Monday Poster Session
Category: Liver
P3932 - A Rare Complication of TNF-α Inhibitor With Histoplasmosis Associated Necrotizing Granulomatous Hepatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mena Saad, DO
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Mena Saad, DO1, Medora Doris. Rodrigues, MD, MPH2, Jonathan Scott, MD3, Ronaldo Gnass, MD1, Khalid Mumtaz, MBBS, MSc2, Wichit Srikureja, MD4
1Riverside University Health System, Moreno Valley, CA; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Riverside University Health System, Riverside, CA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Histoplasma capsulatum is a dimorphic fungus endemic to the central and eastern U.S. Disseminated histoplasmosis, its most severe form, can rarely cause necrotizing granulomatous hepatitis. Clinical presentation includes fever, malaise, jaundice, abdominal pain, and cholestatic liver enzyme abnormalities.
Case Description/
Methods: A 62-year-old man from Mexico with rheumatoid arthritis, previously on infliximab, was admitted with abdominal pain. He was febrile at 102.7°F and tachycardic. Physical examination showed icterus; right upper quadrant tenderness without guarding; and without hepato-splenomegaly. Initial labs showed elevated liver tests (LFTs): total bilirubin 2.5 mg/dL, alkaline phosphatase 284 U/L, AST 132 U/L, ALT 311 U/L. CT chest showed diffuse ground glass opacities and mediastinal adenopathy. Ultrasound showed gallstones and normal bile duct size. Endoscopic ultrasound (EUS) was done and showed gallstones and normal CBD with sludge. ERCP with biliary sphincterotomy and stent placement was done. However, LFTs elevation persisted. EUS guided liver biopsy was then undertaken with preliminary finding of necrotizing granulomatous hepatitis. Infectious workup revealed a positive QuantiFERON Gold and coccidioidomycosis serology. He was started and discharged on anti-tuberculosis regimen and fluconazole. However, his LFTs continue to be elevated. Final liver pathology demonstrated numerous intracellular yeasts with halos, consistent with Histoplasma capsulatum (Fig. 1&2). Positive coccidioidomycosis serology was thought to reflect cross-reactivity with histoplasma antigens. He was readmitted and started on liposomal amphotericin B. His anti-tuberculosis regimen was consolidated. Fluconazole was stopped. LFTs normalized within 2 days. He was discharged with itraconazole for 12 months.
Discussion: Histoplasmosis associated necrotizing granulomatous hepatitis is a rare complication in patients on tumor necrosis factor-α inhibitor. Disseminated histoplasmosis often occurs in immunosuppressed patients. Symptoms usually are organ specific and can include fever, fatigue, and weight loss. Hepatic involvement with elevated liver tests can mimic other liver and biliary diseases. The diagnosis is often based on antigen testing and/or histopathology. Our case illustrated a rare disseminated histoplasmosis associated with necrotizing granulomatous hepatitis confirmed on liver pathology. We believe that high index of suspicion combined with early liver biopsy led to a favorable outcome in our case.
