Monday Poster Session
Category: Liver
P3911 - Atypical Presentation of Acute EBV Hepatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cinthia Reyes Cruz, MD
University of Miami Miller School of Medicine at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Cinthia Reyes Cruz, MD1, Wisam Zakko, MD2
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2Gastroenterology Institute Of Fort Lauderdale, Fort Lauderdale, FL
Introduction: Acute viral hepatitis syndrome with a prodrome of fever, malaise, anorexia, and marked elevations in serum aminotransferases of 10 to 40 times the upper limit of normal is typically caused by hepatotropic viruses A to E. In contrast Epstein-Barr virus (EBV) related hepatitis typically manifests with transaminase elevations of less than 10 times normal, is always associated with lymphocytosis with the presence of atypical lymphocytes and often accompanied by mononucleosis features of lymphadenopathy and pharyngitis. We present a case of acute EBV hepatitis presenting with a clinical and biochemical profile characteristic of hepatotropic viral hepatitis without any of the typical clinical or hematological features of infectious mononucleosis.
Case Description/
Methods: A 63-year-old woman with a medical history of diabetes, hypertension and chronic kidney disease presented to the emergency department with generalized weakness, fatigue, abdominal pain, nausea and loss of appetite for 2 weeks. She denied sore throat, alcohol use, recent travel, use of new medications or acetaminophen. No cervical lymphadenopathy or pharyngitis on exam. Initial labs revealed creatinine 2.38, AST 1223, ALT 1675, alkaline phosphatase 317, and total bilirubin 2.1. WBC 5.4, with a normal differential; no lymphocytosis or atypical lymphocytes (Table 1). Ultrasound of the abdomen was unremarkable.
Infectious and autoimmune hepatitis serologies were negative (Table 1). Further workup demonstrated positive EBV serologies (Table 1). On 4 week follow up transaminases and bilirubin were normal and the patient was asymptomatic.
Discussion: While hepatic involvement with mild elevation of transaminases is common with EBV, acute hepatitis is rare and seen in less than 1% of acute EBV infections. On review of the literature, all reported cases of EBV induced acute hepatitis had the typical hematologic findings of lymphocytosis and atypical lymphocytes which raise suspicion of EBV, and all had liver enzyme elevation of no more than 5-10 times normal. In our case, the presentation mimicked an acute viral hepatitis syndrome, classically related to hepatotropic viruses with significant transaminitis greater than 30 times the upper limit of normal, in the absence of typical mononucleosis features or hematologic abnormalities. Our case underscores the importance of considering EBV as a potential cause of acute viral hepatitis syndrome, even when the clinical and laboratory profile deviates from the classical presentation.
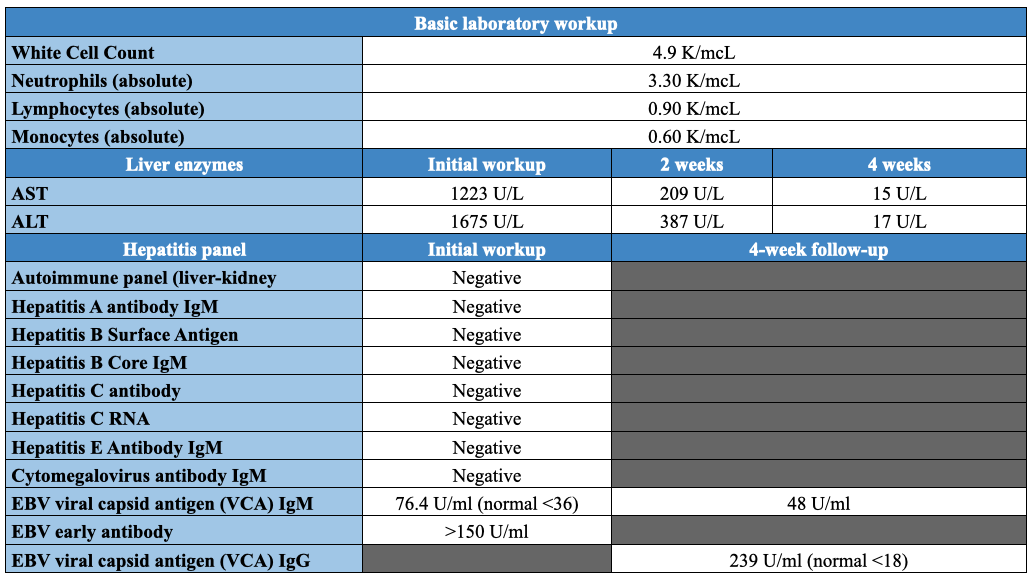
Figure: Table 1. Laboratory Workup
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Wisam Zakko indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Wisam Zakko, MD2. P3911 - Atypical Presentation of Acute EBV Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2Gastroenterology Institute Of Fort Lauderdale, Fort Lauderdale, FL
Introduction: Acute viral hepatitis syndrome with a prodrome of fever, malaise, anorexia, and marked elevations in serum aminotransferases of 10 to 40 times the upper limit of normal is typically caused by hepatotropic viruses A to E. In contrast Epstein-Barr virus (EBV) related hepatitis typically manifests with transaminase elevations of less than 10 times normal, is always associated with lymphocytosis with the presence of atypical lymphocytes and often accompanied by mononucleosis features of lymphadenopathy and pharyngitis. We present a case of acute EBV hepatitis presenting with a clinical and biochemical profile characteristic of hepatotropic viral hepatitis without any of the typical clinical or hematological features of infectious mononucleosis.
