Monday Poster Session
Category: Liver
P3851 - Acute Liver Failure Following Wild Mushroom Ingestion: A Case of Suspected Amanita Toxicity Managed With Silibinin and N-Acetylcysteine
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Krishna Kothamasu, DO (he/him/his)
Jefferson Torresdale Hospital
Philadelphia, PA
Presenting Author(s)
Krishna Kothamasu, DO1, Michelle Joyner, DO, MS2, Ashley Gault, DO1, Kashif Tufail, MD3
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Jefferson Northeast Hospital, Philadelphia, PA; 3Northeast Gastroenterology Associates, Philadelphia, PA
Introduction: Amanita phalloides, or “death cap”, is a lethal wild mushroom known to cause fulminant hepatic failure due to amatoxins that inhibit RNA polymerase II. Mortality remains high without prompt management. This is a case of suspected amatoxin induced acute liver failure (ALF) managed with N-acetylcysteine (NAC) and Silibinin, an experimental therapy showing promise in inhibiting hepatic toxin uptake and reducing morbidity and mortality.
Case Description/
Methods: A 34-year-old Arabic-speaking female with no significant medical history presented with epigastric pain, nausea, non-bloody, non-bilious emesis, and diarrhea eight hours after ingesting mushrooms resembling white button-caps, foraged from a park in northeast Philadelphia. Eight family members developed similar symptoms (three with ALF) after ingestion. Initial labs revealed mild alkaline phosphatase elevation (118 U/L) with normal transaminases, bilirubin, and coagulation profile. Ultrasound abdomen with doppler was unrevealing. Poison Control recommended supportive management and activated charcoal.
By day two, AST rose to 277 U/L and ALT to 89 U/L. Given persistent gastrointestinal (GI) symptoms and rising liver enzymes, per Poison Control, N-acetylcysteine (NAC) and Silibinin (obtained via FDA expanded access) were initiated. Hepatology was consulted for concern of early-stage ALF. She remained without neurologic symptoms and was monitored with serial labs.
By day four, liver function deteriorated with AST and ALT peaked at 5,186 and 2,668 U/L respectively. Coagulation studies worsened (INR 2.19, PT 24.9), prompting hepatology consultation and transfer planning for liver transplant evaluation. Despite the severity, she improved by day five with down-trending LFTs and resolution of GI symptoms. NAC and Silabinin were discontinued once INR was below 1.5. Further work up for viral, autoimmune, and metabolic liver disease were unremarkable. Liver transplant evaluation was cancelled and she was discharged on day six with outpatient hepatology follow-up. Repeat labs six months later confirmed normalized liver enzymes.
Discussion: This case illustrates the importance of prompt suspicion of Amanita toxin induced ALF and early initiation of Silibinin. Though it is only investigational and not FDA-approved, Silibinin in conjunction with NAC, halted hepatocellular toxin uptake and prevented progression of ALF to transplant. This case adds to the evidence supporting Silibinin as a therapeutic in early management of amatoxin-related hepatotoxicity.
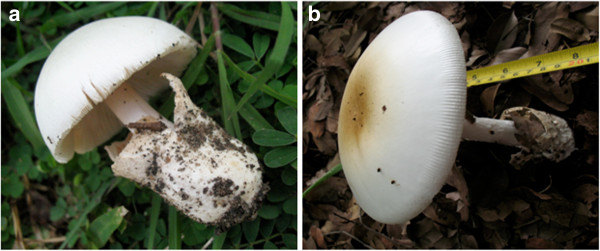
Figure: Wild mushroom species which appear similar: (a) An edible Volvariella volvacea (paddy straw mushroom); (b) A deadly poisonous Amanita phalloides (death cap). (All photo taken by Tibuhwa DD in the field).
Disclosures:
Krishna Kothamasu indicated no relevant financial relationships.
Michelle Joyner indicated no relevant financial relationships.
Ashley Gault indicated no relevant financial relationships.
Kashif Tufail indicated no relevant financial relationships.
