Monday Poster Session
Category: Liver
P3833 - Not Just Bacteria: A Case of Candida Glabrata Hepatic Abscess Post-Cholecystectomy and Stenting
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Charitha Karanam Ramapathy, MD (she/her/hers)
UAB Montgomery
Montgomery, AL
Presenting Author(s)
Charitha Karanam Ramapathy, MD1, Jayasree Rajapandian, MD2, Mohamad Imam, MD1
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Pyogenic liver abscess being the most common visceral abscess poses a significant mortality and morbidity. Common risk factors include diabetes mellitus, live transplant and biliary tract disease. Liver abscesses can develop because of surgical or penetrating injuries, or through the bloodstream via hematogenous spread. Another significant pathway for abscess formation involves the direct extension of infection from the biliary system. Fungal infections causing hepatic abscesses are very rare especially in an immunocompetent patient. This case highlights that a fungal liver abscess can occur following cholecystectomy, even in patients with a normal immune system.
Case Description/
Methods: Patient is a 53-year-old man who underwent open cholecystectomy 6 weeks ago due to necrosis of gallbladder and was discharged with ciprofloxacin and flagyl. Few days later, he presented with abdominal distension, work up showed biliary leak, underwent Endoscopic retrograde cholangiopancreatography [ERCP] with biliary stent placement and was discharged with the same antibiotics. After few days, he presented with worsening abdomen pain and fever. Vitals on admission were Heart rate 134 beats per minute, Blood pressure 150/90 mmhg, temperature 100.2 F, Respiratory rate 20/minute. Physical exam was remarkable for tenderness on