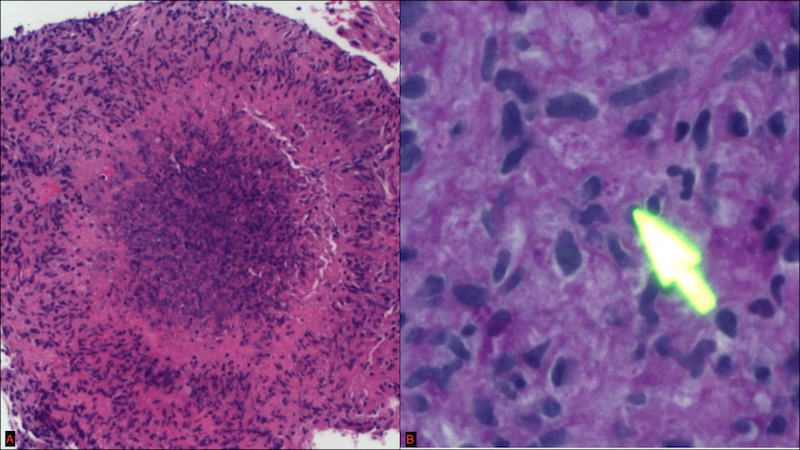
Figure: Figure 1A. Granulomatous hepatitis (H&E)
Figure 1B. Histoplasma microorganisms-budding yeasts (GMS)
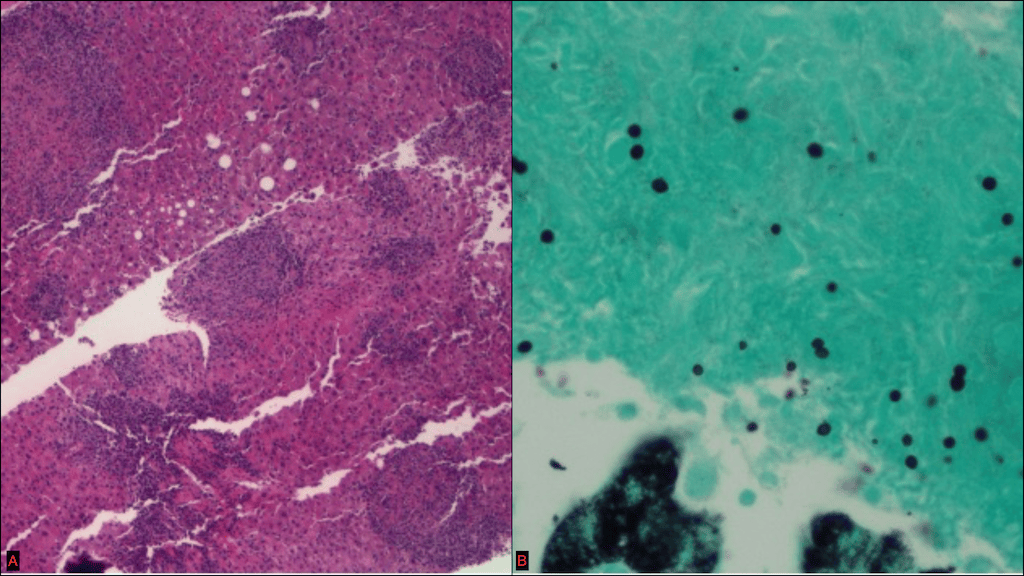
Figure: Figure 2A. Necrotizing granuloma (H&E)
Figure 2B. Histoplasma microorganisms (PAS)
Disclosures:
Mena Saad indicated no relevant financial relationships.
Medora Rodrigues indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Ronaldo Gnass indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Mena Saad, DO1, Medora Doris. Rodrigues, MD, MPH2, Jonathan Scott, MD3, Ronaldo Gnass, MD1, Khalid Mumtaz, MBBS, MSc2, Wichit Srikureja, MD4. P3932 - A Rare Complication of TNF-α Inhibitor With Histoplasmosis Associated Necrotizing Granulomatous Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mena Saad, DO1, Medora Doris. Rodrigues, MD, MPH2, Jonathan Scott, MD3, Ronaldo Gnass, MD1, Khalid Mumtaz, MBBS, MSc2, Wichit Srikureja, MD4
1Riverside University Health System, Moreno Valley, CA; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Riverside University Health System, Riverside, CA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Histoplasma capsulatum is a dimorphic fungus endemic to the central and eastern U.S. Disseminated histoplasmosis, its most severe form, can rarely cause necrotizing granulomatous hepatitis. Clinical presentation includes fever, malaise, jaundice, abdominal pain, and cholestatic liver enzyme abnormalities.
Case Description/
Methods: A 62-year-old man from Mexico with rheumatoid arthritis, previously on infliximab, was admitted with abdominal pain. He was febrile at 102.7°F and tachycardic. Physical examination showed icterus; right upper quadrant tenderness without guarding; and without hepato-splenomegaly. Initial labs showed elevated liver tests (LFTs): total bilirubin 2.5 mg/dL, alkaline phosphatase 284 U/L, AST 132 U/L, ALT 311 U/L. CT chest showed diffuse ground glass opacities and mediastinal adenopathy. Ultrasound showed gallstones and normal bile duct size. Endoscopic ultrasound (EUS) was done and showed gallstones and normal CBD with sludge. ERCP with biliary sphincterotomy and stent placement was done. However, LFTs elevation persisted. EUS guided liver biopsy was then undertaken with preliminary finding of necrotizing granulomatous hepatitis. Infectious workup revealed a positive QuantiFERON Gold and coccidioidomycosis serology. He was started and discharged on anti-tuberculosis regimen and fluconazole. However, his LFTs continue to be elevated. Final liver pathology demonstrated numerous intracellular yeasts with halos, consistent with Histoplasma capsulatum (Fig. 1&2). Positive coccidioidomycosis serology was thought to reflect cross-reactivity with histoplasma antigens. He was readmitted and started on liposomal amphotericin B. His anti-tuberculosis regimen was consolidated. Fluconazole was stopped. LFTs normalized within 2 days. He was discharged with itraconazole for 12 months.
