Monday Poster Session
Category: Liver
P3840 - Chronic Hepatitis E Infection: An Insidious Cause of Elevated Transaminases in a Patient with Solid Organ Transplant
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jenson Phung, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Award: ACG Presidential Poster Award
Jenson Phung, MD1, Morgan Freeman, MD1, Rahul Karna, MD2, Mary Thomson, MD, MS1
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Hepatitis E (HEV) is an RNA virus typically presenting as acute hepatitis in highly endemic regions of Asia and Africa. It has been rarely associated with chronic liver injury in low endemic regions such as the United States. We describe a case of HEV presenting as persistently elevated transaminases in a patient with renal transplant.
Case Description/
Methods: A 37-year-old female with history of anti-neutrophil cytoplasmic antibody vasculitis, minimal alcohol use, and two prior renal transplants 2 years and 17 years ago presented for evaluation of elevated transaminases. At the time of her referral, she had alanine transaminase in the 200s and aspartate transaminase in the 100s, both of which were previously normal. She also had mildly elevated direct bilirubin. Her INR, alkaline phosphatase, and platelets were all unremarkable. Her trimethoprim-sulfamethoxazole and atorvastatin were put on hold due to possibility of drug-induced liver injury. Part of her initial workup included testing for anti-nuclear antibodies, F-actin, iron panel, genetic testing for hemochromatosis, and an echocardiogram, all of which were normal. Ultrasound demonstrated normal liver echotexture without focal mass and normal bile ducts. Viral testing was negative for hepatitis A, B, and C, as well as cytomegalovirus and Epstein-Barr virus.
Transaminases continued to be elevated but stable on repeat, so a liver biopsy was pursued, which showed hepatitis of unclear etiology without evidence of fibrosis. After multidisciplinary discussion, the differential was expanded to include autoimmune hepatitis, as this could be consistent with the biopsy findings. However, the patient was already receiving immunosuppressive medication with tacrolimus and mycophenolate that would theoretically treat autoimmune hepatitis. As such, hepatitis E was then considered. Testing for HEV revealed positive IgG and IgM, as well as viral load of 100 million by PCR. Due to high donor-specific antibodies, the patient’s immunosuppression could not be decreased, so she was treated with ribavirin for 12 weeks. Transaminases normalized after 6 months, and HEV viral load was undetectable 3 months after treatment.
Discussion: HEV can be a problematic cause of transaminase elevations in patients with solid organ transplants, as chronic infection can lead to cirrhosis (Figure 1). Our case demonstrates the importance of including HEV testing for elevated transaminases evaluation in immunocompromised patients even in low endemic regions.
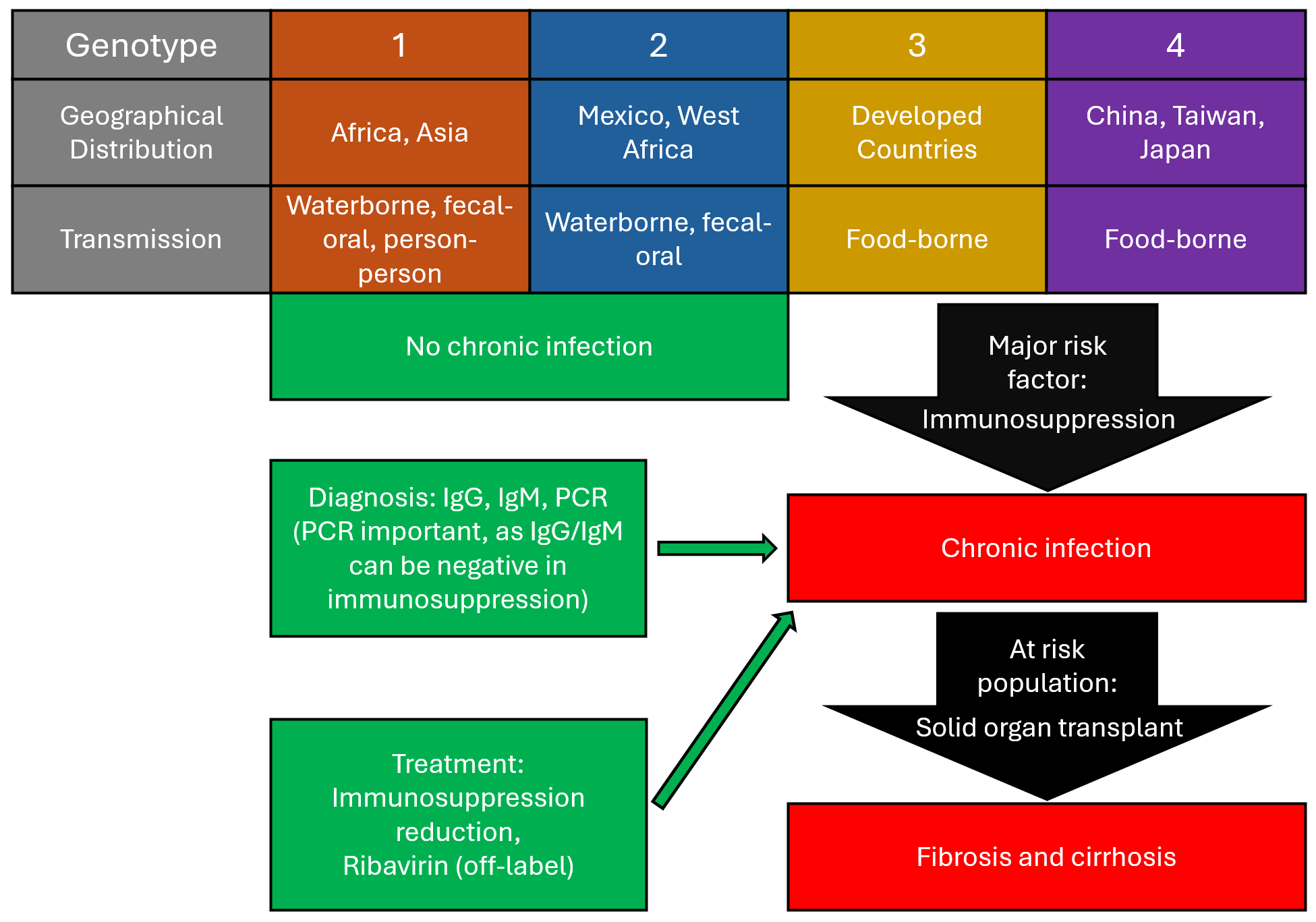
