Monday Poster Session
Category: Liver
P3830 - Clinical Clues and Genetic Views: Unraveling a Diagnostic Journey to Birt–Hogg–Dubé Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Geraldine Nabeta, MD, MS (she/her/hers)
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Geraldine Nabeta, MD, MS1, Muhammad M.. Kamal, MD1, Karthik Mathialagan, MD2, Elizabeth Richardson, DO3
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT
Introduction: Birt-Hogg-Dube syndrome (BHDS), an exceedingly rare syndrome, is characterized by an autosomal dominant mutation in the tumor suppressor gene, Folliculin (FLCN). Although the pathophysiology is poorly understood, patients with BHDS are prone to various disease manifestations. Most are cutaneous, such as lipomas and fibrofolliculomas, and lung cysts with increased risk for pneumothoraces. Patients are also susceptible to renal tumors and possibly other cancers, though this literature is scarce.
Case Description/
Methods: Here we present a case of how a 60-year-old male with a presumed benign liver lesion and no known family history of hereditary disease led to a diagnosis of BHDS. Past medical history includes chronic liver disease without fibrosis, pulmonary cysts without emphysematous changes, treated HCV with SVR, and adrenocortical adenoma s/p adrenalectomy. He initially presented with complaints of neuropathy, bilateral lower extremity edema, and gynecomastia. On exam he had multiple lipomas and facial pearly papules resembling fibrofolliculomas. Workup revealed a 3 cm liver mass, however initial biopsy was nondiagnostic. His symptoms progressed with acute-on-chronic back pain, prompting repeat FDG-PET/CT. Imaging revealed a lytic lesion at T4 biopsied as metastatic undifferentiated carcinoma. Repeat abdominal imaging revealed an incremental