Case Description/
Methods: A 63-year-old woman with a medical history of diabetes, hypertension and chronic kidney disease presented to the emergency department with generalized weakness, fatigue, abdominal pain, nausea and loss of appetite for 2 weeks. She denied sore throat, alcohol use, recent travel, use of new medications or acetaminophen. No cervical lymphadenopathy or pharyngitis on exam. Initial labs revealed creatinine 2.38, AST 1223, ALT 1675, alkaline phosphatase 317, and total bilirubin 2.1. WBC 5.4, with a normal differential; no lymphocytosis or atypical lymphocytes (Table 1). Ultrasound of the abdomen was unremarkable.
Infectious and autoimmune hepatitis serologies were negative (Table 1). Further workup demonstrated positive EBV serologies (Table 1). On 4 week follow up transaminases and bilirubin were normal and the patient was asymptomatic.
Discussion: While hepatic involvement with mild elevation of transaminases is common with EBV, acute hepatitis is rare and seen in less than 1% of acute EBV infections. On review of the literature, all reported cases of EBV induced acute hepatitis had the typical hematologic findings of lymphocytosis and atypical lymphocytes which raise suspicion of EBV, and all had liver enzyme elevation of no more than 5-10 times normal. In our case, the presentation mimicked an acute viral hepatitis syndrome, classically related to hepatotropic viruses with significant transaminitis greater than 30 times the upper limit of normal, in the absence of typical mononucleosis features or hematologic abnormalities. Our case underscores the importance of considering EBV as a potential cause of acute viral hepatitis syndrome, even when the clinical and laboratory profile deviates from the classical presentation.
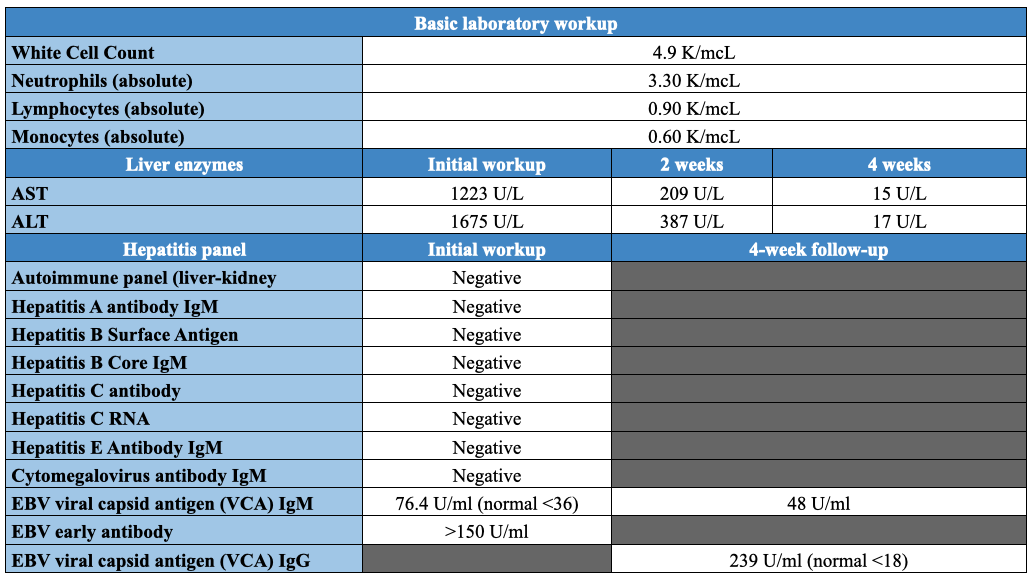
Figure: Table 1. Laboratory Workup
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Wisam Zakko indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Wisam Zakko, MD2. P3911 - Atypical Presentation of Acute EBV Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