Krishna Kothamasu, DO1, Michelle Joyner, DO, MS2, Ashley Gault, DO1, Kashif Tufail, MD3. P3851 - Acute Liver Failure Following Wild Mushroom Ingestion: A Case of Suspected Amanita Toxicity Managed With Silibinin and N-Acetylcysteine, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Jefferson Northeast Hospital, Philadelphia, PA; 3Northeast Gastroenterology Associates, Philadelphia, PA
Introduction: Amanita phalloides, or “death cap”, is a lethal wild mushroom known to cause fulminant hepatic failure due to amatoxins that inhibit RNA polymerase II. Mortality remains high without prompt management. This is a case of suspected amatoxin induced acute liver failure (ALF) managed with N-acetylcysteine (NAC) and Silibinin, an experimental therapy showing promise in inhibiting hepatic toxin uptake and reducing morbidity and mortality.
Case Description/
Methods: A 34-year-old Arabic-speaking female with no significant medical history presented with epigastric pain, nausea, non-bloody, non-bilious emesis, and diarrhea eight hours after ingesting mushrooms resembling white button-caps, foraged from a park in northeast Philadelphia. Eight family members developed similar symptoms (three with ALF) after ingestion. Initial labs revealed mild alkaline phosphatase elevation (118 U/L) with normal transaminases, bilirubin, and coagulation profile. Ultrasound abdomen with doppler was unrevealing. Poison Control recommended supportive management and activated charcoal.
By day two, AST rose to 277 U/L and ALT to 89 U/L. Given persistent gastrointestinal (GI) symptoms and rising liver enzymes, per Poison Control, N-acetylcysteine (NAC) and Silibinin (obtained via FDA expanded access) were initiated. Hepatology was consulted for concern of early-stage ALF. She remained without neurologic symptoms and was monitored with serial labs.
By day four, liver function deteriorated with AST and ALT peaked at 5,186 and 2,668 U/L respectively. Coagulation studies worsened (INR 2.19, PT 24.9), prompting hepatology consultation and transfer planning for liver transplant evaluation. Despite the severity, she improved by day five with down-trending LFTs and resolution of GI symptoms. NAC and Silabinin were discontinued once INR was below 1.5. Further work up for viral, autoimmune, and metabolic liver disease were unremarkable. Liver transplant evaluation was cancelled and she was discharged on day six with outpatient hepatology follow-up. Repeat labs six months later confirmed normalized liver enzymes.
Discussion: This case illustrates the importance of prompt suspicion of Amanita toxin induced ALF and early initiation of Silibinin. Though it is only investigational and not FDA-approved, Silibinin in conjunction with NAC, halted hepatocellular toxin uptake and prevented progression of ALF to transplant. This case adds to the evidence supporting Silibinin as a therapeutic in early management of amatoxin-related hepatotoxicity.
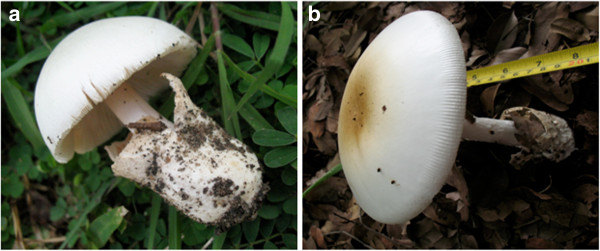
Figure: Wild mushroom species which appear similar: (a) An edible Volvariella volvacea (paddy straw mushroom); (b) A deadly poisonous Amanita phalloides (death cap). (All photo taken by Tibuhwa DD in the field).
Disclosures:
Krishna Kothamasu indicated no relevant financial relationships.
Michelle Joyner indicated no relevant financial relationships.
Ashley Gault indicated no relevant financial relationships.
Kashif Tufail indicated no relevant financial relationships.
Krishna Kothamasu, DO1, Michelle Joyner, DO, MS2, Ashley Gault, DO1, Kashif Tufail, MD3. P3851 - Acute Liver Failure Following Wild Mushroom Ingestion: A Case of Suspected Amanita Toxicity Managed With Silibinin and N-Acetylcysteine, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