abdominal palpation. CT abdomen and pelvis showed large subcapsular hepatic abscess measuring 17.8x6.6cm, peripherally enhancing fluid collection (Figure 1). Interventional Radiology was consulted and percutaneous drainage of the hepatic abscess was done with 750 ml of output and drain was placed. Cultures grew Candida Glabrata and Streptococcus Intermedius and were treated with IV Ertapenem and Micafungin for a total of 6 weeks. Follow up CT showed resolution of abscess (Figure 2).
Discussion: Candida liver abscesses are extremely rare among patients with normal immune system and without malignancies. Candida species mainly C.albicans, C.glabrata, and C.tropicalis commonly colonize the gastrointestinal tract in a substantial number of healthy individuals. Colonization is noted to be high among hospitalized patients. Our patient grew C. glabrata with likely risk factors including recent surgery, prolonged hospital stay and antibiotic use. when bacterial cultures from a pyogenic abscess are sterile, it is advisable to consider the possibility of a fungal infection among immunocompetent patients, as appropriate antifungal treatment can lead to favorable outcomes.
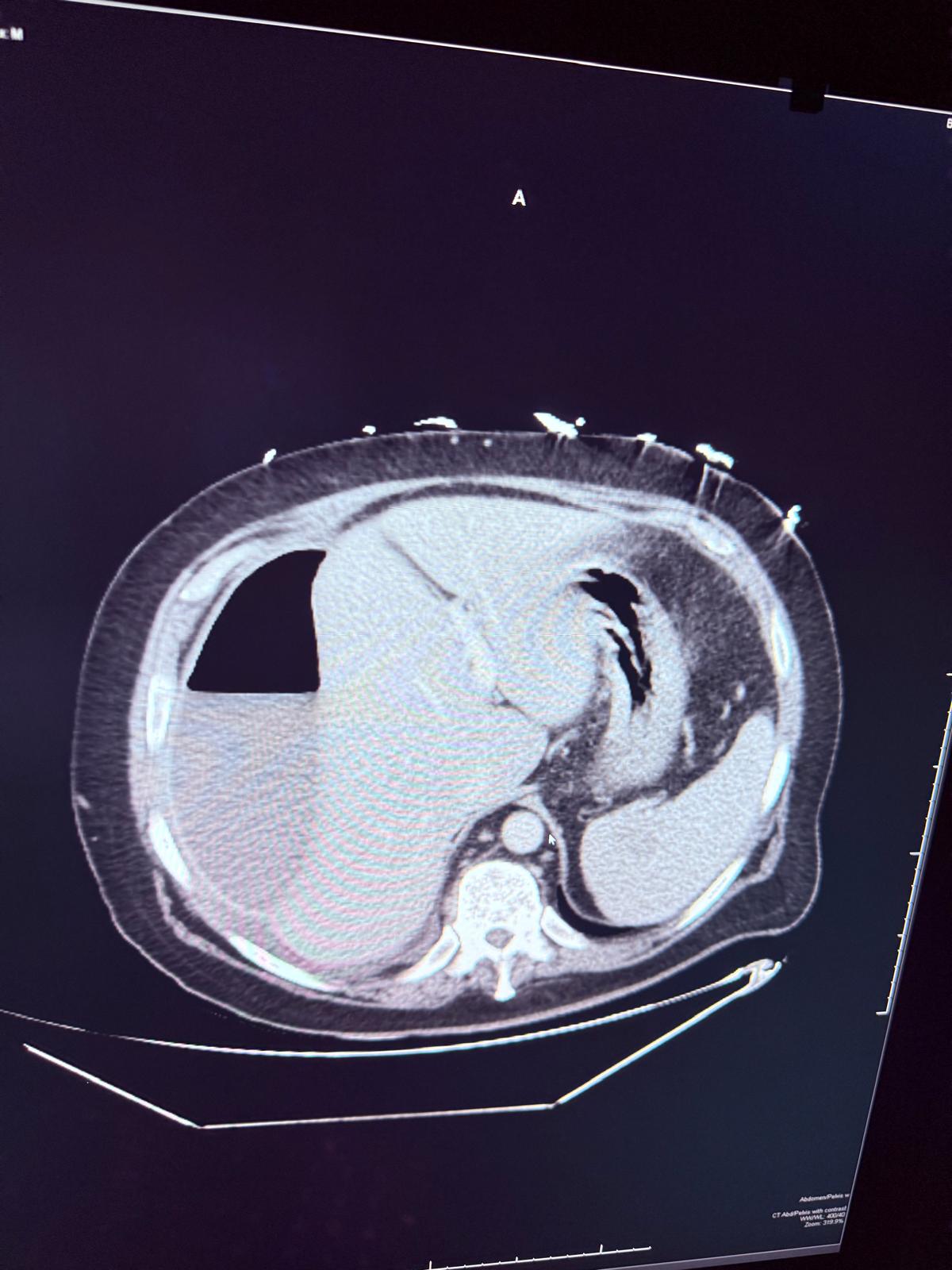
Figure: Figure 1
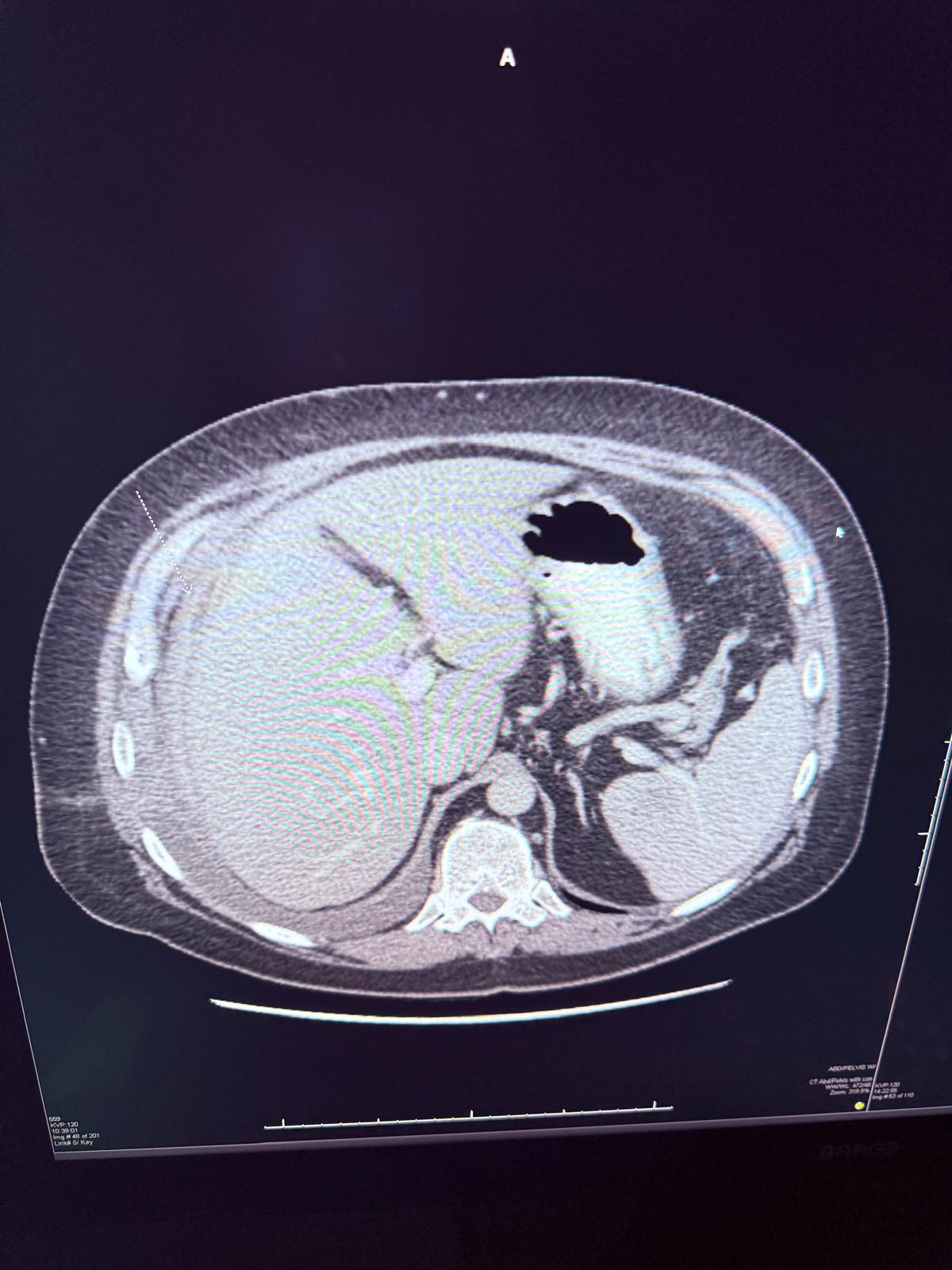
Figure: Figure 2
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Jayasree Rajapandian indicated no relevant financial relationships.
Mohamad Imam indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Jayasree Rajapandian, MD2, Mohamad Imam, MD1. P3833 - Not Just Bacteria: A Case of Candida Glabrata Hepatic Abscess Post-Cholecystectomy and Stenting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Pyogenic liver abscess being the most common visceral abscess