Monday Poster Session
Category: Liver
P3976 - Primary Hepatic GIST: Rare Tumor Defying Conventional Origins – A Case Report With Radiological-Pathological Correlation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sebastian Hermida Velasquez, DO
Palmetto General Hospital
Miami, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Sebastian Hermida Velasquez, DO1, Salaah M. Siddiqui, DO2, Sanskriti Sharma, MD3, Thatcher T. Huynh, DO3, Abelardo Broceta-Martinez, MD3, Natalia Martin, DO4, Karthik Mohan, DO3
1Palmetto General Hospital, Hialeah, FL; 2Palmetto General Hospital, Miami, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, South Miami, FL
Introduction: In clinical practice, occasionally one encounters cases that defy textbook descriptions. This holds particularly true for stromal tumors developing outside their usual anatomical boundaries. This patient's situation especially is noteworthy given both the radiological progression and the surgical/pathological confirmation of a tumor. Serial imaging shows an unusual metamorphosis from fluid-filled cyst to solid tumor mass over sixteen months; a progression pattern rare for liver based GISTs. It was through surgical exploration and pathological examination, that we were able to confirm the tumor's origin within liver tissue rather than secondary spread.
Case Description/
Methods: Our case involves an 82-year-old female presenting with right upper quadrant pain. Sixteen months prior, a CT scan had shown an innocent-appearing 4.9 cm liver cyst. New imaging now revealing a startling transformation: 8.8 cm solid mass emerging from hepatic segment III. Diagnostic upper endoscopy with endoscopic ultrasound was performed, which showed normal esophageal gastric and duodenal anatomy. EUS identified a 9×6 cm solid, necrotic-appearing mass within the left hepatic lobe, distinct from the gastric wall. Fine-needle aspiration of this lesion confirmed the diagnosis of GIST with no malignant cells detected in EGD gastric biopsies. After surgical resection, the report showed tumor bulk deeply embedded in liver tissue, minimal contact with the stomach's outer surface. Repeat pathology revealed gradual infiltration with entrapped hepatocytes at the periphery, a pattern characteristic of primary hepatic neoplasms. Gastric involvement was limited to reactive changes, without submucosal penetration.
Discussion: This case fundamentally challenges the assumption that hepatic GISTs must represent metastases. Serial imaging documenting the lesion developing primarily within the liver for over a year before any gastric contact appeared showed an unlikely progression for a metastatic lesion. Also, histological evidence revealing a growth pattern with hepatic focus and gradual hepatocyte displacement and no gastric submucosa involvement raises multiple questions as to the source of this tumor. The evidence suggests these rare tumors may develop through distinct biological pathways, requiring alternate diagnostic and therapeutic approaches. Most importantly, it serves as a reminder that medical knowledge evolves through rare cases; each one challenging our assumptions and expanding our understanding of disease processes.
