Monday Poster Session
Category: Liver
P3927 - Esophageal Variceal Bleeding: An Uncommon Manifestation of Hepatic Sarcoidosis-Induced Portal Hypertension
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Gabriel Sperling, MD
University of North Carolina Hospitals
Chapel Hill, NC
Presenting Author(s)
Gabriel Sperling, MD1, Alisa Siebrasse, MD1, Amy Brownlee, MD2, Alfred S.. Barritt, MD, MPH1
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of North Carolina at Chapel Hill, Chapel Hill, NC
Introduction: Sarcoidosis is a multisystem granulomatous disorder that affects the lungs most commonly, however liver, skin, and cardiac manifestations are well described. Manifestations of hepatic involvement range from asymptomatic with only biochemical abnormalities to severe including portal hypertension with or without cirrhosis. Here, we present a case of hepatic sarcoidosis manifesting as non-cirrhotic portal hypertension with variceal bleeding.
Case Description/
Methods: Patient is a 59 year-old male with Graves’ disease, pulmonary sarcoidosis (off all medication), hypertension, and CKD3 who presented with hematemesis. Importantly, he also has a history of unexplored cholestatic liver enzyme elevation. Notable labs on admission included hemoglobin of 9g/dL (baseline 11-12g/dL), creatinine 1.94mg/dL (baseline 1.5mg/dL), and AST/ALT/ALP U/L were 75/101/422 U/L respectively. An emergent EGD revealed large ( >5mm) esophageal varices, of which 4 were banded. Relevant infectious/serologic workup include an unremarkable hepatitis panel, alcohol level, ferritin, ceruloplasmin, and antimitochondrial antibody. Antinuclear antibody (1:640) and anti-smooth muscle antibody (1:80) were both positive. MRCP showed diffusely heterogenous enhancement of the liver parenchyma with central peribiliary wall thickening and enhancement. He underwent a percutaneous liver biopsy, with pathology demonstrating non-necrotizing granulomas with surrounding chronic inflammation and fibrosis. The pattern of infiltrate is compatible with hepatic sarcoidosis in this clinical context. Notably, there was no cirrhosis identified on the biopsy. A multidisciplinary discussion is underway between GI and pulmonology regarding treatment, preliminarily favoring initiation of mycophenolate.
Discussion: We highlight the importance of maintaining a broad differential for portal hypertension, including non-cirrhotic etiologies such as hepatic sarcoidosis. Symptomatic hepatic sarcoid typically presents with abdominal pain, pruritus, and hepatomegaly, with portal hypertension serving as a much less common manifestation. Liver biopsy is recommended for those with moderate or severe liver enzyme abnormalities or when diagnostic confirmation is needed. Timely identification of hepatic involvement is key to prevent potential disease progression. Some experts propose that patients with symptomatic hepatic sarcoidosis receive prednisone, however further studies are warranted to determine an optimal treatment regimen for hepatic sarcoidosis.
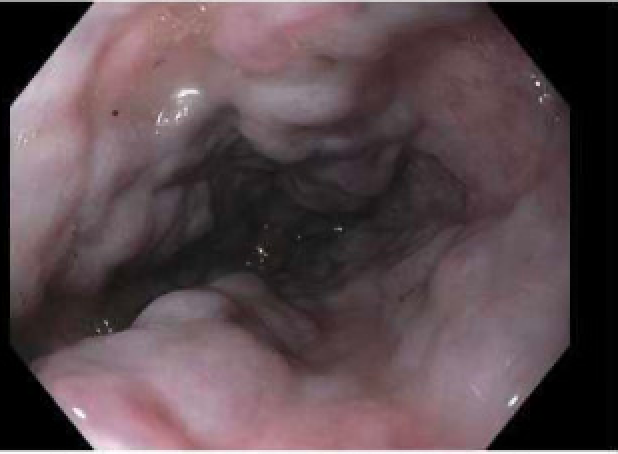
Figure: a) Large esophageal varices in the mid to distal esophagus

Figure: b) Non-caseating granulomas with surrounding chronic inflammation and fibrosis; high power H&E
Disclosures:
Gabriel Sperling indicated no relevant financial relationships.
Alisa Siebrasse indicated no relevant financial relationships.
Amy Brownlee indicated no relevant financial relationships.
Alfred Barritt indicated no relevant financial relationships.
