Monday Poster Session
Category: Liver
P3883 - Acute Myelomonocytic Leukemia Following Liver Transplantation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sirisha Gaddipati, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Sneha Akurati, BS1, Sirisha Gaddipati, MD1, Sunny Sandhu, MD2, Felipe Camacho-Cordovez, MD1, Ping Yang, PhD1, Eric F. Martin, MD3
1University of Miami Miller School of Medicine, Miami, FL; 2Stanford University, Palo Alto, CA; 3University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL
Introduction: Hematologic malignancies are uncommon but serious complications following solid organ transplantation, with acute myeloid leukemia (AML) being particularly rare. Among AML subtypes, acute myelomonocytic leukemia (AMML) is scarcely reported after liver transplantation (LT), and its pathogenesis and optimal management in this context remain poorly defined. We present a case of AMML which was successfully treated with early recognition and prompt therapy.
Case Description/
Methods: A 67-year-old male with history of MetALD cirrhosis complicated by hepatocellular carcinoma (treated with locoregional therapies) with history of LT 7 months prior with uncomplicated post-transplant course, who was admitted for evaluation of acute onset chest pain. Workup for cardiac and pulmonary etiologies was unremarkable. Laboratory workup showed WBC 15,800 cells/µL, ALT 23 U/L, AST 24 U/L, ALP 102 IU/L, and total bilirubin 0.8 mg/dL. WBC progressively increased despite empiric antimicrobials and broad infectious workup, with hospital WBC 54,700 cells/µL, with differential showing 61% monocytes on hospital day #14. Bone marrow biopsy was performed which showed findings consistent with favorable risk NPM 1-mutated AMML, with 61% blasts (Figure 1). Chromosome karyotype identified a pericentric inversion involving chromosome 4. (Figure 2). He was treated with cytarabine and daunorubicin (7+3 induction), with successful remission, with consolidation treatment with high dose cytarabine. Immunosuppression with tacrolimus was closely managed in conjunction with transplant hepatology, and liver graft function remained stable throughout. He remains clinically well with no evidence of recurrence.
Discussion: Malignancy is a well-established long-term complication of SOT. While hematologic cancers—including post-transplant lymphoproliferative disorders—are relatively more common, neoplasms such AML remain rare, with the AMML subtype seldom reported in LT recipients. Pathogenesis is likely multifactorial, involving cumulative immunosuppressive exposure, viral oncogenesis, and genetic instability. This case underscores the importance of early recognition and prompt therapy of hematologic abnormalities in LT recipients and demonstrates that favorable-risk AMML can be successfully treated with curative intent, even in the setting of immunosuppression for recent LT. Close surveillance and multidisciplinary care are critical in optimizing outcomes for this rare post-transplant complication.
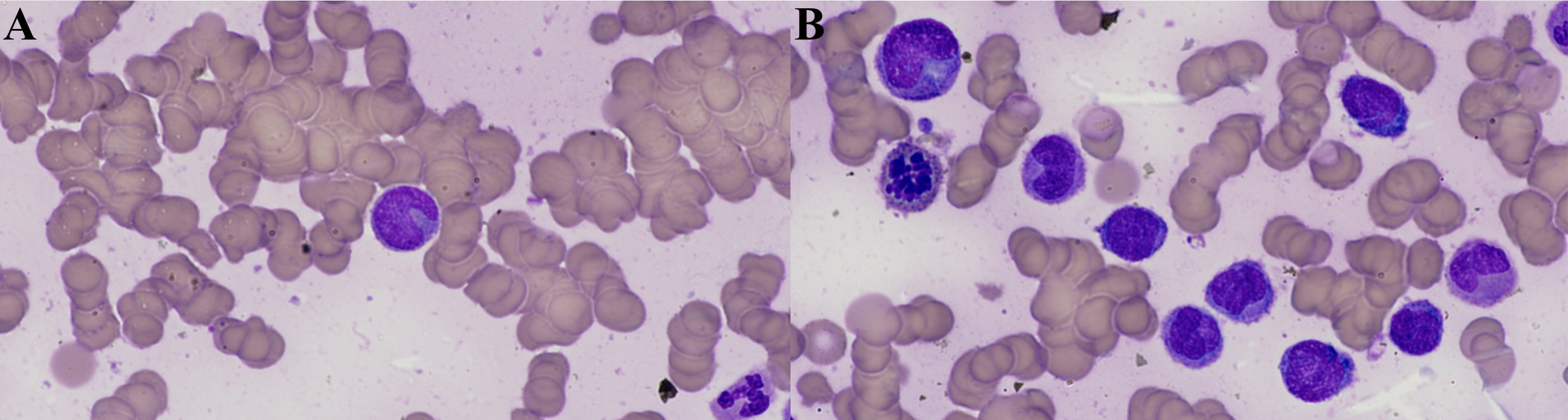
Figure: Figure 1: Bone marrow smear (Giemsa, 100x, A) showing blasts with cup-like nuclear morphology, characteristic of AML with NPM1 mutation (Giemsa). Blasts, myeloid series, and scattered dyspoiesis (B).

