Monday Poster Session
Category: Liver
P3826 - Checkpoint and Checkmate: Concurrent Immune-Mediated Hepatitis and HBV Reactivation in a Cancer Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Emmanuel Boateng, MD (he/him/his)
University of California Davis Health
Seattle, WA
Presenting Author(s)
Emmanuel Boateng, MD1, Hannah Chi, MD2, Naima Hashi, MD2, Lindsay Sobotka, DO2, Vivek Mendiratta, MD3
1University of California Davis Health, Sacramento, CA; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University Wexner Medical Center, Dublin, OH
Introduction: With the expanding use of immune checkpoint inhibitors (ICI), there has been a notable rise in immune-related adverse events, including ICI hepatitis, a potentially severe and under-recognized etiology of liver injury. Furthermore, Hepatitis B reactivation is a rare
but potentially life-threatening complication that can emerge unexpectedly in patients receiving ICI therapy. We present a unique case of a patient with acute liver injury due to both reactivated hepatitis B and ICI hepatitis.
Case Description/
Methods: A 42-year-old Kenyan female with metastatic renal cell carcinoma (RCC) presented to the hospital with worsening abdominal pain. She was receiving Pembrolizumab and Lenvatinib for her RCC. Labs revealed elevated AST 800, ALT 312, ALP 237, and INR 1.5. Physical exam was pertinent for diffusely tender abdomen. Serologies showed a positive hepatitis B core antibody, hepatitis B surface antigen, and PCR >10 million. She was started on treatment for hepatitis B reactivation with Tenofovir and N-Acetylcysteine (NAC). The patient’s LFTs continued to rise despite treatment and hence underwent endoscopic ultrasound-guided liver biopsy. Pathology revealed injury from both ICI therapy (Figure 1) and HBV (Figure 2). After a multidisciplinary discussion, she was initiated on Solumedrol 1 g/kg in addition to continuing her Tenofovir. Thereafter, the patient’s LFTs and INR rapidly improved, and she was transitioned to oral prednisone taper. Labs 3 months later showed normalization of her LFTs, and labs 6 months later showed her HBV DNA was undetectable.
Discussion: The diagnosis of ICI-induced hepatitis is a diagnosis of exclusion and while histopathology is not required, liver biopsy is essential in cases of diagnostic uncertainty or treatment of refractory hepatitis. When diagnosed, treatment for ICI-induced hepatitis includes holding therapy for grade 2 and above injury and initiation of corticosteroids for persistent or severe cases. The challenge in this case was that the patient needed steroids to manage the immune-mediated liver damage caused by ICI therapy, but using steroids also risked enhancing viral replication and potentially leading to additional liver injury. Patients with undiagnosed hepatitis B are at increased risk of developing fulminant liver failure. Therefore, it is imperative to check hepatitis B serologies before immunosuppression and initiate antiviral prophylaxis when indicated. Unfortunately, our patient did not have her serologies checked before starting treatment.
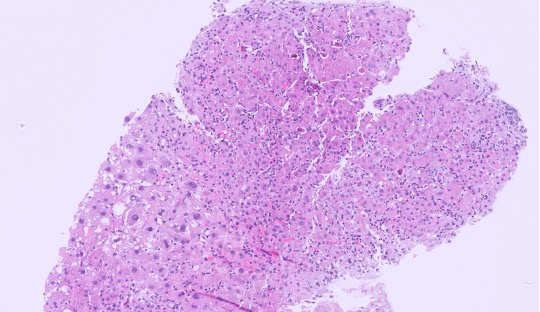
Figure: Figure 1, H&E image showing acute hepatitis pattern of injury with lobular disarray, inflammation, hepatocyte swelling, and many acidophil bodies
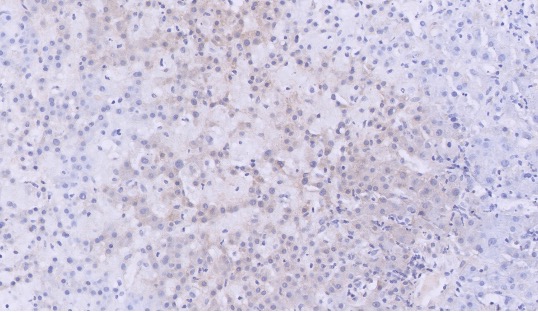
Figure: Figure 2, Hepatitis B stain image showing the positive staining for hepatitis B (brown color in the hepatocytes)
Disclosures:
Emmanuel Boateng indicated no relevant financial relationships.
Hannah Chi indicated no relevant financial relationships.
Naima Hashi indicated no relevant financial relationships.
Lindsay Sobotka indicated no relevant financial relationships.
Vivek Mendiratta indicated no relevant financial relationships.
