Monday Poster Session
Category: Liver
P3845 - A Case Series on the Intersection of Cirrhosis, Bariatric Surgery, and Urea Cycle Dysfunction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mustafa Shah, MD
Geisinger Health System
Danville, PA
Presenting Author(s)
Mustafa Shah, MD, Deepa Kumarjiguda, DO, Syed Hassan, MD, Alberto Unzueta, MD
Geisinger Health System, Danville, PA
Introduction: Urea cycle disorders (UCDs) are rare inborn errors of metabolism that impair ammonia detoxification, causing hyperammonemia (HA), leading to severe neurological damage and death if untreated. The urea cycle comprises five key enzymes, and defects in any can result in varying severity, from neonatal to adult onset. Diagnosis relies on biochemical markers, genetic testing, and ammonia levels. Treatment focuses on dietary management, nitrogen-scavenging drugs, and, in rare cases, transplantation. We present four patients with prior Roux-en-Y gastric bypass (RYGB) admitted for symptomatic HA.
Case Description/
Methods: Four female patients' status post RYGB presented with encephalopathy and were found to have elevated ammonia levels (112 - 256 umol/L) via venous blood samples. They were screened for underlying UCDs with plasma quantitative amino acid (AA) levels, molecular genetic testing, and urinary orotic acid levels. Infectious and other metabolic etiologies of encephalopathy were ruled out.
Two patients had a high glutamine-to-citrulline ratio, suggesting a proximal urea cycle deficit, whereas the other two patients had essential amino acid (AA) deficiencies. Of the two patients with AA deficiencies, the one with cirrhosis improved with nitrogen-scavenging drugs (lactulose and rifaximin).
Marked AA deficiencies impair ammonia detoxification despite preserved synthetic hepatic function. The patients improved with supportive therapy and nutritional repletion. The case of the patient with a history of recurrent HA encephalopathy and a negative genetic workup emphasizes the diagnostic challenge of adult-onset or partial UCD. However, the elevated glutamine-to-citrulline ratio pointed to a proximal UCD. The patient had clinical improvement following continuous renal replacement therapy.
Discussion: These cases highlight the complex interplay of liver dysfunction, altered GI anatomy, and UCD in the pathogenesis of HA in adults. These pathophysiologic processes independently contribute to the development of HA encephalopathy. The presence of RYGB reflects the existence of post-bariatric surgery hyperammonemia as a distinct clinical entity. The alteration of GI anatomy and microbiome increases bacterial urease activity and promotes protein malabsorption, contributing to increased ammonia production and reduced clearance. Evaluation of UCDs in cirrhotic and non-cirrhotic patients with RYGB can be considered as part of the evaluation of hepatic encephalopathy in this population.
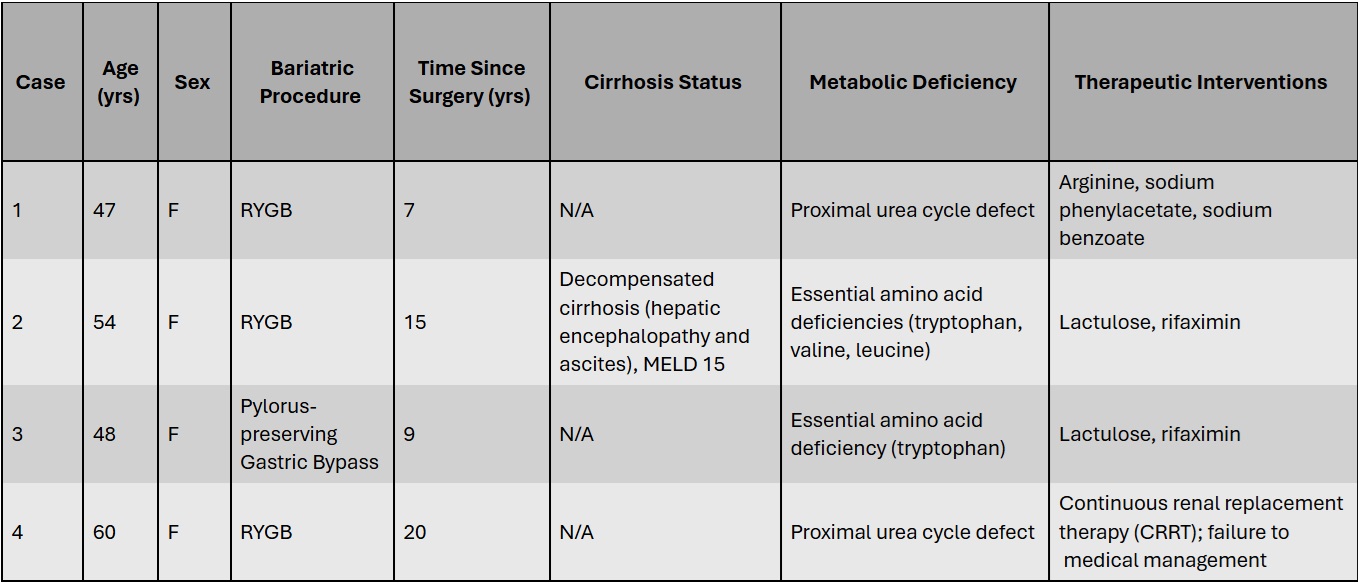
Figure: Table 1. Patient characteristics
Disclosures:
Mustafa Shah indicated no relevant financial relationships.
Deepa Kumarjiguda indicated no relevant financial relationships.
Syed Hassan indicated no relevant financial relationships.
Alberto Unzueta indicated no relevant financial relationships.
