low-power (40X mag) H&E with multiple non-necrotizing granulomata involving hepatic parenchyma. Fig 2. High-power (400X mag) H&E with non-necrotizing granuloma and also bile duct and hepatocytes in lower right. Fig 3. High-power (400X mag) Ziehl-Neelsen stain highlights abundant acid-fast bacilli.
Disclosures:
Emilio Fernandez indicated no relevant financial relationships.
Grecia Dominguez Rivera indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Emilio Fernandez, MD1, Grecia Dominguez Rivera, MD1, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2, Fabian Rodas, MD2. P3980 - Under Pressure: Granulomatous Liver Disease and Portal Hypertension in Disseminated MAC, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Mycobacterium avium complex (MAC), an environmental pathogen acquired via inhalation or ingestion, frequently causes disseminated disease in immunocompromised patients, notably those with AIDS. Hepatic involvement occurs in over 50% of disseminated cases, often manifesting as granulomatous liver disease. We present a case of a patient who developed transaminitis and new-onset ascites in the setting of granulomatous liver disease secondary to disseminated MAC.
Case Description/
Methods: A 27-year-old male with a past medical history of AIDS and disseminated MAC was directly admitted due to chronic diarrhea and MAC bacteremia. The patient was initially diagnosed with disseminated MAC in February 2024 and closely followed by ID with outpatient antibiotic management (rifabutin, ethambutol, and azithromycin). In late December 2024, the patient was admitted for esophageal candidiasis. Blood cultures at that time were positive for MAC with new resistances. The patient was admitted and began treatment with IV amikacin. During admission, the patient developed elevated liver-associated enzymes, AST 160 U/L, ALT 142 U/L, and ALP 518 U/L with new-onset ascites. A CT liver 4 phase was only significant for mild hepatomegaly. Paracentesis was performed with studies showing a serum-ascites albumin gradient of 1.3. An IR-guided transjugular liver biopsy was consistent with portal hypertension (portal gradient=22 mm Hg). Histology showed hepatic parenchyma with multiple non-necrotizing poorly formed granulomatous containing acid-fast bacilli, consistent with MAC. The patient was discharged on ethambutol, rifabutin, azithromycin, and IV amikacin. At a recent follow-up, the patient reports resolution of diarrhea, though he has still required 3 paracenteses in the 3 months following discharge. His liver-associated enzymes have since down trended and are now near or within normal limits: AST 19 U/L, ALT 16 U/L and ALP 179 U/L.
Discussion: Hepatic granulomas are observed in 2% to 10% of all liver biopsy specimens and are a hallmark of disseminated Mycobacterium avium complex infection, particularly in immunocompromised patients. Non-cirrhotic portal hypertension, as seen in this case, is a rare complication of granulomatous liver disease. Clinically, patients may present with ascites and other sequelae of portal hypertension. Pathophysiology involves granulomatous inflammation compressing intrahepatic venous lumina, coupled with fibrosis from resolving granulomas, which leads to elevated portal pressures.
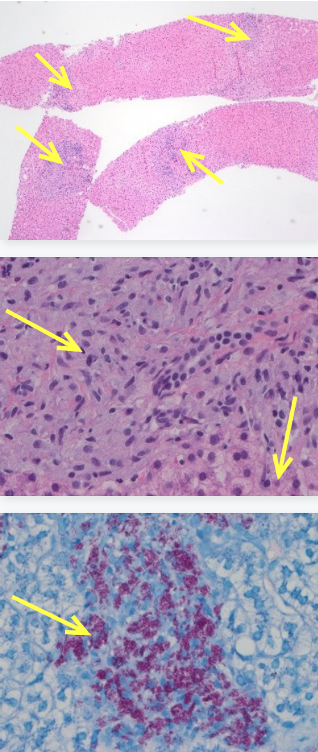
Figure: Fig 1. Low-power (40X mag) H&E with multiple non-necrotizing granulomata involving hepatic parenchyma. Fig 2. High-power (400X mag) H&E with non-necrotizing granuloma and also bile duct and hepatocytes in lower right. Fig 3. High-power (400X mag) Ziehl-Neelsen stain highlights abundant acid-fast bacilli.
Disclosures:
Emilio Fernandez indicated no relevant financial relationships.
Grecia Dominguez Rivera indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Emilio Fernandez, MD1, Grecia Dominguez Rivera, MD1, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2, Fabian Rodas, MD2. P3980 - Under Pressure: Granulomatous Liver Disease and Portal Hypertension in Disseminated MAC, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