Figure: Figure 1. Summary of hepatitis E genotypes, diagnosis, treatment, and genotype 3/4 progression of disease based on data from Centers for Disease Control and the European Association for the Study of Liver Guidelines from 2018.
Disclosures:
Jenson Phung indicated no relevant financial relationships.
Morgan Freeman indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mary Thomson indicated no relevant financial relationships.
Jenson Phung, MD1, Morgan Freeman, MD1, Rahul Karna, MD2, Mary Thomson, MD, MS1. P3840 - Chronic Hepatitis E Infection: An Insidious Cause of Elevated Transaminases in a Patient with Solid Organ Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Jenson Phung, MD1, Morgan Freeman, MD1, Rahul Karna, MD2, Mary Thomson, MD, MS1
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Hepatitis E (HEV) is an RNA virus typically presenting as acute hepatitis in highly endemic regions of Asia and Africa. It has been rarely associated with chronic liver injury in low endemic regions such as the United States. We describe a case of HEV presenting as persistently elevated transaminases in a patient with renal transplant.
Case Description/
Methods: A 37-year-old female with history of anti-neutrophil cytoplasmic antibody vasculitis, minimal alcohol use, and two prior renal transplants 2 years and 17 years ago presented for evaluation of elevated transaminases. At the time of her referral, she had alanine transaminase in the 200s and aspartate transaminase in the 100s, both of which were previously normal. She also had mildly elevated direct bilirubin. Her INR, alkaline phosphatase, and platelets were all unremarkable. Her trimethoprim-sulfamethoxazole and atorvastatin were put on hold due to possibility of drug-induced liver injury. Part of her initial workup included testing for anti-nuclear antibodies, F-actin, iron panel, genetic testing for hemochromatosis, and an echocardiogram, all of which were normal. Ultrasound demonstrated normal liver echotexture without focal mass and normal bile ducts. Viral testing was negative for hepatitis A, B, and C, as well as cytomegalovirus and Epstein-Barr virus.
Transaminases continued to be elevated but stable on repeat, so a liver biopsy was pursued, which showed hepatitis of unclear etiology without evidence of fibrosis. After multidisciplinary discussion, the differential was expanded to include autoimmune hepatitis, as this could be consistent with the biopsy findings. However, the patient was already receiving immunosuppressive medication with tacrolimus and mycophenolate that would theoretically treat autoimmune hepatitis. As such, hepatitis E was then considered. Testing for HEV revealed positive IgG and IgM, as well as viral load of 100 million by PCR. Due to high donor-specific antibodies, the patient’s immunosuppression could not be decreased, so she was treated with ribavirin for 12 weeks. Transaminases normalized after 6 months, and HEV viral load was undetectable 3 months after treatment.
