Monday Poster Session
Category: Liver
P3798 - Vonoprazan Is Associated With a Lower Risk of Infections, Hospitalizations, and Death Compared to PPIs in Patients With Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JB
Jasmohan S. Bajaj, MD, MS, FACG
Virginia Commonwealth University; Central Virginia Veterans Healthcare System
Richmond, VA
Presenting Author(s)
Nilang Patel, MD1, Scott Silvey, MS1, Jasmohan S.. Bajaj, MD, MS, FACG2
1Virginia Commonwealth University School of Medicine and Richmond VA Medical Center, Richmond, VA; 2Virginia Commonwealth University; Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Acid suppression with proton pump inhibitors (PPI) is linked with infections & poor outcomes in cirrhosis. Potassium competitive acid blockers (PCAB) have been introduced as alternatives.
Aim: compare PCABs vs PPIs in predicting outcomes in cirrhosis
Methods: Using TriNetX, we created a cohort of cirrhosis patients using validated ICD-9/10 codes between Jan 2018 to Dec 2024 who were started on PPI or PCAB (Vonoprazan) after cirrhosis diagnosis. Demographics, comorbidities, cirrhosis severity labs closest to the index PPI/vonoprazan prescription dates were chosen. To address the differences in baseline characteristics between the two groups, we extracted demographic variables such as age, sex, race, and ethnicity, comorbidities and concurrent medication use within 2 years before the index date. The laboratory tests analyzed in this study included MELD-Na labs and blood counts; closest labs from the index date were selected.
Outcomes: Primary outcome was 6 month post-index date mortality, while infections and all-cause hospitalizations were secondary outcomes. 1-year outcomes were also evaluated. Univariate analysis performed and crude estimate of odds ratio of outcomes were reported. Adjusted hazard ratios (AHRs) with 95% CIs and P values were calculated using Cox proportional hazards regression models for all outcomes. Kaplan-Meier curves for outcomes were created.
Results: 19,273 cirrhosis patients (63.9±13.8 yrs, 66% men) were included. Most (89%, n=17.285) were on PPI while the rest (11% n=1988) were on vonoprazan. The median follow up was 180 (IQR 117 days). Fig 1 shows PPI users were older, and more male. PCAB users had higher cardiovascular disorders & GERD. Cirrhosis variables showed lower alcohol, higher HE with lactulose & rifaximin, & SBP with higher propranolol in PPI gp. Lower platelets, worse MELD score variables were seen in PPI but albumin was higher than PCABs.
Cox proportional hazards (Fig 2A) shows lower rate of all outcomes at 6 & 12 months with vonoprazan versus PPIs which remained significant on adjusted comparisons. Kaplan Meier curves showed significant separation between vonoprazan & PPIs for all outcomes (Fig 2B).
Discussion: In patients with cirrhosis there was a lower risk of infections, all-cause hospitalizations, & trend towards lower death at 6 & 12 months post-medication initiation date with vonoprazan compared to PPIs despite controlling for demographics, cirrhosis severity, and comorbid conditions. PCAB use in cirrhosis could be considered instead of PPIs.