increase in the liver lesion, 4.4 cm. A subsequent biopsy reported perivascular epithelioid cell tumor (PEComa), however further review of the pathology was consistent with adrenal adenocarcinoma. Given his skin lesions, neoplasms, and pulmonary cysts, there was suspicion of a cancer predisposition syndrome. Genetic testing confirmed a germline mutation in Folliculin (FLCN), consistent with BHDS. The patient was started on radiation therapy with plans to begin chemotherapy.
Discussion: This is a challenging case that highlights the variability in presentation in a patient with no known family history of BHDS. His skin changes, pulmonary cysts, and a liver mass initially misdiagnosed as PEComa, led to the identification of a pathologic FLCN mutation. Neoplasms associated with BHDS are commonly renal cancers, though PEComas or adrenal adenocarcinoma can also be considered. This case reinforces the significance of maintaining high suspicion for hereditary cancer syndromes in patients with visibly unrelated benign and malignant lesions. Early diagnosis of BHDS is instrumental for appropriate surveillance, intervention, and genetic testing in family members.
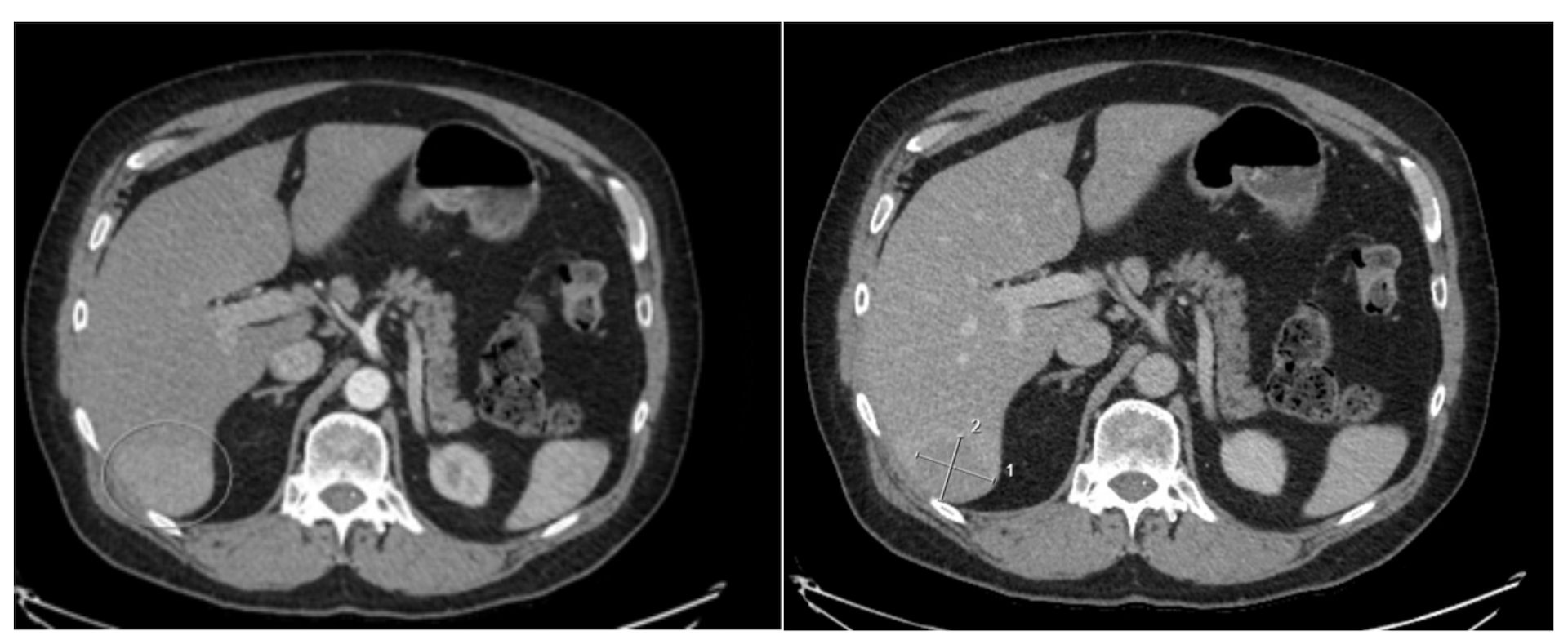
Figure: Figure 1: Rounded lesion in right hepatic segment 6/7, measuring 4.4 x 3.7 cm, which demonstrates nonperipheral arterial hyperenhancement and delayed phase washout
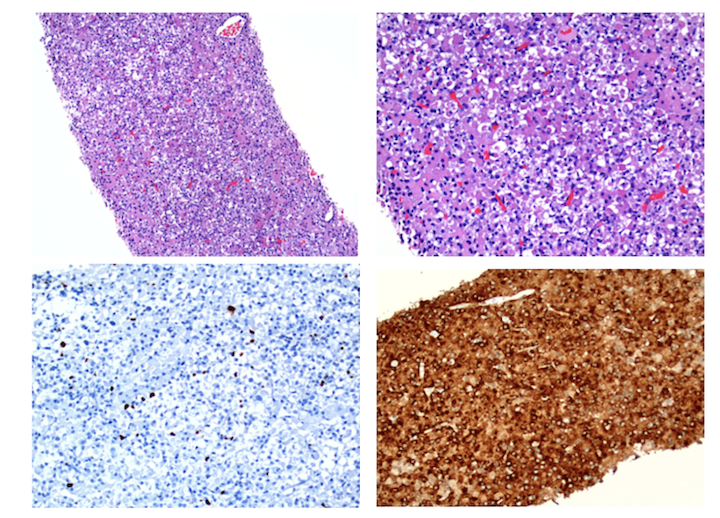
Figure: Figure 2: Immunohistochemistry and H&E staining of liver mass. Ki-67 indicating low proliferation index (bottom left ) . Cathepsin K staining positive (bottom right).
Disclosures:
Geraldine Nabeta indicated no relevant financial relationships.
Muhammad Kamal indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Elizabeth Richardson indicated no relevant financial relationships.
