Monday Poster Session
Category: Liver
P3972 - Not Your Usual Culprit: Elevated Liver Enzymes Confounding Immune-Mediated Necrotizing Myopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Sohini Samaddar, MBBS (she/her/hers)
University of Kansas Medical Center
Kansas City, KS
Presenting Author(s)
Sohini Samaddar, MBBS1, Zunirah Ahmed, MD1, Daffolyn Rachael Fels Elliott, MD1, Areeba Fatima, MBBS2
1University of Kansas Medical Center, Kansas City, KS; 2Civil Hospital Karachi, Karachi, Sindh, Pakistan
Introduction: Immune-mediated necrotizing myopathy (IMNM) is a rare autoimmune condition that typically presents with progressive muscle weakness and elevated creatine kinase (CK) levels. The disease is strongly associated with anti-3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR) antibodies and often occurs in patients with prior statin exposure. In some cases, liver enzyme elevations may precede or accompany muscle symptoms, potentially obscuring the diagnosis.
Case Description/
Methods: A 72-year-old man with a history of hypertension, atrial fibrillation, prediabetes, obstructive sleep apnea, and non-ischemic cardiomyopathy presented with fatigue, anorexia, and significant weight loss. One month later, he was admitted for evaluation of transaminase elevation and new-onset proximal muscle weakness. He had been on atorvastatin for four years, which was increased to 40 mg daily shortly before presentation and discontinued following admission.
Laboratory testing showed AST 116 U/L, ALT 155 U/L, and CK 2269 U/L. Autoimmune serologies revealed a positive antinuclear antibody (ANA) at 1:320 and anti-smooth muscle antibody at 1:80. On this basis, a short corticosteroid taper was prescribed. A liver biopsy subsequently revealed only mild steatosis (Fig. 1 and 2) and no evidence of autoimmune hepatitis or other hepatic pathology.
Due to persistent weakness and elevated CK, further testing was performed, which demonstrated a strongly positive anti-HMGCR antibody (98 units). Myositis-specific and paraneoplastic panels were negative. These findings established the diagnosis of IMNM. The patient was started on high-dose prednisone, with plans to initiate methotrexate and intravenous immunoglobulin (IVIG). Over the following two months, liver enzymes declined, with AST decreasing from 116 U/L to 56 U/L and ALT from 155 U/L to 89 U/L, corresponding with the initiation of corticosteroid therapy.
Discussion: This case emphasizes the need to consider muscle-derived causes of transaminase elevation, particularly when clinical features extend beyond the liver. IMNM, though uncommon, should be part of the differential in patients presenting with constitutional symptoms, elevated liver enzymes, and muscle involvement—especially in the context of recent statin use. Early identification can prevent unnecessary hepatic interventions and guide appropriate immunosuppressive therapy.