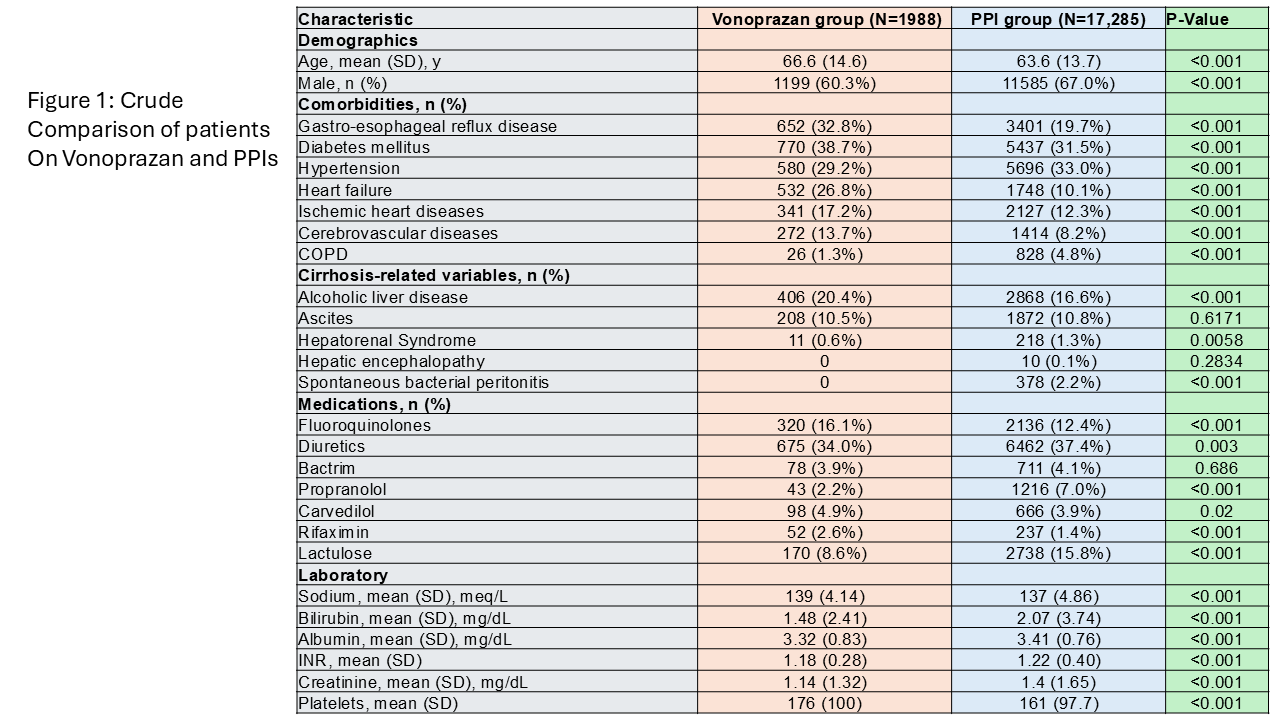
Figure: Crude Comparisons Between PPIs and Vonoprazan groups
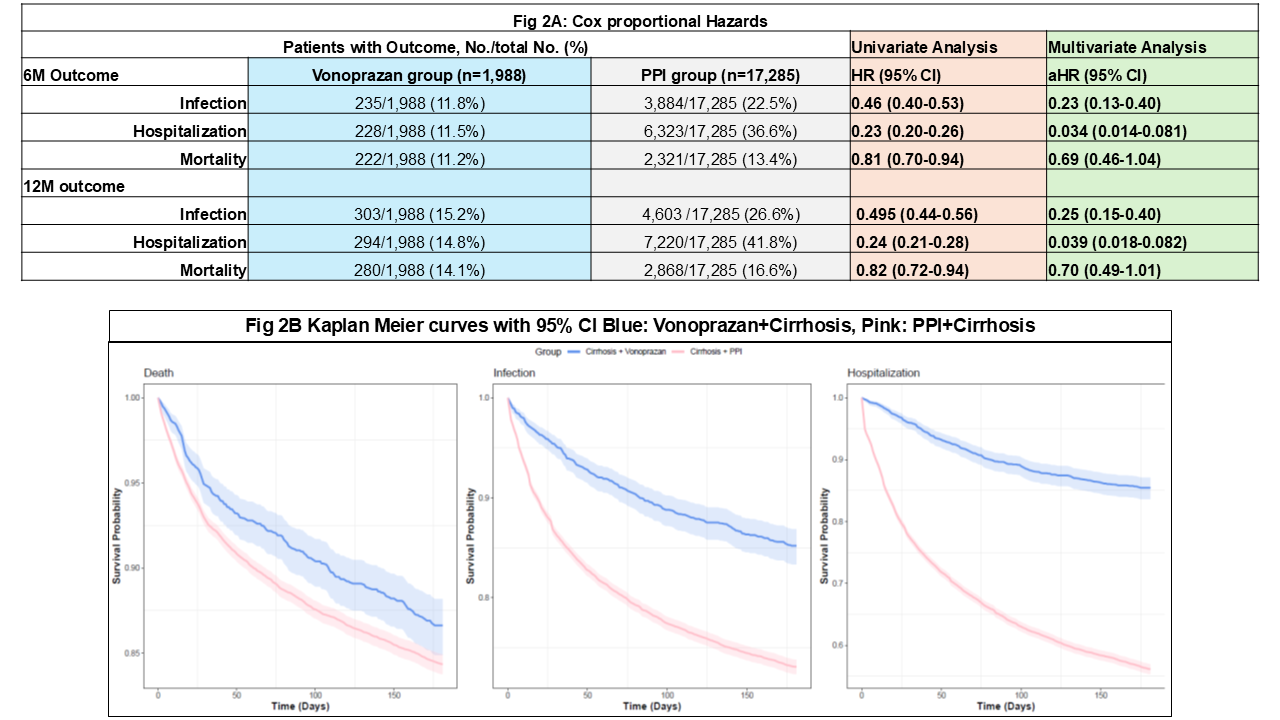
Figure: Cox Proportional Hazards and Kaplan Meier Curves Showing Significantly Lower rate of Infections, All-cause Hospitalizations, and trend towards lower Death in Vonoprazan compared to PPI group
Disclosures:
Nilang Patel indicated no relevant financial relationships.
Scott Silvey indicated no relevant financial relationships.
Jasmohan Bajaj: Bausch – Grant/Research Support. Genfit – Grant/Research Support. Salix Pharmaceuticals – Clinical trial investigator. Sequana – Grant/Research Support.
Nilang Patel, MD1, Scott Silvey, MS1, Jasmohan S.. Bajaj, MD, MS, FACG2. P3798 - Vonoprazan Is Associated With a Lower Risk of Infections, Hospitalizations, and Death Compared to PPIs in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University School of Medicine and Richmond VA Medical Center, Richmond, VA; 2Virginia Commonwealth University; Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Acid suppression with proton pump inhibitors (PPI) is linked with infections & poor outcomes in cirrhosis. Potassium competitive acid blockers (PCAB) have been introduced as alternatives.
Aim: compare PCABs vs PPIs in predicting outcomes in cirrhosis