Geraldine Nabeta, MD, MS1, Muhammad M.. Kamal, MD1, Karthik Mathialagan, MD2, Elizabeth Richardson, DO3. P3830 - Clinical Clues and Genetic Views: Unraveling a Diagnostic Journey to Birt–Hogg–Dubé Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Hospital, Hartford, CT
Introduction: Birt-Hogg-Dube syndrome (BHDS), an exceedingly rare syndrome, is characterized by an autosomal dominant mutation in the tumor suppressor gene, Folliculin (FLCN). Although the pathophysiology is poorly understood, patients with BHDS are prone to various disease manifestations. Most are cutaneous, such as lipomas and fibrofolliculomas, and lung cysts with increased risk for pneumothoraces. Patients are also susceptible to renal tumors and possibly other cancers, though this literature is scarce.
Case Description/
Methods: Here we present a case of how a 60-year-old male with a presumed benign liver lesion and no known family history of hereditary disease led to a diagnosis of BHDS. Past medical history includes chronic liver disease without fibrosis, pulmonary cysts without emphysematous changes, treated HCV with SVR, and adrenocortical adenoma s/p adrenalectomy. He initially presented with complaints of neuropathy, bilateral lower extremity edema, and gynecomastia. On exam he had multiple lipomas and facial pearly papules resembling fibrofolliculomas. Workup revealed a 3 cm liver mass, however initial biopsy was nondiagnostic. His symptoms progressed with acute-on-chronic back pain, prompting repeat FDG-PET/CT. Imaging revealed a lytic lesion at T4 biopsied as metastatic undifferentiated carcinoma. Repeat abdominal imaging revealed an incremental increase in the liver lesion, 4.4 cm. A subsequent biopsy reported perivascular epithelioid cell tumor (PEComa), however further review of the pathology was consistent with adrenal adenocarcinoma. Given his skin lesions, neoplasms, and pulmonary cysts, there was suspicion of a cancer predisposition syndrome. Genetic testing confirmed a germline mutation in Folliculin (FLCN), consistent with BHDS. The patient was started on radiation therapy with plans to begin chemotherapy.