Discussion: HEV can be a problematic cause of transaminase elevations in patients with solid organ transplants, as chronic infection can lead to cirrhosis (Figure 1). Our case demonstrates the importance of including HEV testing for elevated transaminases evaluation in immunocompromised patients even in low endemic regions.
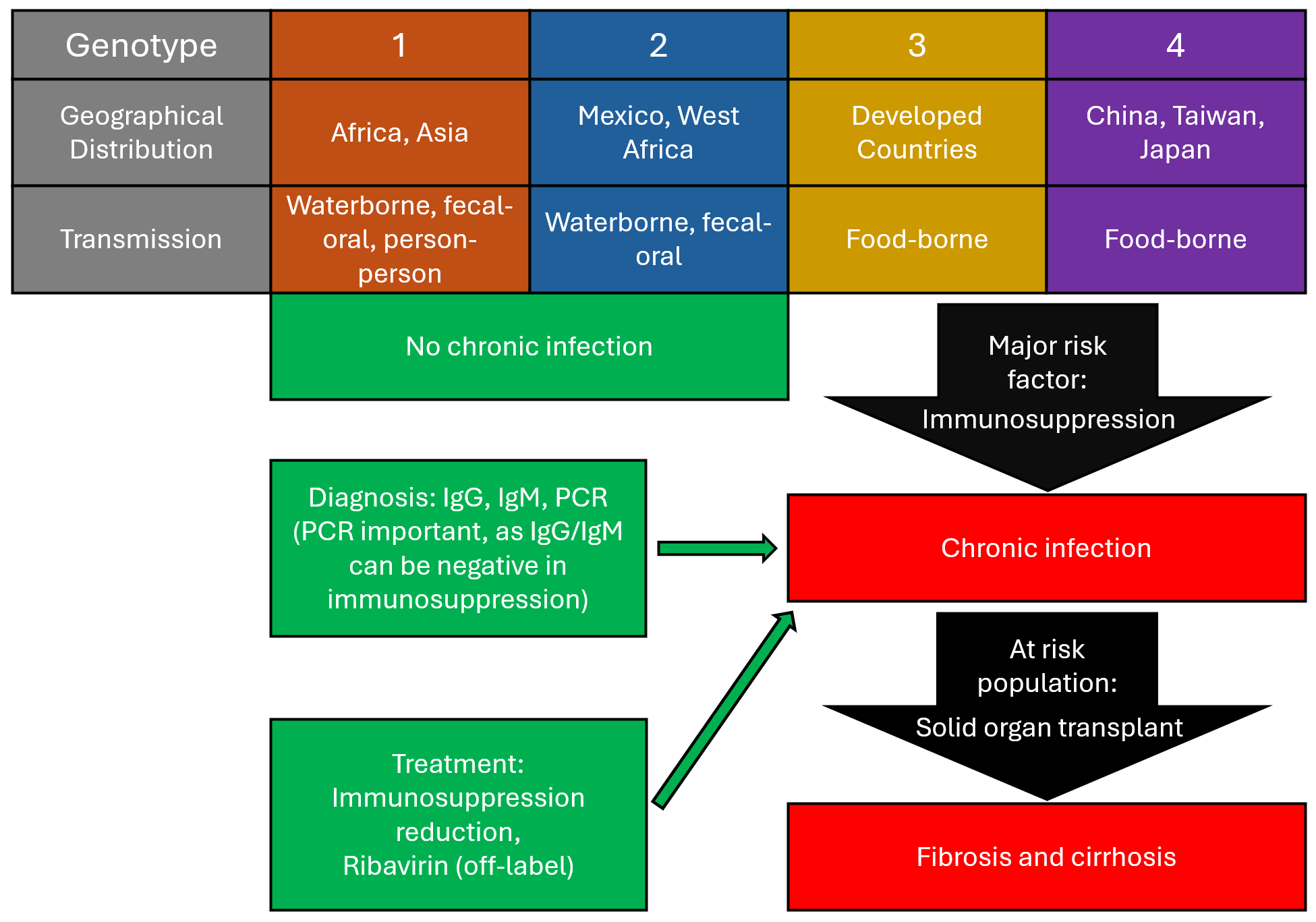
Figure: Figure 1. Summary of hepatitis E genotypes, diagnosis, treatment, and genotype 3/4 progression of disease based on data from Centers for Disease Control and the European Association for the Study of Liver Guidelines from 2018.
Disclosures:
Jenson Phung indicated no relevant financial relationships.
Morgan Freeman indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mary Thomson indicated no relevant financial relationships.
Jenson Phung, MD1, Morgan Freeman, MD1, Rahul Karna, MD2, Mary Thomson, MD, MS1. P3840 - Chronic Hepatitis E Infection: An Insidious Cause of Elevated Transaminases in a Patient with Solid Organ Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