Gabriel Sperling, MD1, Alisa Siebrasse, MD1, Amy Brownlee, MD2, Alfred S.. Barritt, MD, MPH1. P3927 - Esophageal Variceal Bleeding: An Uncommon Manifestation of Hepatic Sarcoidosis-Induced Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of North Carolina at Chapel Hill, Chapel Hill, NC
Introduction: Sarcoidosis is a multisystem granulomatous disorder that affects the lungs most commonly, however liver, skin, and cardiac manifestations are well described. Manifestations of hepatic involvement range from asymptomatic with only biochemical abnormalities to severe including portal hypertension with or without cirrhosis. Here, we present a case of hepatic sarcoidosis manifesting as non-cirrhotic portal hypertension with variceal bleeding.
Case Description/
Methods: Patient is a 59 year-old male with Graves’ disease, pulmonary sarcoidosis (off all medication), hypertension, and CKD3 who presented with hematemesis. Importantly, he also has a history of unexplored cholestatic liver enzyme elevation. Notable labs on admission included hemoglobin of 9g/dL (baseline 11-12g/dL), creatinine 1.94mg/dL (baseline 1.5mg/dL), and AST/ALT/ALP U/L were 75/101/422 U/L respectively. An emergent EGD revealed large ( >5mm) esophageal varices, of which 4 were banded. Relevant infectious/serologic workup include an unremarkable hepatitis panel, alcohol level, ferritin, ceruloplasmin, and antimitochondrial antibody. Antinuclear antibody (1:640) and anti-smooth muscle antibody (1:80) were both positive. MRCP showed diffusely heterogenous enhancement of the liver parenchyma with central peribiliary wall thickening and enhancement. He underwent a percutaneous liver biopsy, with pathology demonstrating non-necrotizing granulomas with surrounding chronic inflammation and fibrosis. The pattern of infiltrate is compatible with hepatic sarcoidosis in this clinical context. Notably, there was no cirrhosis identified on the biopsy. A multidisciplinary discussion is underway between GI and pulmonology regarding treatment, preliminarily favoring initiation of mycophenolate.
Discussion: We highlight the importance of maintaining a broad differential for portal hypertension, including non-cirrhotic etiologies such as hepatic sarcoidosis. Symptomatic hepatic sarcoid typically presents with abdominal pain, pruritus, and hepatomegaly, with portal hypertension serving as a much less common manifestation. Liver biopsy is recommended for those with moderate or severe liver enzyme abnormalities or when diagnostic confirmation is needed. Timely identification of hepatic involvement is key to prevent potential disease progression. Some experts propose that patients with symptomatic hepatic sarcoidosis receive prednisone, however further studies are warranted to determine an optimal treatment regimen for hepatic sarcoidosis.
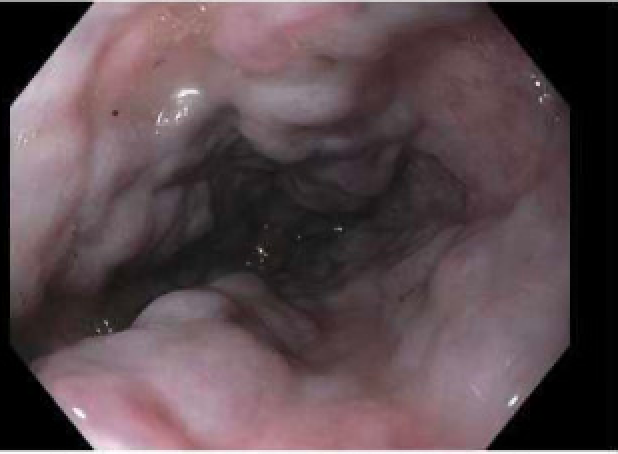
Figure: a) Large esophageal varices in the mid to distal esophagus

Figure: b) Non-caseating granulomas with surrounding chronic inflammation and fibrosis; high power H&E
Disclosures:
Gabriel Sperling indicated no relevant financial relationships.
Alisa Siebrasse indicated no relevant financial relationships.
Amy Brownlee indicated no relevant financial relationships.
Alfred Barritt indicated no relevant financial relationships.
Gabriel Sperling, MD1, Alisa Siebrasse, MD1, Amy Brownlee, MD2, Alfred S.. Barritt, MD, MPH1. P3927 - Esophageal Variceal Bleeding: An Uncommon Manifestation of Hepatic Sarcoidosis-Induced Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