Methods: Using TriNetX, we created a cohort of cirrhosis patients using validated ICD-9/10 codes between Jan 2018 to Dec 2024 who were started on PPI or PCAB (Vonoprazan) after cirrhosis diagnosis. Demographics, comorbidities, cirrhosis severity labs closest to the index PPI/vonoprazan prescription dates were chosen. To address the differences in baseline characteristics between the two groups, we extracted demographic variables such as age, sex, race, and ethnicity, comorbidities and concurrent medication use within 2 years before the index date. The laboratory tests analyzed in this study included MELD-Na labs and blood counts; closest labs from the index date were selected.
Outcomes: Primary outcome was 6 month post-index date mortality, while infections and all-cause hospitalizations were secondary outcomes. 1-year outcomes were also evaluated. Univariate analysis performed and crude estimate of odds ratio of outcomes were reported. Adjusted hazard ratios (AHRs) with 95% CIs and P values were calculated using Cox proportional hazards regression models for all outcomes. Kaplan-Meier curves for outcomes were created.
Results: 19,273 cirrhosis patients (63.9±13.8 yrs, 66% men) were included. Most (89%, n=17.285) were on PPI while the rest (11% n=1988) were on vonoprazan. The median follow up was 180 (IQR 117 days). Fig 1 shows PPI users were older, and more male. PCAB users had higher cardiovascular disorders & GERD. Cirrhosis variables showed lower alcohol, higher HE with lactulose & rifaximin, & SBP with higher propranolol in PPI gp. Lower platelets, worse MELD score variables were seen in PPI but albumin was higher than PCABs.
