Monday Poster Session
Category: Liver
P3965 - Chronic Sickle Cell Intrahepatic Cholestasis: A Silent Driver of Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TK
Taofeek Kolade, MD, MBA, MPH (he/him/his)
Bayonne Medical Center
Bayonne, NJ
Presenting Author(s)
Taofeek Kolade, MD, MBA, MPH1, Het Pandya, MD2, Ramsey Jaber, MD, MPH1, Philip Hall, MD, MPH2, Harleen Kaur, MD1
1Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Sickle cell intrahepatic cholestasis (SCIC) is a rare but potentially fatal complication of sickle cell disease (SCD), with fewer than 50 cases reported in the U.S. It results from sinusoidal obstruction by sickled erythrocytes, leading to hepatic ischemia, necrosis, and cholestasis. Though typically acute, SCIC may present chronically and contribute silently to progressive liver disease. We present a case of chronic SCIC in a young adult, highlighting its underrecognized role in cirrhosis development.
Case Description/
Methods: A 31-year-old male with SCD, prior splenectomy, and cholecystectomy presented with progressive jaundice, self-resolving epistaxis, and epigastric pain. He reported no recent sickle crises and had not sought medical care in 13 years. Family history was non-contributory. He denied alcohol or drug use. On exam, he was febrile, tachycardic, and visibly jaundiced. Labs revealed hemoglobin 5.9 g/dL, leukocytosis, total bilirubin 43.3 mg/dL (direct 35.8), elevated AST, ALP, LDH (2281), high-normal ALT, and INR 1.66. Renal function was preserved. Viral hepatitis, HIV, and AFP were negative. Lipase and amylase were elevated. CT showed a nodular liver and gastroesophageal varices, consistent with cirrhosis and portal hypertension. Doppler ultrasound confirmed patent vasculature without biliary dilation. MRCP demonstrated signal dropout on gradient echo imaging, suggestive of iron or mineral deposition. The pancreas appeared normal. Findings supported chronic SCIC. Red blood cell exchange transfusion and supportive care were advised, but the patient declined further treatment and was lost to follow-up.
Discussion: SCIC ranges from mild jaundice to fulminant liver failure and is frequently underdiagnosed. Although no standardized diagnostic criteria exist, this patient’s presentation of jaundice, fever, hepatomegaly, leukocytosis, and liver enzyme abnormalities all align with features described in case literature. Imaging revealed cirrhosis, a finding rarely reported in SCIC and unusual in the absence of traditional risk factors. This suggests repeated, unrecognized SCIC episodes during his prolonged care gap. MRCP supported ongoing hepatic injury. While liver biopsy is diagnostic, it is often contraindicated due to coagulopathy. RBC exchange may improve outcomes but was declined. This case underscores the importance of routine hepatic surveillance in patients with SCD and raises awareness of SCIC as a potential precursor to cirrhosis.

Figure: CT Abdomen Pelvis with Intravenous contrast- ( axial view)- Shows significant hepatomegaly, left lobe of liver is markedly enlarged, liver contour is lobulated. Right lobe of liver measures 18.7 cm. Main portal vein measures 1.4 cm.
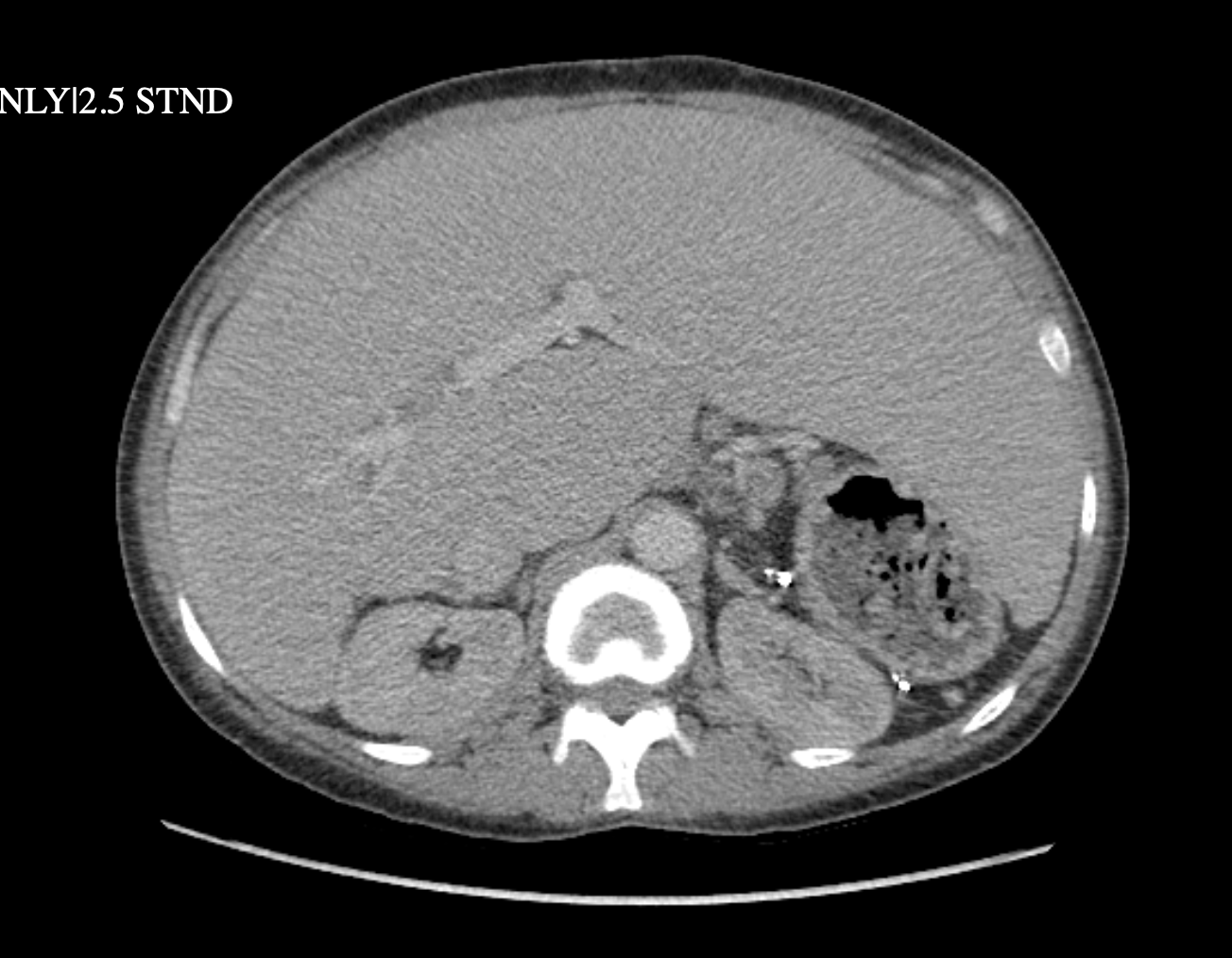