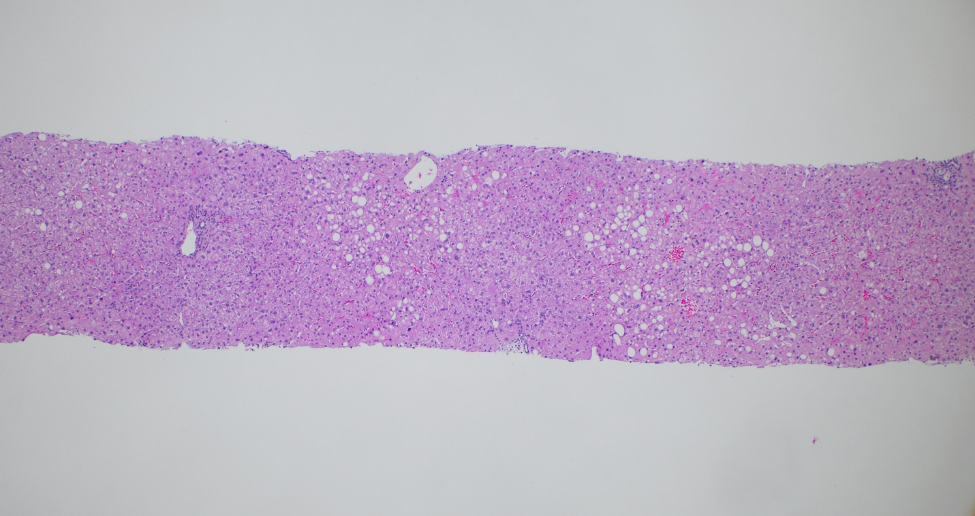
Figure: Liver core biopsy shows mild macrovesicular steatosis (H&E stain, x40)
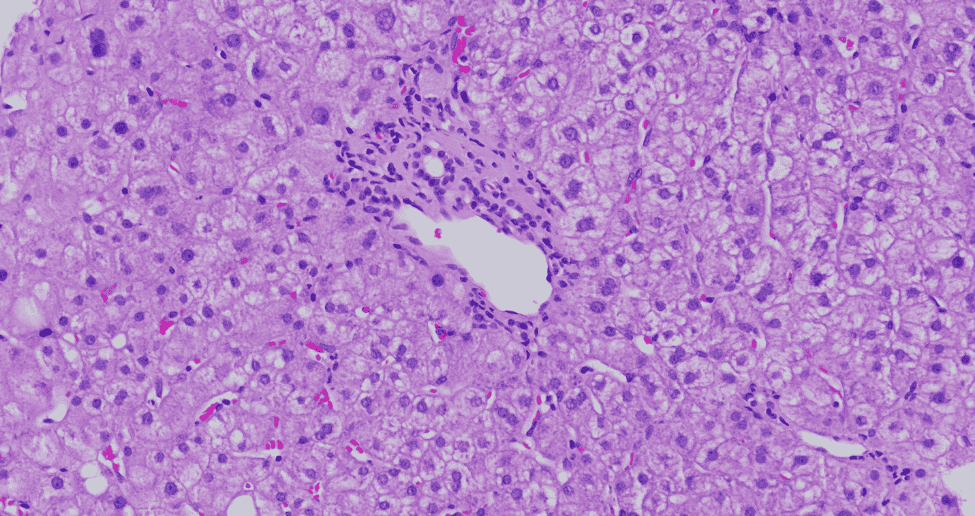
Figure: Portal tract with minimal inflammation and intact bile duct. Hepatocytes show mild swelling with cytoplasmic clearing (H&E stain, x200)
Disclosures:
Sohini Samaddar indicated no relevant financial relationships.
Zunirah Ahmed indicated no relevant financial relationships.
Daffolyn Rachael Fels Elliott indicated no relevant financial relationships.
Areeba Fatima indicated no relevant financial relationships.
Sohini Samaddar, MBBS1, Zunirah Ahmed, MD1, Daffolyn Rachael Fels Elliott, MD1, Areeba Fatima, MBBS2. P3972 - Not Your Usual Culprit: Elevated Liver Enzymes Confounding Immune-Mediated Necrotizing Myopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas Medical Center, Kansas City, KS; 2Civil Hospital Karachi, Karachi, Sindh, Pakistan
Introduction: Immune-mediated necrotizing myopathy (IMNM) is a rare autoimmune condition that typically presents with progressive muscle weakness and elevated creatine kinase (CK) levels. The disease is strongly associated with anti-3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR) antibodies and often occurs in patients with prior statin exposure. In some cases, liver enzyme elevations may precede or accompany muscle symptoms, potentially obscuring the diagnosis.
Case Description/
Methods: A 72-year-old man with a history of hypertension, atrial fibrillation, prediabetes, obstructive sleep apnea, and non-ischemic cardiomyopathy presented with fatigue, anorexia, and significant weight loss. One month later, he was admitted for evaluation of transaminase elevation and new-onset proximal muscle weakness. He had been on atorvastatin for four years, which was increased to 40 mg daily shortly before presentation and discontinued following admission.
Laboratory testing showed AST 116 U/L, ALT 155 U/L, and CK 2269 U/L. Autoimmune serologies revealed a positive antinuclear antibody (ANA) at 1:320 and anti-smooth muscle antibody at 1:80. On this basis, a short corticosteroid taper was prescribed. A liver biopsy subsequently revealed only mild steatosis (Fig. 1 and 2) and no evidence of autoimmune hepatitis or other hepatic pathology.
Due to persistent weakness and elevated CK, further testing was performed, which demonstrated a strongly positive anti-HMGCR antibody (98 units). Myositis-specific and paraneoplastic panels were negative. These findings established the diagnosis of IMNM. The patient was started on high-dose prednisone, with plans to initiate methotrexate and intravenous immunoglobulin (IVIG). Over the following two months, liver enzymes declined, with AST decreasing from 116 U/L to 56 U/L and ALT from 155 U/L to 89 U/L, corresponding with the initiation of corticosteroid therapy.