Discussion: Histoplasmosis associated necrotizing granulomatous hepatitis is a rare complication in patients on tumor necrosis factor-α inhibitor. Disseminated histoplasmosis often occurs in immunosuppressed patients. Symptoms usually are organ specific and can include fever, fatigue, and weight loss. Hepatic involvement with elevated liver tests can mimic other liver and biliary diseases. The diagnosis is often based on antigen testing and/or histopathology. Our case illustrated a rare disseminated histoplasmosis associated with necrotizing granulomatous hepatitis confirmed on liver pathology. We believe that high index of suspicion combined with early liver biopsy led to a favorable outcome in our case.
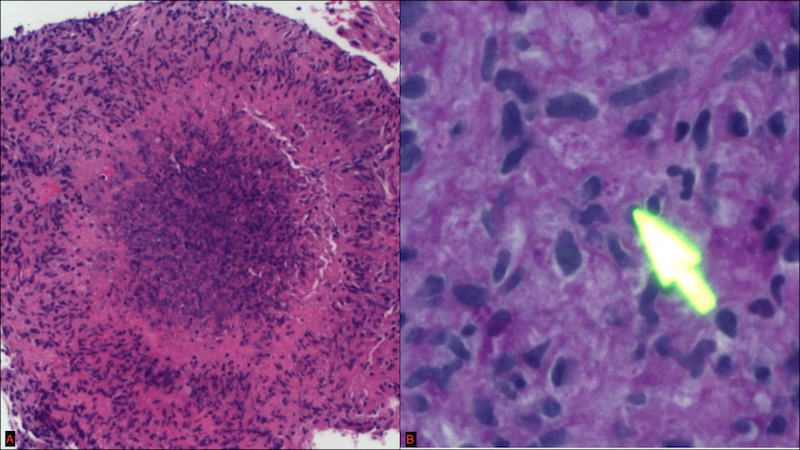
Figure: Figure 1A. Granulomatous hepatitis (H&E)
Figure 1B. Histoplasma microorganisms-budding yeasts (GMS)
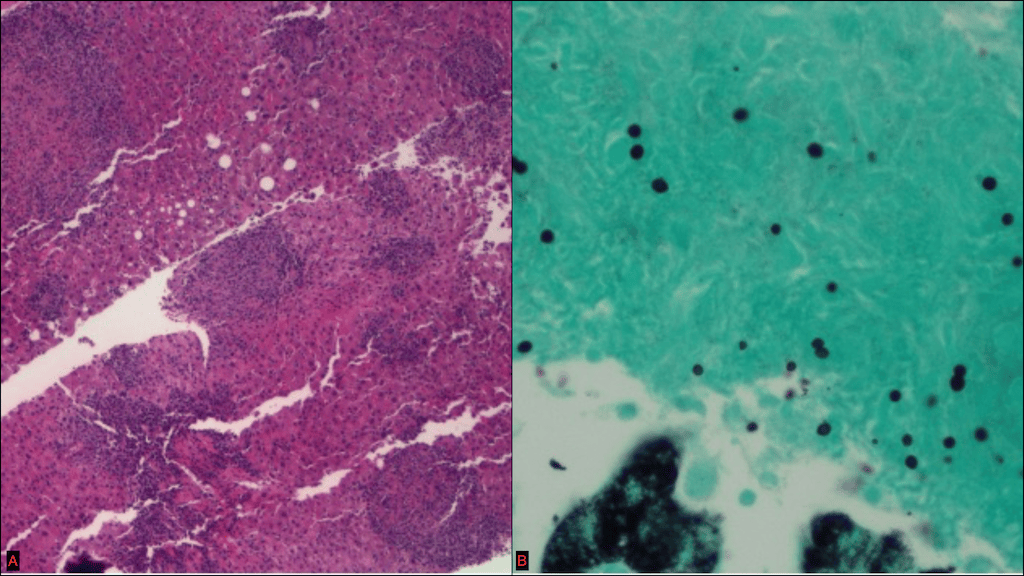
Figure: Figure 2A. Necrotizing granuloma (H&E)
Figure 2B. Histoplasma microorganisms (PAS)
Disclosures:
Mena Saad indicated no relevant financial relationships.
Medora Rodrigues indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Ronaldo Gnass indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Mena Saad, DO1, Medora Doris. Rodrigues, MD, MPH2, Jonathan Scott, MD3, Ronaldo Gnass, MD1, Khalid Mumtaz, MBBS, MSc2, Wichit Srikureja, MD4. P3932 - A Rare Complication of TNF-α Inhibitor With Histoplasmosis Associated Necrotizing Granulomatous Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