Figure: MRCP (coronal view) shows hepatomegaly, right lobe of liver measures 20.3 cm. Diffuse nodular texture, lobulated border of the liver suggestive of cirrhotic liver. Signal dropout of the liver from gradient echo ultra phase to inphase, suggestive of iron deposition or mineral deposition. Small perihepatic ascites.
Disclosures:
Taofeek Kolade indicated no relevant financial relationships.
Het Pandya indicated no relevant financial relationships.
Ramsey Jaber indicated no relevant financial relationships.
Philip Hall indicated no relevant financial relationships.
Harleen Kaur indicated no relevant financial relationships.
Taofeek Kolade, MD, MBA, MPH1, Het Pandya, MD2, Ramsey Jaber, MD, MPH1, Philip Hall, MD, MPH2, Harleen Kaur, MD1. P3965 - Chronic Sickle Cell Intrahepatic Cholestasis: A Silent Driver of Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Sickle cell intrahepatic cholestasis (SCIC) is a rare but potentially fatal complication of sickle cell disease (SCD), with fewer than 50 cases reported in the U.S. It results from sinusoidal obstruction by sickled erythrocytes, leading to hepatic ischemia, necrosis, and cholestasis. Though typically acute, SCIC may present chronically and contribute silently to progressive liver disease. We present a case of chronic SCIC in a young adult, highlighting its underrecognized role in cirrhosis development.
Case Description/
Methods: A 31-year-old male with SCD, prior splenectomy, and cholecystectomy presented with progressive jaundice, self-resolving epistaxis, and epigastric pain. He reported no recent sickle crises and had not sought medical care in 13 years. Family history was non-contributory. He denied alcohol or drug use. On exam, he was febrile, tachycardic, and visibly jaundiced. Labs revealed hemoglobin 5.9 g/dL, leukocytosis, total bilirubin 43.3 mg/dL (direct 35.8), elevated AST, ALP, LDH (2281), high-normal ALT, and INR 1.66. Renal function was preserved. Viral hepatitis, HIV, and AFP were negative. Lipase and amylase were elevated. CT showed a nodular liver and gastroesophageal varices, consistent with cirrhosis and portal hypertension. Doppler ultrasound confirmed patent vasculature without biliary dilation. MRCP demonstrated signal dropout on gradient echo imaging, suggestive of iron or mineral deposition. The pancreas appeared normal. Findings supported chronic SCIC. Red blood cell exchange transfusion and supportive care were advised, but the patient declined further treatment and was lost to follow-up.
Discussion: SCIC ranges from mild jaundice to fulminant liver failure and is frequently underdiagnosed. Although no standardized diagnostic criteria exist, this patient’s presentation of jaundice, fever, hepatomegaly, leukocytosis, and liver enzyme abnormalities all align with features described in case literature. Imaging revealed cirrhosis, a finding rarely reported in SCIC and unusual in the absence of traditional risk factors. This suggests repeated, unrecognized SCIC episodes during his prolonged care gap. MRCP supported ongoing hepatic injury. While liver biopsy is diagnostic, it is often contraindicated due to coagulopathy. RBC exchange may improve outcomes but was declined. This case underscores the importance of routine hepatic surveillance in patients with SCD and raises awareness of SCIC as a potential precursor to cirrhosis.