poses a significant mortality and morbidity. Common risk factors include diabetes mellitus, live transplant and biliary tract disease. Liver abscesses can develop because of surgical or penetrating injuries, or through the bloodstream via hematogenous spread. Another significant pathway for abscess formation involves the direct extension of infection from the biliary system. Fungal infections causing hepatic abscesses are very rare especially in an immunocompetent patient. This case highlights that a fungal liver abscess can occur following cholecystectomy, even in patients with a normal immune system.
Case Description/
Methods: Patient is a 53-year-old man who underwent open cholecystectomy 6 weeks ago due to necrosis of gallbladder and was discharged with ciprofloxacin and flagyl. Few days later, he presented with abdominal distension, work up showed biliary leak, underwent Endoscopic retrograde cholangiopancreatography [ERCP] with biliary stent placement and was discharged with the same antibiotics. After few days, he presented with worsening abdomen pain and fever. Vitals on admission were Heart rate 134 beats per minute, Blood pressure 150/90 mmhg, temperature 100.2 F, Respiratory rate 20/minute. Physical exam was remarkable for tenderness on abdominal palpation. CT abdomen and pelvis showed large subcapsular hepatic abscess measuring 17.8x6.6cm, peripherally enhancing fluid collection (Figure 1). Interventional Radiology was consulted and percutaneous drainage of the hepatic abscess was done with 750 ml of output and drain was placed. Cultures grew Candida Glabrata and Streptococcus Intermedius and were treated with IV Ertapenem and Micafungin for a total of 6 weeks. Follow up CT showed resolution of abscess (Figure 2).