Cox proportional hazards (Fig 2A) shows lower rate of all outcomes at 6 & 12 months with vonoprazan versus PPIs which remained significant on adjusted comparisons. Kaplan Meier curves showed significant separation between vonoprazan & PPIs for all outcomes (Fig 2B).
Discussion: In patients with cirrhosis there was a lower risk of infections, all-cause hospitalizations, & trend towards lower death at 6 & 12 months post-medication initiation date with vonoprazan compared to PPIs despite controlling for demographics, cirrhosis severity, and comorbid conditions. PCAB use in cirrhosis could be considered instead of PPIs.
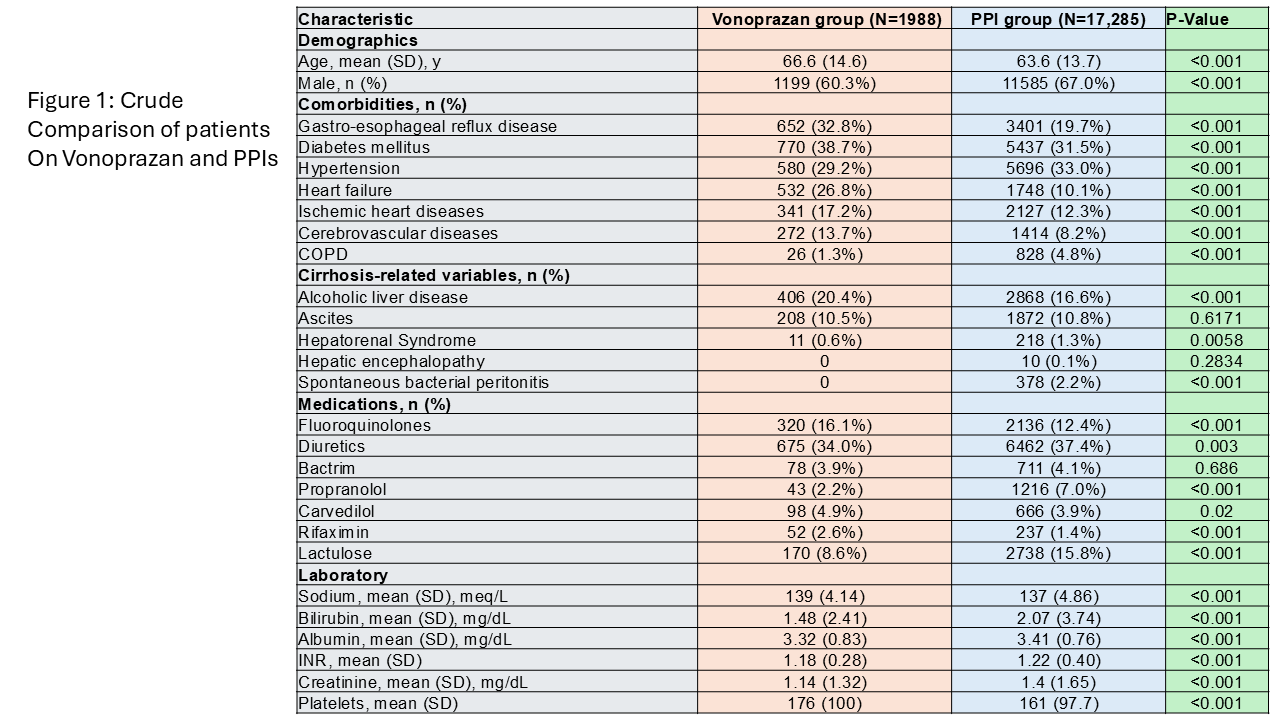
Figure: Crude Comparisons Between PPIs and Vonoprazan groups
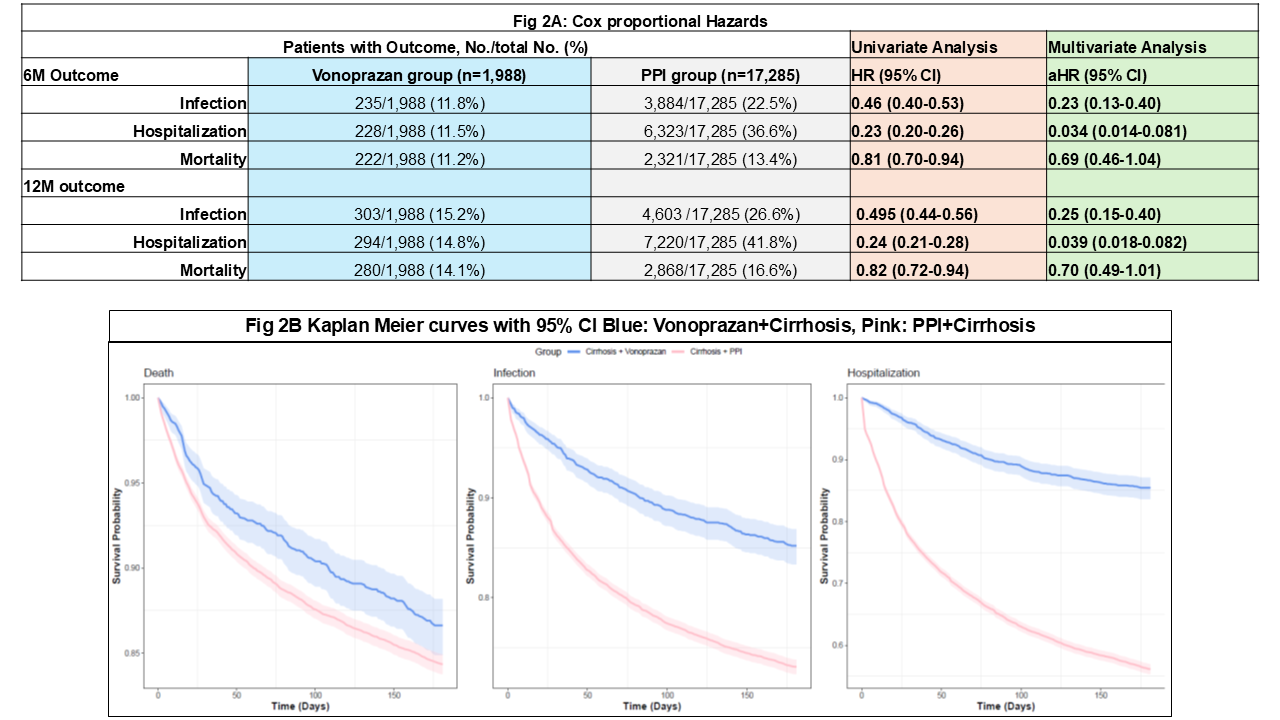
Figure: Cox Proportional Hazards and Kaplan Meier Curves Showing Significantly Lower rate of Infections, All-cause Hospitalizations, and trend towards lower Death in Vonoprazan compared to PPI group
Disclosures:
Nilang Patel indicated no relevant financial relationships.
Scott Silvey indicated no relevant financial relationships.
Jasmohan Bajaj: Bausch – Grant/Research Support. Genfit – Grant/Research Support. Salix Pharmaceuticals – Clinical trial investigator. Sequana – Grant/Research Support.
Nilang Patel, MD1, Scott Silvey, MS1, Jasmohan S.. Bajaj, MD, MS, FACG2. P3798 - Vonoprazan Is Associated With a Lower Risk of Infections, Hospitalizations, and Death Compared to PPIs in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