Figure: CT Abdomen Pelvis with Intravenous contrast- ( axial view)- Shows significant hepatomegaly, left lobe of liver is markedly enlarged, liver contour is lobulated. Right lobe of liver measures 18.7 cm. Main portal vein measures 1.4 cm.
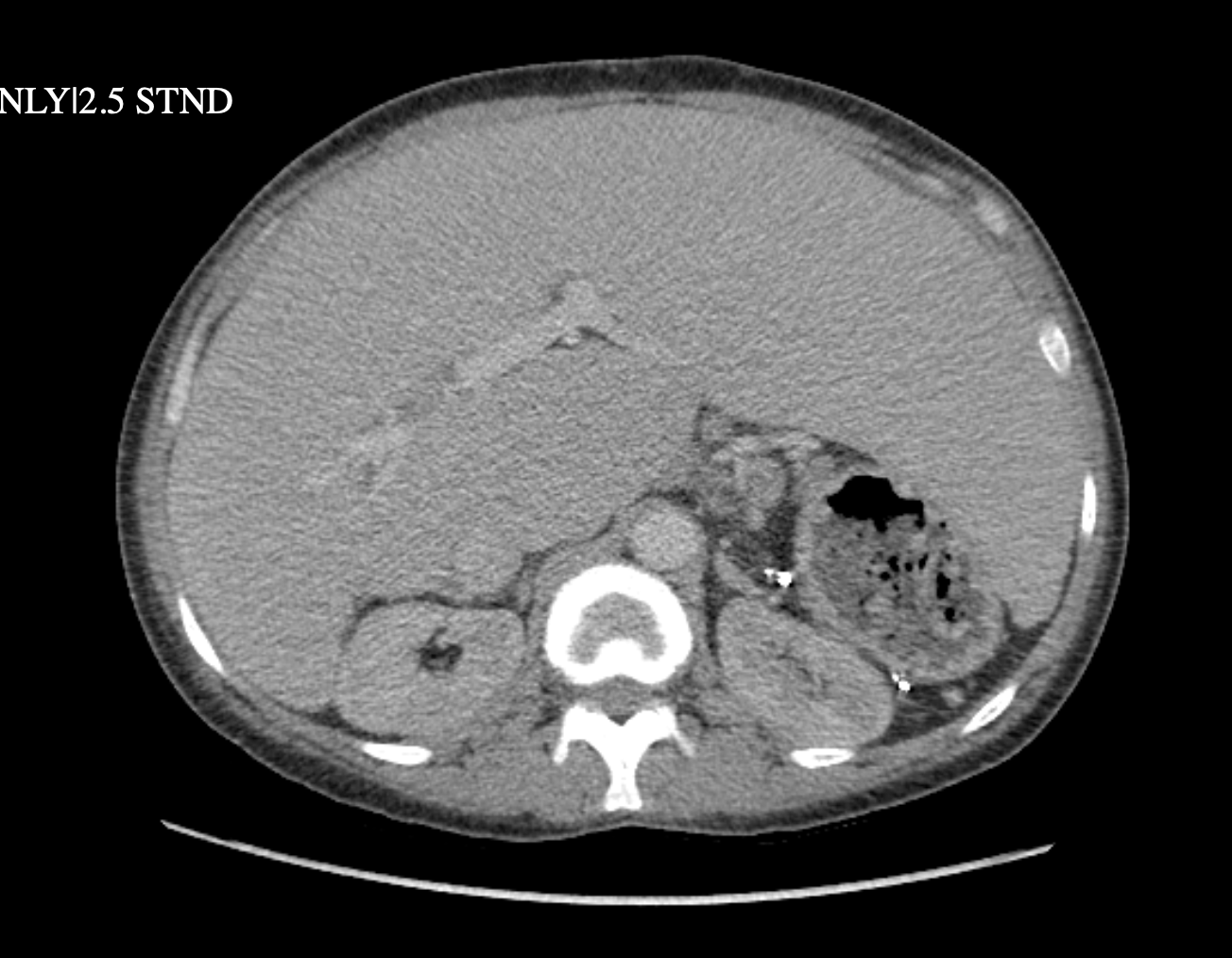
Figure: MRCP (coronal view) shows hepatomegaly, right lobe of liver measures 20.3 cm. Diffuse nodular texture, lobulated border of the liver suggestive of cirrhotic liver. Signal dropout of the liver from gradient echo ultra phase to inphase, suggestive of iron deposition or mineral deposition. Small perihepatic ascites.
Disclosures:
Taofeek Kolade indicated no relevant financial relationships.
Het Pandya indicated no relevant financial relationships.
Ramsey Jaber indicated no relevant financial relationships.
Philip Hall indicated no relevant financial relationships.
Harleen Kaur indicated no relevant financial relationships.
Taofeek Kolade, MD, MBA, MPH1, Het Pandya, MD2, Ramsey Jaber, MD, MPH1, Philip Hall, MD, MPH2, Harleen Kaur, MD1. P3965 - Chronic Sickle Cell Intrahepatic Cholestasis: A Silent Driver of Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