Emmanuel Boateng, MD1, Hannah Chi, MD2, Naima Hashi, MD2, Lindsay Sobotka, DO2, Vivek Mendiratta, MD3. P3826 - Checkpoint and Checkmate: Concurrent Immune-Mediated Hepatitis and HBV Reactivation in a Cancer Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Davis Health, Sacramento, CA; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University Wexner Medical Center, Dublin, OH
Introduction: With the expanding use of immune checkpoint inhibitors (ICI), there has been a notable rise in immune-related adverse events, including ICI hepatitis, a potentially severe and under-recognized etiology of liver injury. Furthermore, Hepatitis B reactivation is a rare
but potentially life-threatening complication that can emerge unexpectedly in patients receiving ICI therapy. We present a unique case of a patient with acute liver injury due to both reactivated hepatitis B and ICI hepatitis.
Case Description/
Methods: A 42-year-old Kenyan female with metastatic renal cell carcinoma (RCC) presented to the hospital with worsening abdominal pain. She was receiving Pembrolizumab and Lenvatinib for her RCC. Labs revealed elevated AST 800, ALT 312, ALP 237, and INR 1.5. Physical exam was pertinent for diffusely tender abdomen. Serologies showed a positive hepatitis B core antibody, hepatitis B surface antigen, and PCR >10 million. She was started on treatment for hepatitis B reactivation with Tenofovir and N-Acetylcysteine (NAC). The patient’s LFTs continued to rise despite treatment and hence underwent endoscopic ultrasound-guided liver biopsy. Pathology revealed injury from both ICI therapy (Figure 1) and HBV (Figure 2). After a multidisciplinary discussion, she was initiated on Solumedrol 1 g/kg in addition to continuing her Tenofovir. Thereafter, the patient’s LFTs and INR rapidly improved, and she was transitioned to oral prednisone taper. Labs 3 months later showed normalization of her LFTs, and labs 6 months later showed her HBV DNA was undetectable.
Discussion: The diagnosis of ICI-induced hepatitis is a diagnosis of exclusion and while histopathology is not required, liver biopsy is essential in cases of diagnostic uncertainty or treatment of refractory hepatitis. When diagnosed, treatment for ICI-induced hepatitis includes holding therapy for grade 2 and above injury and initiation of corticosteroids for persistent or severe cases. The challenge in this case was that the patient needed steroids to manage the immune-mediated liver damage caused by ICI therapy, but using steroids also risked enhancing viral replication and potentially leading to additional liver injury. Patients with undiagnosed hepatitis B are at increased risk of developing fulminant liver failure. Therefore, it is imperative to check hepatitis B serologies before immunosuppression and initiate antiviral prophylaxis when indicated. Unfortunately, our patient did not have her serologies checked before starting treatment.
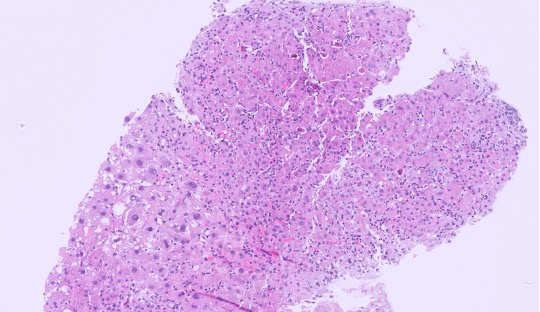
Figure: Figure 1, H&E image showing acute hepatitis pattern of injury with lobular disarray, inflammation, hepatocyte swelling, and many acidophil bodies
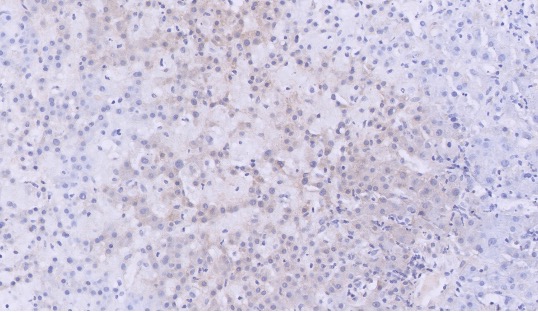
Figure: Figure 2, Hepatitis B stain image showing the positive staining for hepatitis B (brown color in the hepatocytes)
Disclosures:
Emmanuel Boateng indicated no relevant financial relationships.
Hannah Chi indicated no relevant financial relationships.
Naima Hashi indicated no relevant financial relationships.
Lindsay Sobotka indicated no relevant financial relationships.
Vivek Mendiratta indicated no relevant financial relationships.
Emmanuel Boateng, MD1, Hannah Chi, MD2, Naima Hashi, MD2, Lindsay Sobotka, DO2, Vivek Mendiratta, MD3. P3826 - Checkpoint and Checkmate: Concurrent Immune-Mediated Hepatitis and HBV Reactivation in a Cancer Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