Figure: Figure 2: Chromosome karyotype image obtained from G-banded analysis of a bone marrow sample from the patient. A pericentric inversion involving one chromosome 4 was identified in all 20 of the 20 cells examined. Arrows indicate the breakpoints on the inverted chromosome 4, located at bands p14 and q31. The homologous chromosome 4 (left) and all other chromosomes appeared normal. Karyotype nomenclature: 46,XY,inv(4)(p14q31). Banding resolution: 300 bands.
Disclosures:
Sneha Akurati indicated no relevant financial relationships.
Sirisha Gaddipati indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Felipe Camacho-Cordovez indicated no relevant financial relationships.
Ping Yang indicated no relevant financial relationships.
Eric Martin indicated no relevant financial relationships.
Sneha Akurati, BS1, Sirisha Gaddipati, MD1, Sunny Sandhu, MD2, Felipe Camacho-Cordovez, MD1, Ping Yang, PhD1, Eric F. Martin, MD3. P3883 - Acute Myelomonocytic Leukemia Following Liver Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2Stanford University, Palo Alto, CA; 3University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL
Introduction: Hematologic malignancies are uncommon but serious complications following solid organ transplantation, with acute myeloid leukemia (AML) being particularly rare. Among AML subtypes, acute myelomonocytic leukemia (AMML) is scarcely reported after liver transplantation (LT), and its pathogenesis and optimal management in this context remain poorly defined. We present a case of AMML which was successfully treated with early recognition and prompt therapy.
Case Description/
Methods: A 67-year-old male with history of MetALD cirrhosis complicated by hepatocellular carcinoma (treated with locoregional therapies) with history of LT 7 months prior with uncomplicated post-transplant course, who was admitted for evaluation of acute onset chest pain. Workup for cardiac and pulmonary etiologies was unremarkable. Laboratory workup showed WBC 15,800 cells/µL, ALT 23 U/L, AST 24 U/L, ALP 102 IU/L, and total bilirubin 0.8 mg/dL. WBC progressively increased despite empiric antimicrobials and broad infectious workup, with hospital WBC 54,700 cells/µL, with differential showing 61% monocytes on hospital day #14. Bone marrow biopsy was performed which showed findings consistent with favorable risk NPM 1-mutated AMML, with 61% blasts (Figure 1). Chromosome karyotype identified a pericentric inversion involving chromosome 4. (Figure 2). He was treated with cytarabine and daunorubicin (7+3 induction), with successful remission, with consolidation treatment with high dose cytarabine. Immunosuppression with tacrolimus was closely managed in conjunction with transplant hepatology, and liver graft function remained stable throughout. He remains clinically well with no evidence of recurrence.