Mustafa Shah, MD, Deepa Kumarjiguda, DO, Syed Hassan, MD, Alberto Unzueta, MD. P3845 - A Case Series on the Intersection of Cirrhosis, Bariatric Surgery, and Urea Cycle Dysfunction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Geisinger Health System, Danville, PA
Introduction: Urea cycle disorders (UCDs) are rare inborn errors of metabolism that impair ammonia detoxification, causing hyperammonemia (HA), leading to severe neurological damage and death if untreated. The urea cycle comprises five key enzymes, and defects in any can result in varying severity, from neonatal to adult onset. Diagnosis relies on biochemical markers, genetic testing, and ammonia levels. Treatment focuses on dietary management, nitrogen-scavenging drugs, and, in rare cases, transplantation. We present four patients with prior Roux-en-Y gastric bypass (RYGB) admitted for symptomatic HA.
Case Description/
Methods: Four female patients' status post RYGB presented with encephalopathy and were found to have elevated ammonia levels (112 - 256 umol/L) via venous blood samples. They were screened for underlying UCDs with plasma quantitative amino acid (AA) levels, molecular genetic testing, and urinary orotic acid levels. Infectious and other metabolic etiologies of encephalopathy were ruled out.
Two patients had a high glutamine-to-citrulline ratio, suggesting a proximal urea cycle deficit, whereas the other two patients had essential amino acid (AA) deficiencies. Of the two patients with AA deficiencies, the one with cirrhosis improved with nitrogen-scavenging drugs (lactulose and rifaximin).
Marked AA deficiencies impair ammonia detoxification despite preserved synthetic hepatic function. The patients improved with supportive therapy and nutritional repletion. The case of the patient with a history of recurrent HA encephalopathy and a negative genetic workup emphasizes the diagnostic challenge of adult-onset or partial UCD. However, the elevated glutamine-to-citrulline ratio pointed to a proximal UCD. The patient had clinical improvement following continuous renal replacement therapy.
Discussion: These cases highlight the complex interplay of liver dysfunction, altered GI anatomy, and UCD in the pathogenesis of HA in adults. These pathophysiologic processes independently contribute to the development of HA encephalopathy. The presence of RYGB reflects the existence of post-bariatric surgery hyperammonemia as a distinct clinical entity. The alteration of GI anatomy and microbiome increases bacterial urease activity and promotes protein malabsorption, contributing to increased ammonia production and reduced clearance. Evaluation of UCDs in cirrhotic and non-cirrhotic patients with RYGB can be considered as part of the evaluation of hepatic encephalopathy in this population.
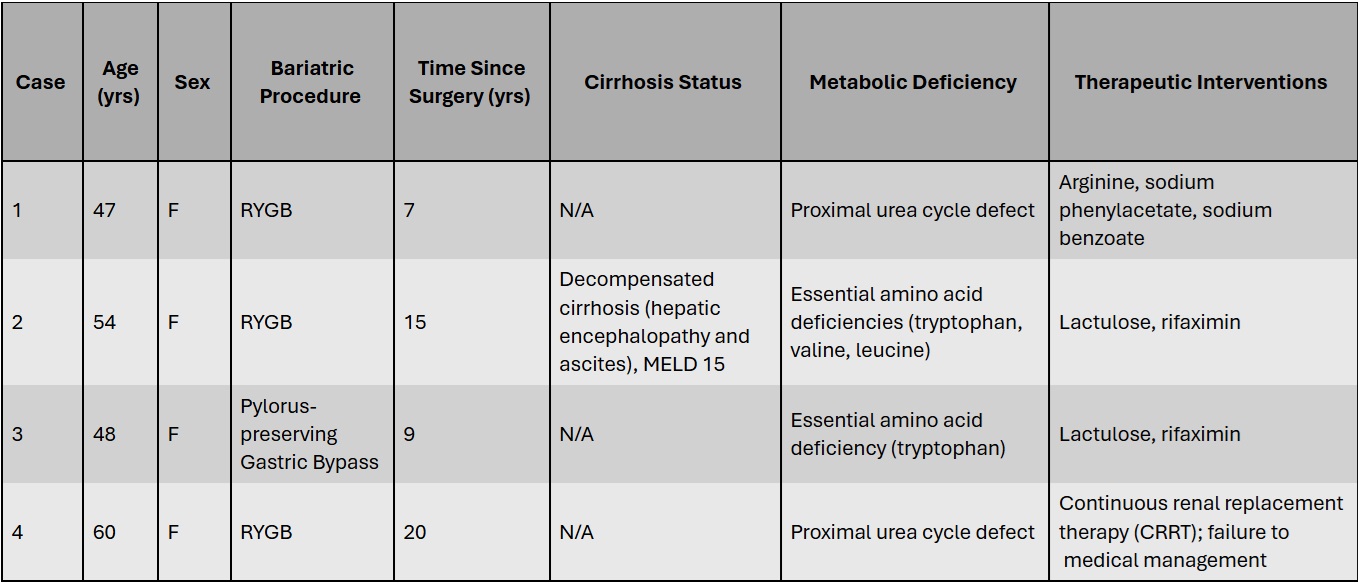
Figure: Table 1. Patient characteristics
Disclosures:
Mustafa Shah indicated no relevant financial relationships.
Deepa Kumarjiguda indicated no relevant financial relationships.
Syed Hassan indicated no relevant financial relationships.
Alberto Unzueta indicated no relevant financial relationships.
Mustafa Shah, MD, Deepa Kumarjiguda, DO, Syed Hassan, MD, Alberto Unzueta, MD. P3845 - A Case Series on the Intersection of Cirrhosis, Bariatric Surgery, and Urea Cycle Dysfunction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