Discussion: This case emphasizes the need to consider muscle-derived causes of transaminase elevation, particularly when clinical features extend beyond the liver. IMNM, though uncommon, should be part of the differential in patients presenting with constitutional symptoms, elevated liver enzymes, and muscle involvement—especially in the context of recent statin use. Early identification can prevent unnecessary hepatic interventions and guide appropriate immunosuppressive therapy.
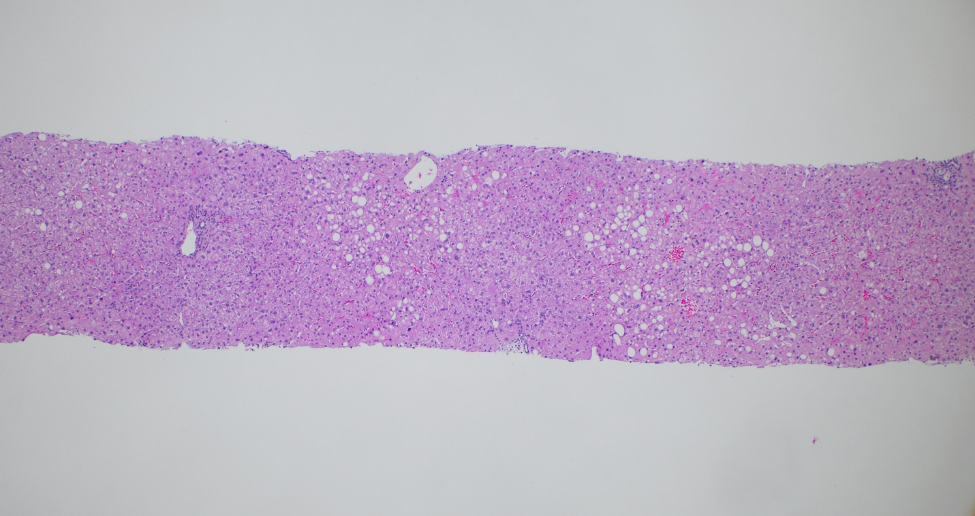
Figure: Liver core biopsy shows mild macrovesicular steatosis (H&E stain, x40)
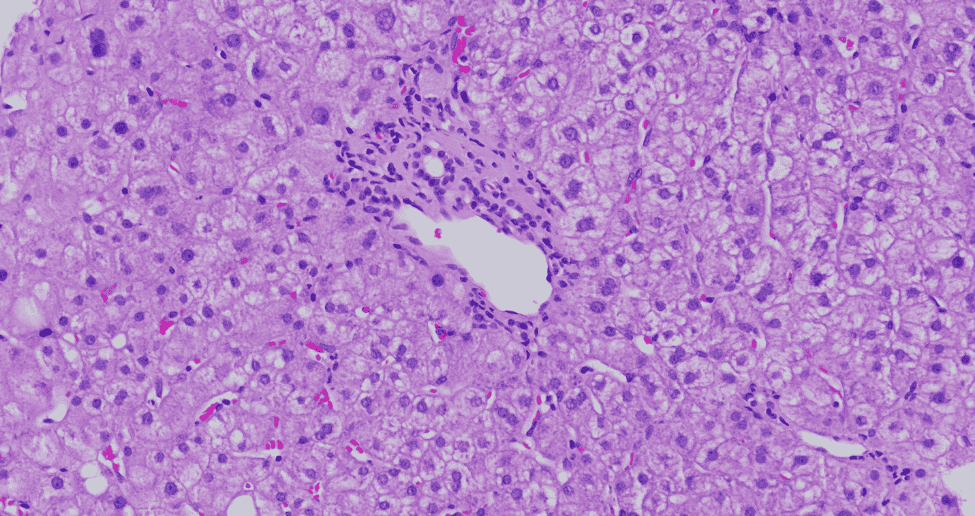
Figure: Portal tract with minimal inflammation and intact bile duct. Hepatocytes show mild swelling with cytoplasmic clearing (H&E stain, x200)
Disclosures:
Sohini Samaddar indicated no relevant financial relationships.
Zunirah Ahmed indicated no relevant financial relationships.
Daffolyn Rachael Fels Elliott indicated no relevant financial relationships.
Areeba Fatima indicated no relevant financial relationships.
Sohini Samaddar, MBBS1, Zunirah Ahmed, MD1, Daffolyn Rachael Fels Elliott, MD1, Areeba Fatima, MBBS2. P3972 - Not Your Usual Culprit: Elevated Liver Enzymes Confounding Immune-Mediated Necrotizing Myopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