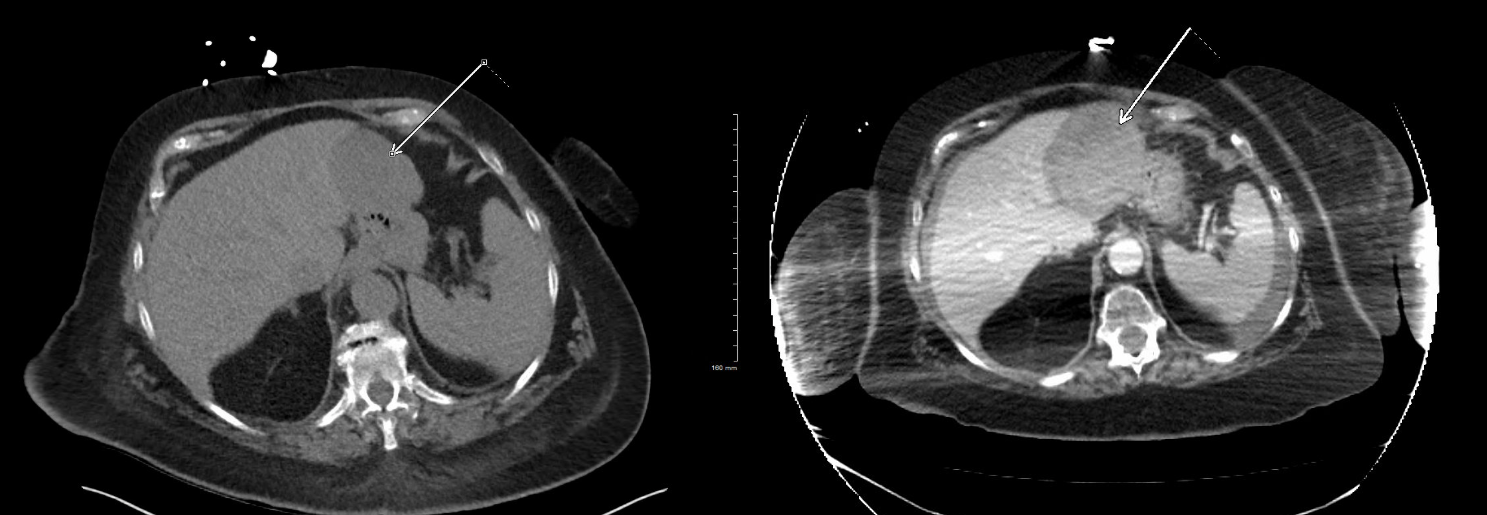
Figure: Figure 1. Serial axial CT images demonstrating the unusual progression of a hepatic lesion from a benign-appearing cyst to a
solid mass. Initial non-contrast CT reveals a 4.9 cm hypodense cystic lesion (left arrow) in segment III of the liver, with no
solid components or wall thickening. Follow-up contrast-enhanced CT 16 months later shows a heterogeneously enhancing
8.8 cm solid mass (right arrowhead) with central necrosis, arising from the same location.
Disclosures:
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Salaah Siddiqui indicated no relevant financial relationships.
Sanskriti Sharma indicated no relevant financial relationships.
Thatcher Huynh indicated no relevant financial relationships.
Abelardo Broceta-Martinez indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Sebastian Hermida Velasquez, DO1, Salaah M. Siddiqui, DO2, Sanskriti Sharma, MD3, Thatcher T. Huynh, DO3, Abelardo Broceta-Martinez, MD3, Natalia Martin, DO4, Karthik Mohan, DO3. P3976 - Primary Hepatic GIST: Rare Tumor Defying Conventional Origins – A Case Report With Radiological-Pathological Correlation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sebastian Hermida Velasquez, DO1, Salaah M. Siddiqui, DO2, Sanskriti Sharma, MD3, Thatcher T. Huynh, DO3, Abelardo Broceta-Martinez, MD3, Natalia Martin, DO4, Karthik Mohan, DO3
1Palmetto General Hospital, Hialeah, FL; 2Palmetto General Hospital, Miami, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, South Miami, FL
Introduction: In clinical practice, occasionally one encounters cases that defy textbook descriptions. This holds particularly true for stromal tumors developing outside their usual anatomical boundaries. This patient's situation especially is noteworthy given both the radiological progression and the surgical/pathological confirmation of a tumor. Serial imaging shows an unusual metamorphosis from fluid-filled cyst to solid tumor mass over sixteen months; a progression pattern rare for liver based GISTs. It was through surgical exploration and pathological examination, that we were able to confirm the tumor's origin within liver tissue rather than secondary spread.
Case Description/
Methods: Our case involves an 82-year-old female presenting with right upper quadrant pain. Sixteen months prior, a CT scan had shown an innocent-appearing 4.9 cm liver cyst. New imaging now revealing a startling transformation: 8.8 cm solid mass emerging from hepatic segment III. Diagnostic upper endoscopy with endoscopic ultrasound was performed, which showed normal esophageal gastric and duodenal anatomy. EUS identified a 9×6 cm solid, necrotic-appearing mass within the left hepatic lobe, distinct from the gastric wall. Fine-needle aspiration of this lesion confirmed the diagnosis of GIST with no malignant cells detected in EGD gastric biopsies. After surgical resection, the report showed tumor bulk deeply embedded in liver tissue, minimal contact with the stomach's outer surface. Repeat pathology revealed gradual infiltration with entrapped hepatocytes at the periphery, a pattern characteristic of primary hepatic neoplasms. Gastric involvement was limited to reactive changes, without submucosal penetration.