Discussion: Malignancy is a well-established long-term complication of SOT. While hematologic cancers—including post-transplant lymphoproliferative disorders—are relatively more common, neoplasms such AML remain rare, with the AMML subtype seldom reported in LT recipients. Pathogenesis is likely multifactorial, involving cumulative immunosuppressive exposure, viral oncogenesis, and genetic instability. This case underscores the importance of early recognition and prompt therapy of hematologic abnormalities in LT recipients and demonstrates that favorable-risk AMML can be successfully treated with curative intent, even in the setting of immunosuppression for recent LT. Close surveillance and multidisciplinary care are critical in optimizing outcomes for this rare post-transplant complication.
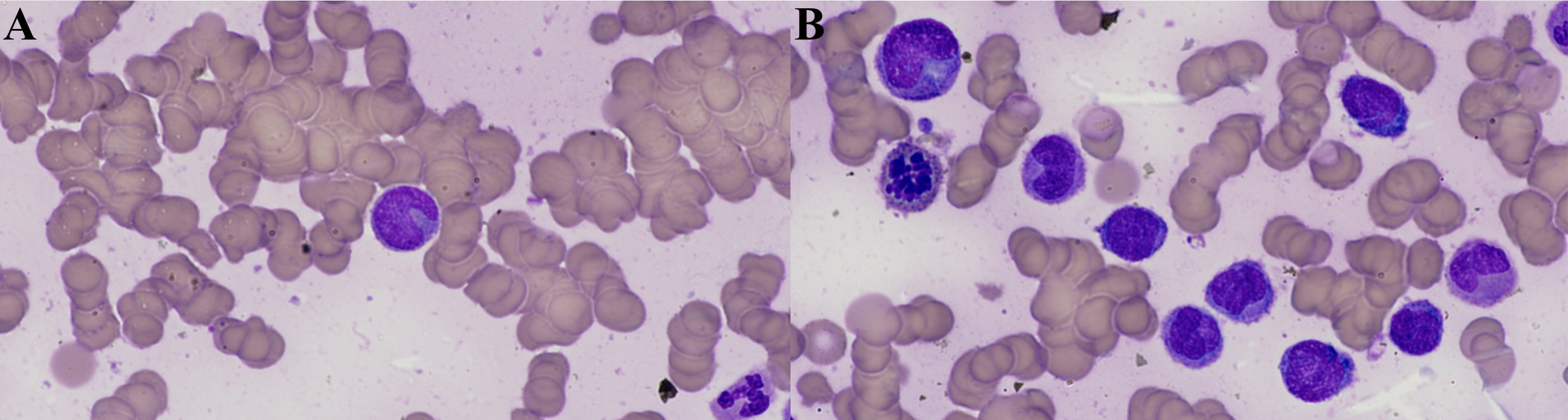
Figure: Figure 1: Bone marrow smear (Giemsa, 100x, A) showing blasts with cup-like nuclear morphology, characteristic of AML with NPM1 mutation (Giemsa). Blasts, myeloid series, and scattered dyspoiesis (B).

Figure: Figure 2: Chromosome karyotype image obtained from G-banded analysis of a bone marrow sample from the patient. A pericentric inversion involving one chromosome 4 was identified in all 20 of the 20 cells examined. Arrows indicate the breakpoints on the inverted chromosome 4, located at bands p14 and q31. The homologous chromosome 4 (left) and all other chromosomes appeared normal. Karyotype nomenclature: 46,XY,inv(4)(p14q31). Banding resolution: 300 bands.
Disclosures:
Sneha Akurati indicated no relevant financial relationships.
Sirisha Gaddipati indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Felipe Camacho-Cordovez indicated no relevant financial relationships.
Ping Yang indicated no relevant financial relationships.
Eric Martin indicated no relevant financial relationships.
Sneha Akurati, BS1, Sirisha Gaddipati, MD1, Sunny Sandhu, MD2, Felipe Camacho-Cordovez, MD1, Ping Yang, PhD1, Eric F. Martin, MD3. P3883 - Acute Myelomonocytic Leukemia Following Liver Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