Discussion: This is a challenging case that highlights the variability in presentation in a patient with no known family history of BHDS. His skin changes, pulmonary cysts, and a liver mass initially misdiagnosed as PEComa, led to the identification of a pathologic FLCN mutation. Neoplasms associated with BHDS are commonly renal cancers, though PEComas or adrenal adenocarcinoma can also be considered. This case reinforces the significance of maintaining high suspicion for hereditary cancer syndromes in patients with visibly unrelated benign and malignant lesions. Early diagnosis of BHDS is instrumental for appropriate surveillance, intervention, and genetic testing in family members.
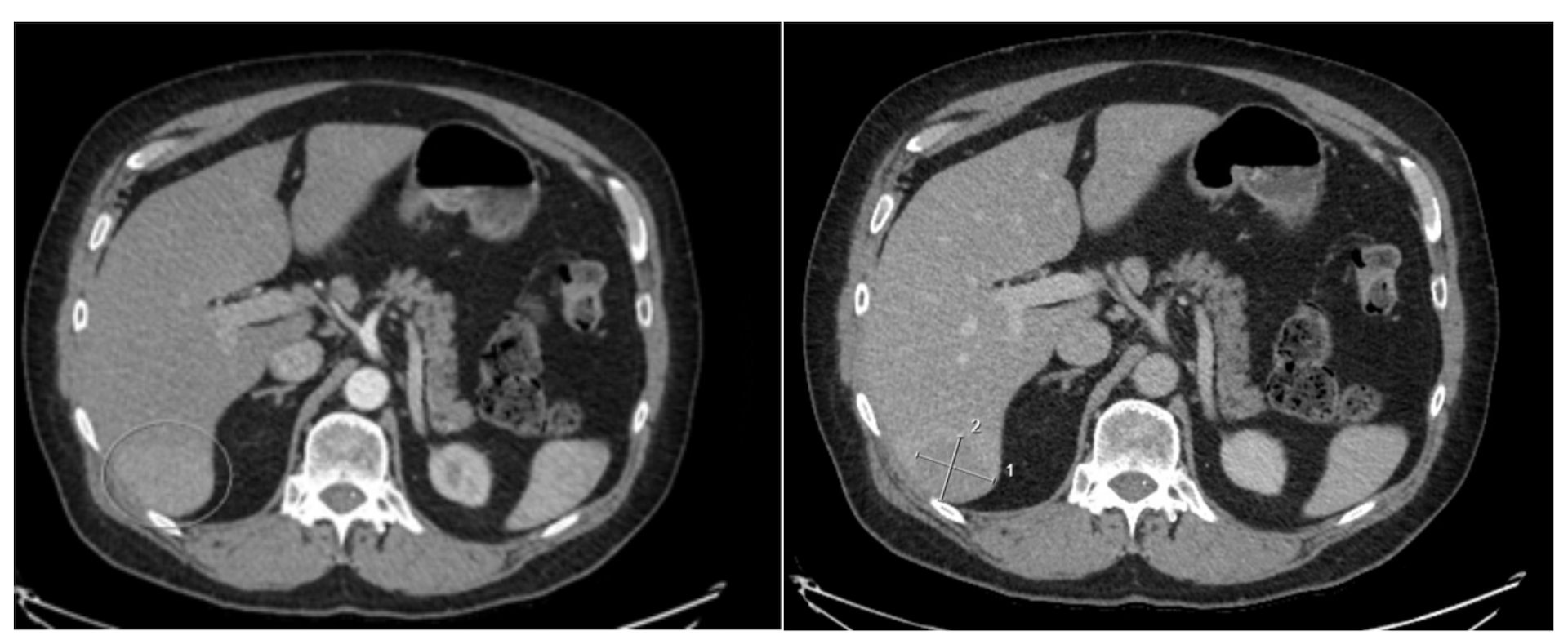
Figure: Figure 1: Rounded lesion in right hepatic segment 6/7, measuring 4.4 x 3.7 cm, which demonstrates nonperipheral arterial hyperenhancement and delayed phase washout
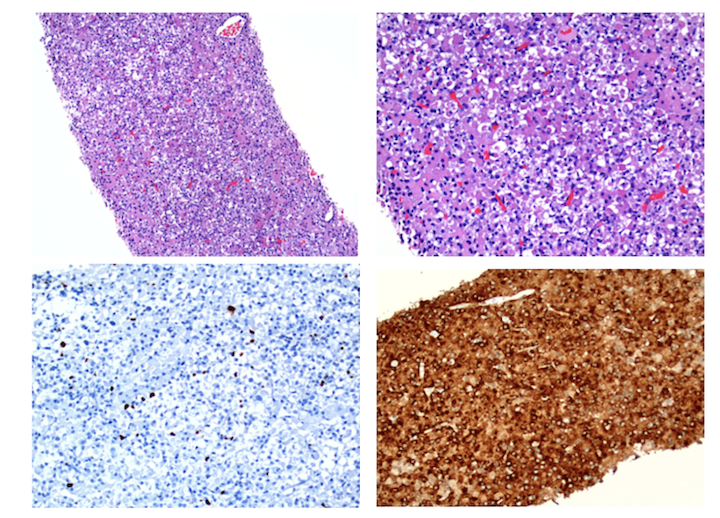
Figure: Figure 2: Immunohistochemistry and H&E staining of liver mass. Ki-67 indicating low proliferation index (bottom left ) . Cathepsin K staining positive (bottom right).
Disclosures:
Geraldine Nabeta indicated no relevant financial relationships.
Muhammad Kamal indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Elizabeth Richardson indicated no relevant financial relationships.
Geraldine Nabeta, MD, MS1, Muhammad M.. Kamal, MD1, Karthik Mathialagan, MD2, Elizabeth Richardson, DO3. P3830 - Clinical Clues and Genetic Views: Unraveling a Diagnostic Journey to Birt–Hogg–Dubé Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