Discussion: This case fundamentally challenges the assumption that hepatic GISTs must represent metastases. Serial imaging documenting the lesion developing primarily within the liver for over a year before any gastric contact appeared showed an unlikely progression for a metastatic lesion. Also, histological evidence revealing a growth pattern with hepatic focus and gradual hepatocyte displacement and no gastric submucosa involvement raises multiple questions as to the source of this tumor. The evidence suggests these rare tumors may develop through distinct biological pathways, requiring alternate diagnostic and therapeutic approaches. Most importantly, it serves as a reminder that medical knowledge evolves through rare cases; each one challenging our assumptions and expanding our understanding of disease processes.
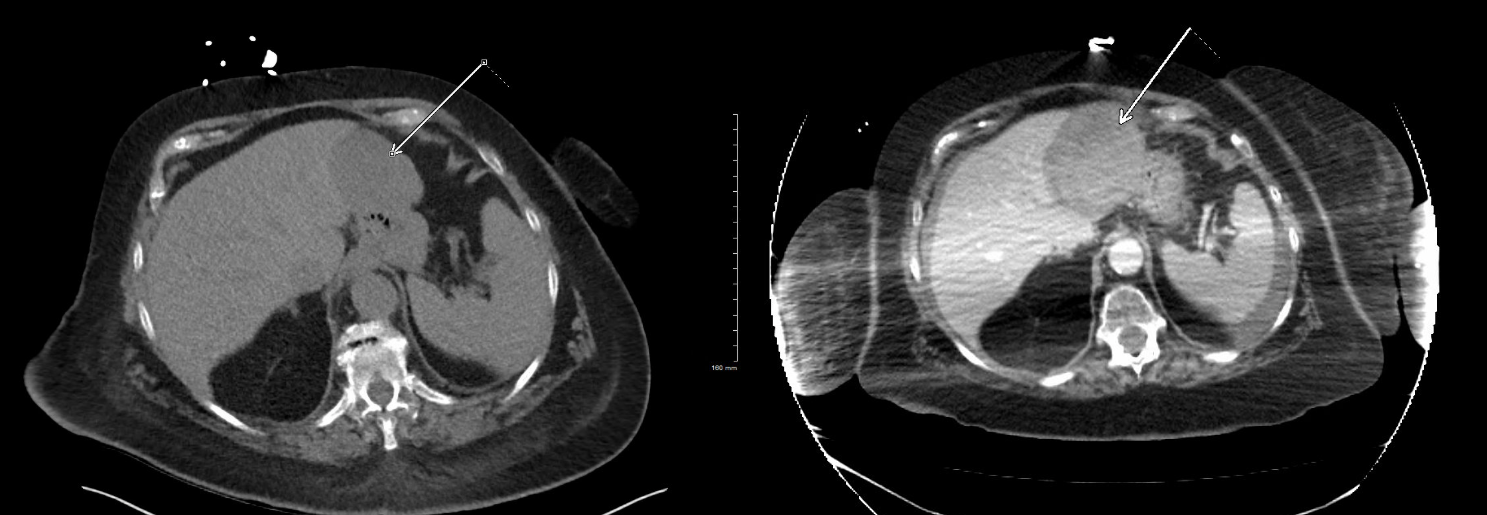
Figure: Figure 1. Serial axial CT images demonstrating the unusual progression of a hepatic lesion from a benign-appearing cyst to a
solid mass. Initial non-contrast CT reveals a 4.9 cm hypodense cystic lesion (left arrow) in segment III of the liver, with no
solid components or wall thickening. Follow-up contrast-enhanced CT 16 months later shows a heterogeneously enhancing
8.8 cm solid mass (right arrowhead) with central necrosis, arising from the same location.
Disclosures:
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Salaah Siddiqui indicated no relevant financial relationships.
Sanskriti Sharma indicated no relevant financial relationships.
Thatcher Huynh indicated no relevant financial relationships.
Abelardo Broceta-Martinez indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Sebastian Hermida Velasquez, DO1, Salaah M. Siddiqui, DO2, Sanskriti Sharma, MD3, Thatcher T. Huynh, DO3, Abelardo Broceta-Martinez, MD3, Natalia Martin, DO4, Karthik Mohan, DO3. P3976 - Primary Hepatic GIST: Rare Tumor Defying Conventional Origins – A Case Report With Radiological-Pathological Correlation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