Discussion: Candida liver abscesses are extremely rare among patients with normal immune system and without malignancies. Candida species mainly C.albicans, C.glabrata, and C.tropicalis commonly colonize the gastrointestinal tract in a substantial number of healthy individuals. Colonization is noted to be high among hospitalized patients. Our patient grew C. glabrata with likely risk factors including recent surgery, prolonged hospital stay and antibiotic use. when bacterial cultures from a pyogenic abscess are sterile, it is advisable to consider the possibility of a fungal infection among immunocompetent patients, as appropriate antifungal treatment can lead to favorable outcomes.
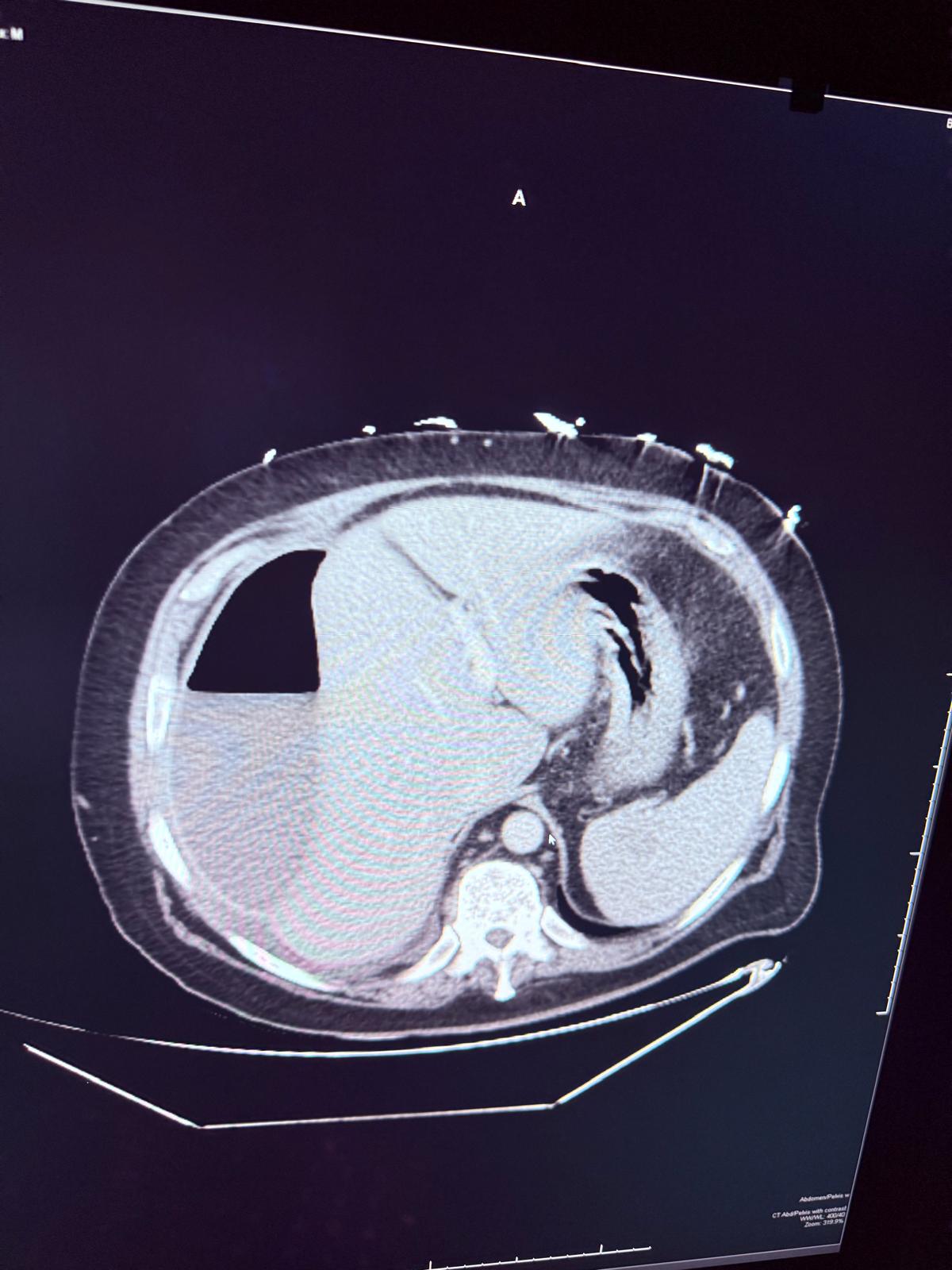
Figure: Figure 1
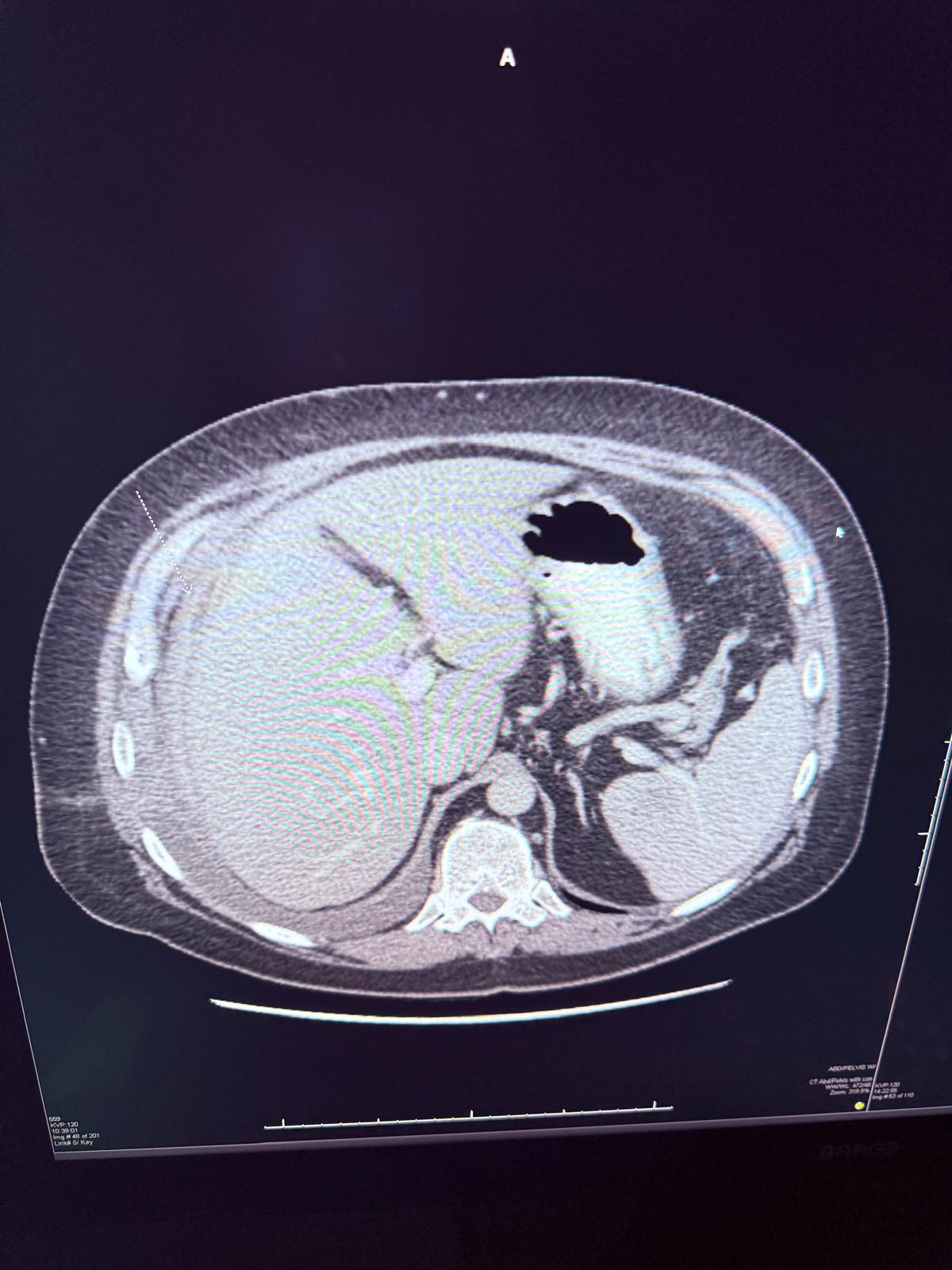
Figure: Figure 2
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Jayasree Rajapandian indicated no relevant financial relationships.
Mohamad Imam indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Jayasree Rajapandian, MD2, Mohamad Imam, MD1. P3833 - Not Just Bacteria: A Case of Candida Glabrata Hepatic Abscess Post-Cholecystectomy and Stenting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
